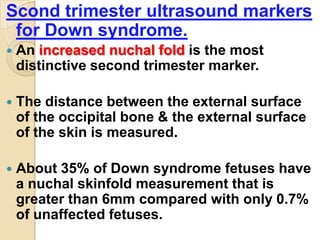
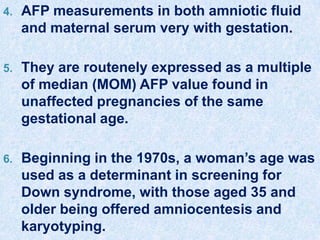
This document discusses maternal serum screening, which analyzes various biomarkers in a pregnant woman's blood to assess risk for fetal abnormalities. It began in the 1970s with alpha-fetoprotein screening for neural tube defects. Additional markers like human chorionic gonadotropin and unconjugated estriol were later added, improving detection rates for Down syndrome. Today's standard screening incorporates these "triple markers" along with inhibin A in a "quad screen". Newer tests analyze markers in the first trimester like pregnancy-associated plasma protein A and nuchal translucency ultrasound to provide very early screening. Positive screens may warrant diagnostic testing via amniocentesis or ultrasound.
![•Second trimester biochemical screening[BCS] started
in the 1970’s when it was found that fetal neural tube
defects[NTD’s] were associated with increase in
maternal serum alpha feto protein[MSAFP].
•Such measurements were offered to pregnant woman
for screening purposes.
•While the screening protocols for NTD’s were being
refined, it was noted that MSAFP tended to be low in
fetal down’s syndrome.
•With a cut off of 2.0 multiples of median[MOM] 85% of
NTD’s would be screened in & with a threshold of 0.5
MOM approx 33% of DS fetus would be screened in.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-2-320.jpg)
![ With the addition of two other analytes
Estriol [which is low in DS] & Human
chorionic gonadotropin[hCG] [which is
increased in DS] the sensitivity of
biochemical screening for DS rose to
approx 65% across all ages & was over 85%
in those above 35 years of age.
The most recent addition to the biochemical
screening regimen taking the above “Triple
screen” to “Quad screen” is inhibin A.
This increases the sensitivity of the
combined test by approx 8%.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-3-320.jpg)
![•Woman with elevated serum AFP levels were offered
Diagnostic amniotic fluid AFP testing[AFAFP].
•Initially the presence of open spina bifida could be
confirmed only by ultrasound examination of the fetal
spine.
•Now the recommendation is to perform the Triple
marker screen test on all pregnant woman’s between 14
& 20 weeks gestation to assess the risk for neural tube
defects, trisomy 21 & trisomy 18.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-4-320.jpg)
![ A further important breakthrough occurred
with the identification of two biochemical
markers [Pregnancy associated plasma protein
A {PAPP-A} ; Free beta subunit of human
chorionic gonadotrophin {βhCG} ] AND
Ultrasound marker [Nuchal Translucency{NT}]
as markers for down’s syndrome & trisomy 18
in the First trimester.
When used together these markers perform
better than second trimester screening and
have the added advantage of early detection.
These tests may also aid in the asessment of
risk for obstetric complications such as pre-
eclampsia,abruption,preterm labour & IUGR.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-5-320.jpg)
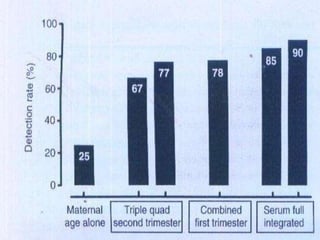
![Suggested protocol for screening
1. Measurement of nuchal translucency[NT] & PAPP-A
in the 1st trimester, but not interpreted or acted upon
until the second trimester.
2. In the second trimester a second serum sample is
drawn and Quadruple test performed.
3. Results for all the six tests , NT, PAPP-A, AFP, uE3
, hCG & DIA are combined into a single risk estimate
for interpretation in the 2nd trimester.
4. 85% detection rate for Down’s Syndrome with only
1% false positive is achieved.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-6-320.jpg)
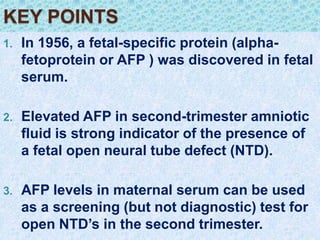
![•TRIPLE SCREEN TEST
•1.ALPHA FETO PROTEIN
•In 1956,Bergstrand & czar described a protein
in fetal serum,located in the α1 region on
electrophoresis[subsequently labelled as α1-
Feto Protein[AFP] that was not present in
maternal serum.
•It is this unique protein that serves as a
marker for leakage of fetal serum into the
amniotic fluid & which is therefore helpful in
diagnosing open fetal lesions.
•AFP is the major serum protein of fetus
synthesized by the fetal yolk sac & fetal liver](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-7-320.jpg)
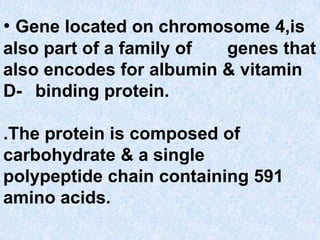
![ The molecular weight and structure of
AFP is similar to that of albumin[about
69kd],but antibodies rised against AFP
have virtual no cross reactivity.
