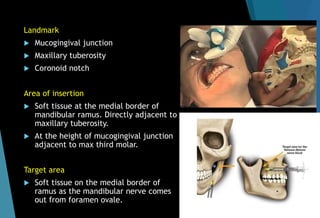
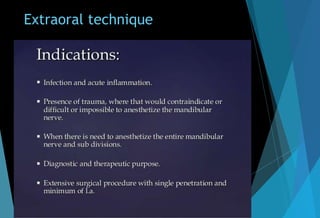
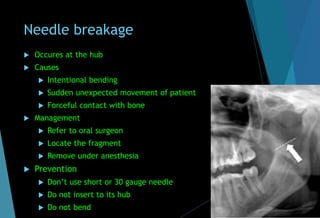
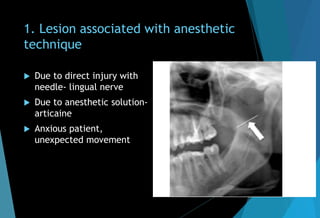
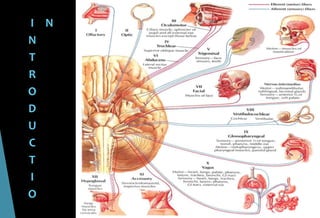
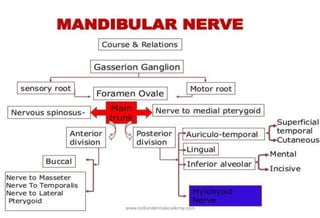
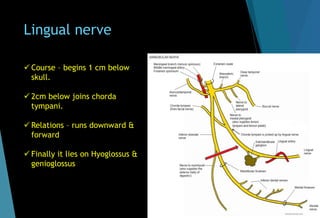
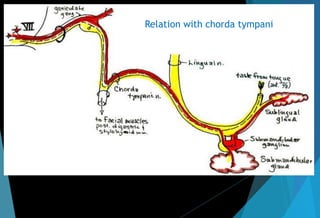
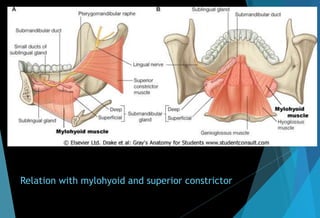
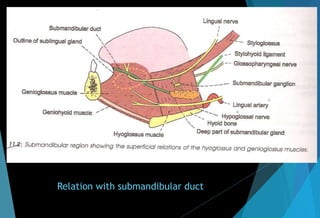
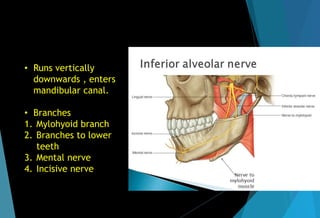
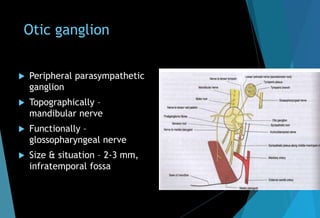
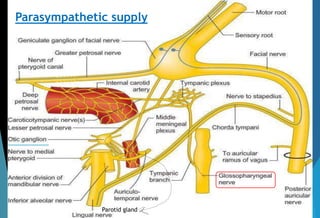
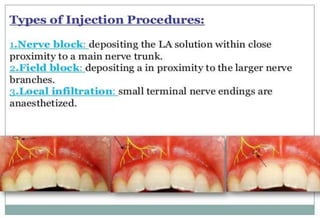
The document discusses the anatomy and branches of the mandibular nerve, including its course, distribution, and supply. It describes various anesthetic techniques for blocking branches of the mandibular nerve, including the inferior alveolar nerve block, lingual nerve block, buccal nerve block, and mental nerve block. It also discusses potential local complications from anesthetic techniques such as needle breakage, prolonged anesthesia, and soft tissue injury.







