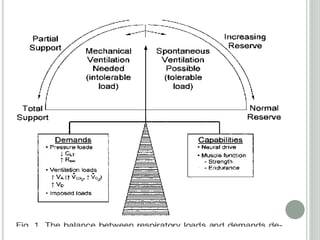
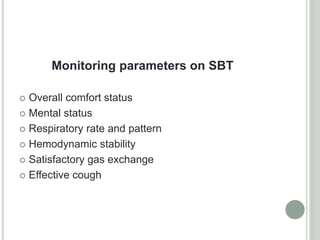
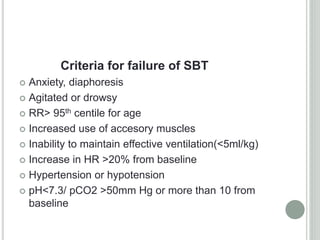
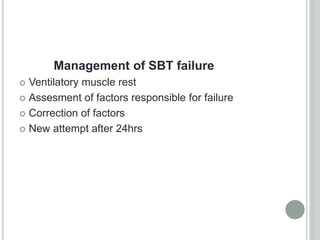
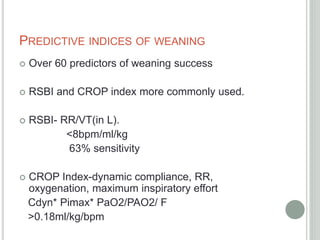
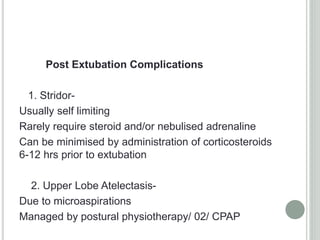
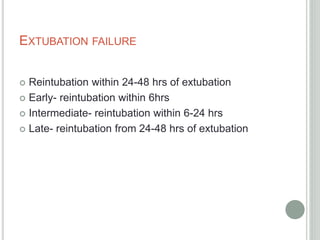
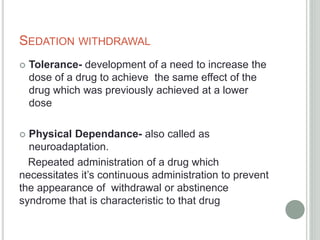
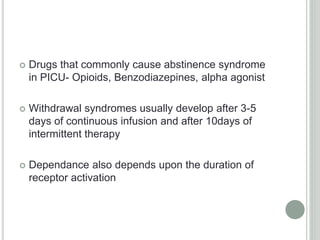
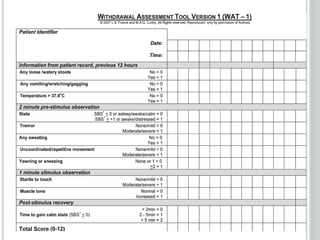
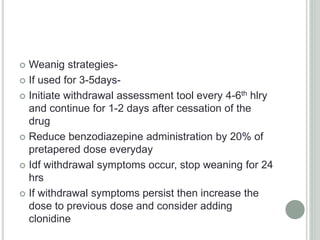
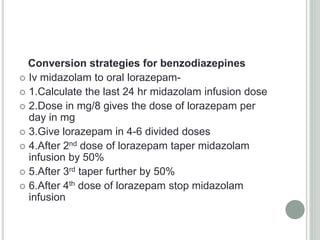
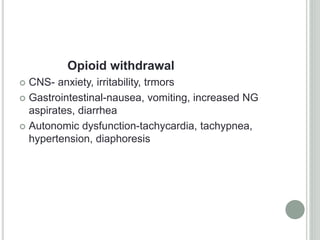
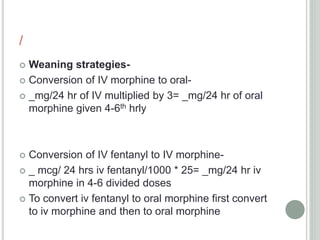
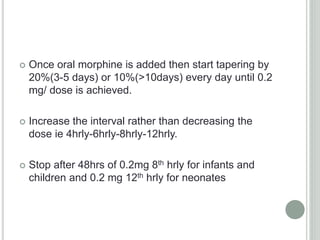
The document discusses the processes of weaning and extubation in pediatric intensive care, outlining techniques for determination of weaning readiness, sedation withdrawal management, and predictive indices for successful weaning. It emphasizes the importance of monitoring during spontaneous breathing trials, recognizing extubation feasibility, and managing sedation withdrawal symptoms, which may arise from opioid and benzodiazepine usage. Various strategies for managing withdrawal, including tapering of medications, are also detailed, along with the assessment tools to evaluate the patient's response.