This characteristic was critical in allowing
the development of a veriety of antibody
based assays for reliably measuring AFP
in amniotic fluid & maternal serum.
The protein is very stable @room
temperature in serum as long as a week.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-9-320.jpg)
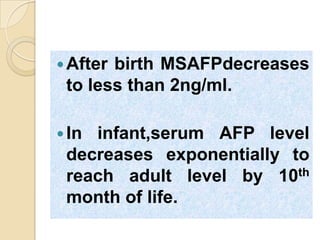
![•Maximum concncentration of AFP in
fetal serum~3,000,000ng/ml reaches by 9
wk gestation decreases to 20,000ng/ml
@ term.
•Maternal serum AFP first detectable
[~5ng/ml] at about 10 wk gestation.
•The concentration increases at a rate of
15% per week to a peak at about
~180ng/ml @ 25 wk gestation,decline
slowly till term.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-11-320.jpg)
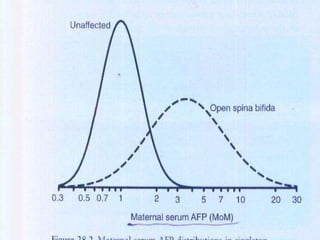
![MULTIPLES OF MEDIAN
[MOM]
•To simplify interpretation of the result , each patient AFP result
expressed as a Multiples of Median[MOM].
•Screening programmes should determine the AFP medians for each
week of gestation from 14 to 20 weeks using at least 100 patients at
each week.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-14-320.jpg)
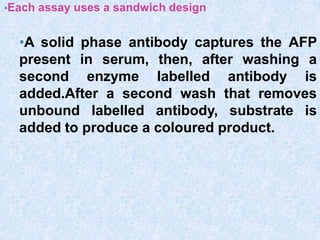
![METHODS FOR DETERMINING α-Feto Protein.
•TRADITIONALLY MEASURED BY RADIO IMMUNO ASSAY [RIA]
•NEWER METHODS USE IMMUNO ENZYMATIC ASSAYS [IEMA]
•Because of it’s lower detection limits , better precision
, speed, avoidance of radiation & ease of automation.
•The FDA has licenced three immuno assay AFP kits for
use in maternal serum screening for neural tube defects,
1. A monoclonal bead assay
2. A microparticles immuno assay
3. A polyclonal bead assay](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-15-320.jpg)
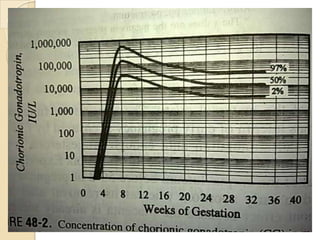
![HUMAN CHORIONIC GONADOTROPHIN[hCG]
It is a glycoprotein hormone with molecular
weight of 36 to 40 kd that is biologically &
immunologically similer to LH[Leutenizing
hormone] but with a longer half life.
Produced during normal pregnancy by the
trophoblast & placenta.
hCG is a hetero dimer having α & β subunits
of which the β subunit is specific for hCG.
All the glycoprotein
hormones[hCG,LH,FSH,TSH] have a similer
biological activity which is characteristic of](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-19-320.jpg)
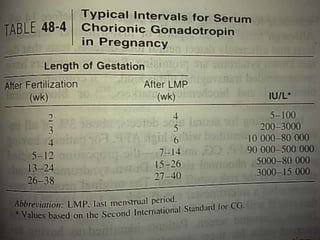
![Free β-hCG was increased
during the 1st trimester in
Trisomy 21[DS] even though
total hCG remained normal.
@16 wk gestation hCG
median level in normal
pregnancy is 20,000 –](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-24-320.jpg)
![METHODS FOR DETERMINING
hCG QUALITATIVE TESTS
1.HOME TEST KITS : MOST COMMONLY USED
PREGNANCY
TESTS.
2.RADIO IMMUNO ASSAY.
3.IMMUNO ENZYMATIC ASSAY[IEMA].
4.IMMUNO RADIOMETRIC ASSAY[IRMA].
QUANTITATIVE TEST : By
IMMUNOCHROMATOGRAPHY
CLINICAL SIGNIFICANCE OF hCG
1. Diagnosis & dating of pregnancy.
2. Predicting the risk of Trisomy 21 & 18.
3. Managing certain neoplasms.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-26-320.jpg)
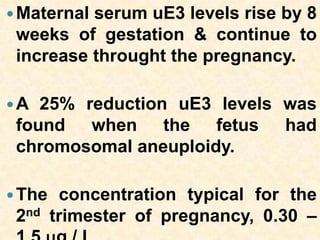
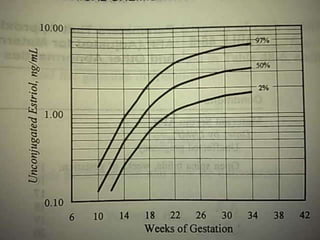
![UNCONJUGATED ESTRIOL [uE3]
Estriol as it’s name implies, is an estrogen with 3
hydroxyl groups [at position 3,16, & 17 ].