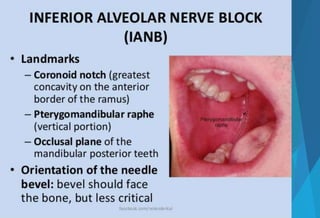
![[A] Inferior alveolar nerve block
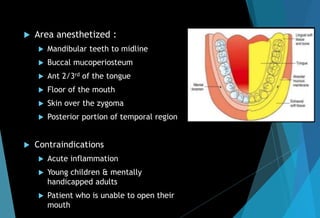
Nerve anesthetized : IA, lingual, mental, incisive.
Area anesthetized : mandibular teeth till midline, buccal
mucoperiosteum, ant. 1/3rd of tongue & floor of mouth.
Indication : multiple extraction, buccal soft tissue
anesthesia.
Contraindication: acute infection, allergic, very young
child.
Advantage: wide area of anesthesia
Disadvantage: high rate of in adequate anesthesia, self
inflicted soft tissue trauma.](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-41-320.jpg)

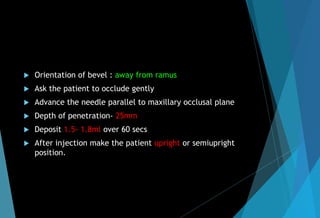
![ Slowly withdraw the needle till half
length remain inside & deposit 0.2ml
to anesthetize lingual nerve.
Subjective symptoms : numbness of
lower lip & tongue
Objective symptoms : no response to
EPT & no pain during procedure.
Precautions : don’t deposit if bone is
not contacted.
Failure of anesthesia : deposited to
far anteriorly, posteriorly, bifid
canal.
[B] Lingual nerve block](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-45-320.jpg)
![[C] Buccal nerve block
Landmark : mandibular
molar, mucobuccal fold.
Operator position : 8
o’clock & 10 o’clock
Penetrate 2-4 mm bevel
facing downwards.
If aspiration is –ve
deposit 0.3ml/10sec](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-46-320.jpg)
![[D] Mental nerve block
Area anesthetized : buccal mucous membrane ant to
mental foramen, lower lip
Technique :
Locate mental foramen
Insert at mucobuccal fold ant to mental foramen
Target area : between apices of first & second
Premolar
Depth of penetration 5-6 mm
If aspiration is –ve deposit 0.6ml over 20 sec
Procedure for incisive nerve block is similar to
Mental nerve block.](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-47-320.jpg)
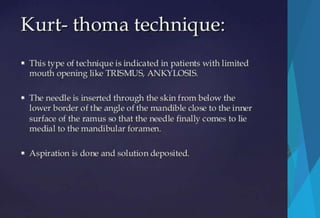
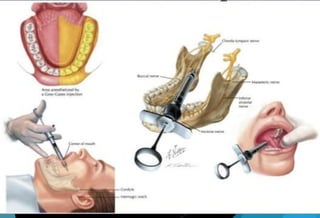
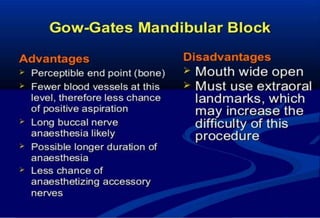
![[E] Gow gates technique (1973)
Nerve anesthetized
Inferior alveolar
Mental
Incisive
Lingual
Mylohyoid
Auriculotemporal
Long buccal (in 75% of the cases)](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-48-320.jpg)
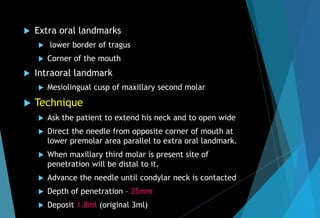
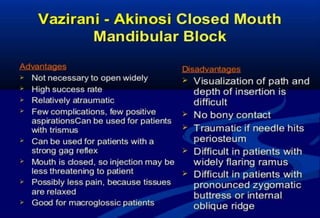
![[F] Vazirani Akinosi closed mouth
technique (1977)
Synonyms :
Akinosi technique
Closed mouth Mandibular nerve block
Tuberosity technique
Indications
Limited mandibular opening
Inability to visualize landmarks for IANB
Nerve anesthetized
IAN, incisive, mental, lingual, mylohyoid](https://image.slidesharecdn.com/mandibularnerveabhi-180529134401/85/Mandibular-nerve-53-320.jpg)