This document provides information on meningitis, including:
- Meningitis is an inflammation of the meninges (membranes covering the brain and spinal cord) that can be caused by bacteria, viruses, fungi, or other causes.
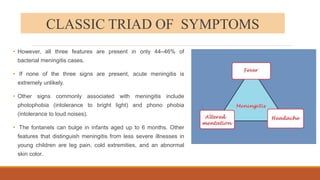
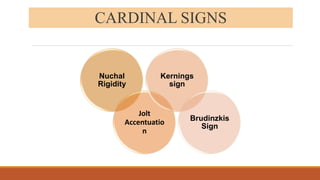
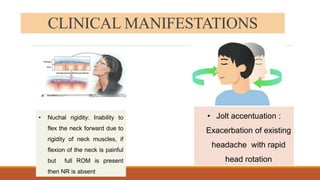
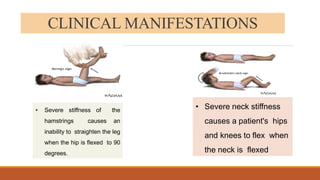
- Common symptoms include fever, headache, and neck stiffness.
- Bacterial meningitis requires immediate treatment with antibiotics to prevent disability or death. Viral meningitis is generally less severe but still requires supportive care.
- Complications can include hearing loss, seizures, learning difficulties, and even death if not properly treated.