3 organs involved in the biosynthesis
1.Fetal adrenal - Cholesterol
2.Fetal liver -
DHEAs[DehydroEpiAndrosteroneSulfate]
3.Placenta - Estriol
Only a minor amount [9%]of the hormone
circulates in plasma unconjugated.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-27-320.jpg)
![The Triple screen has a high detection rate, 80% for
neural tube defecs & 55-60% for chromosomal
aneuploidy & a false positive less than 5 % .
Conditions associated with abnormal maternal
serum screening results
condition AFP hCG uE3
NTD’s VERY
HIGH
- VERY LOW
TRISOMY 21
[DOWN’S
SYNDROME]
LOW HIGH LOW
TRISOMY 18
[EDWARDS
SYNDROME]
LOW LOW VERY LOW](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-31-320.jpg)
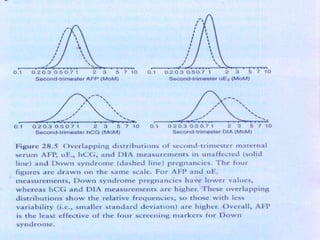
![THE QUADRUPLE TEST[QUAD
TEST]
This includes AFP, Ue3, hCG & an additional marker
INHIBIN-A .
Dimeric Inhibin-A[DIA] is a glycoprotein produced by the
placenta.
It is a dimer , but with dissimilar subunits α & β.
Inhibin-A is measurable in maternal serum & has a
feedback effect on FSH secretion.
The level increases in the 1st trimester until 10 wks & then
remains stable upto 25wks of gestation.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-33-320.jpg)
![RATES OF DETCTION OF DOWN’s
SYNDROME
MATERNAL
AGE[YEAR
S]
TRIPLE
TEST
QUADRUP
LE TEST
DETE
CTION
RATE
FALSE
POSITI
VE
RATE
DETE
CTION
RATE
FALSE
POSITI
VE
RATE
15 - 34 58 3.7 69 4.1
>35 88 19 91 17
<15 69 4.9 77 5.2](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-36-320.jpg)
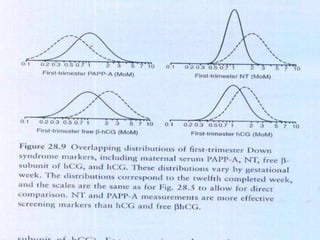
![Pregnancy associated plasma protein – A [PAPP-A]
Measured in the 1st trimester as an early marker
for Down’s Syndrome.
PAPP-A is a high molecular weight Zinc containing
metalloprotein.
It is produced by the trophoblast.
In addition to being a marker of chromosomal
aneuploidy , it is an indicator of early pregnancy
failure & complications.
The level of PAPP-A was found to be significantly
lower in pregnancy with trisomy 21 compared to
unaffected pregnancy.
Persistently lower levels of PAPP-A in second
trimester is indicative of Trisomy 18 .](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-37-320.jpg)

![FOLLOW-UP OF PATIENTS WITH SCREEN POSITIVE
RESULTS
1. Genetic counseling if patient is screen positive.
2. For moderately elevated results [ MOM 2-3 ] a
second test should be done .
3. If second test is negative, screen is taken as
negative.
4. If second test is also gives elevated results
further diagnostic testing to be done.
5. Ultra sonography, Amniocentesis & Analysis of
amniotic fluid for Acetyl choline esterase to
confirm neural tube defects.](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-44-320.jpg)
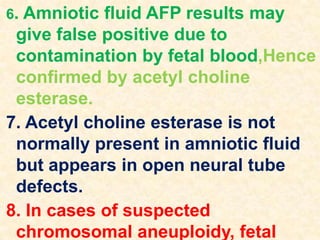
![ACETYL CHOLINE ESTERASE
AChE is a neuronally derived protein.
Measurements of AChE in amniotic fluid
also used to significantly improve the
ability to distinguish between affected &
unaffected pregnancies.
DETERMINED BY GEL-
ELECTROPHORESIS.
This approach has not only proved to be
highly sensitive at detecting open neural
tube defects [99% anencephaly cases &
98% of open spina bifida cases with
positive AFP results ].](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-46-320.jpg)
![7. In 1984, reduced levels of maternal serum AFP in
the second trimester were reported in Down
syndrome pregnancies.
8. Second trimester multiple marker screening is
also able to identify 60% of Trisomy 18
pregnancies.
9. At about the same time, ultrasound
measurements of nuchal translucency (NT)
thickness > 5 mm (at between 11 and 13
completed gestational weeks ) were found to be
the best single marker for Down syndrome.
10. Combining [NT ]measurement with biochemical
markers (combined testing ) in the first trimester](https://image.slidesharecdn.com/maternalserumscreening-140330115945-phpapp01/85/Maternal-serum-screening-49-320.jpg)