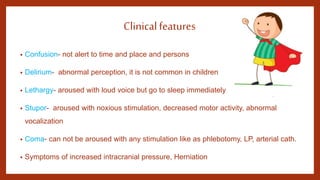
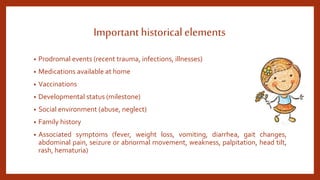
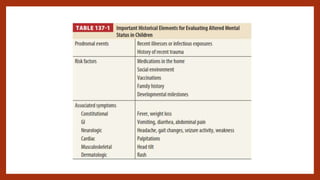
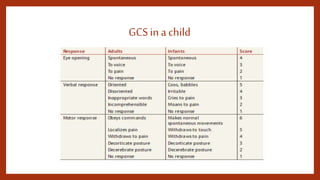
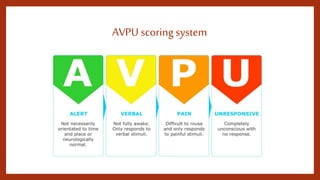
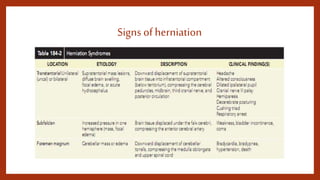
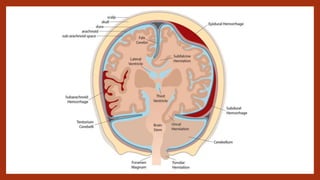
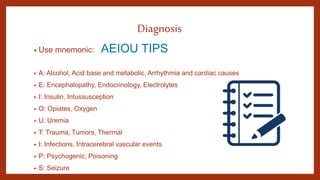
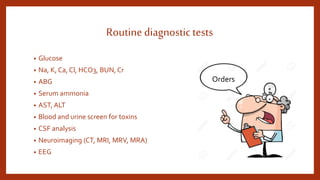
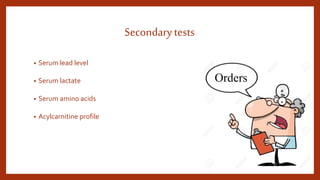
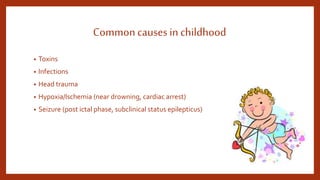
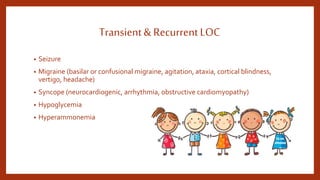
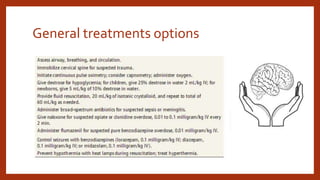
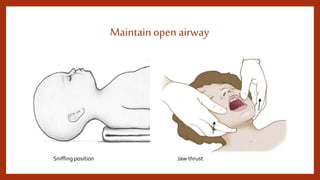
The document discusses altered mental status in children, highlighting the importance of simultaneous stabilization, diagnosis, and treatment to prevent irreversible brain damage. It outlines the pathophysiology, clinical features, historical elements, physical examination, diagnostic tests, and common causes, emphasizing the need for thorough evaluation and appropriate management. Treatment options include maintaining an open airway and addressing reversible causes, with follow-up care essential for discharged patients.