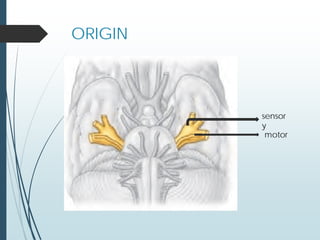
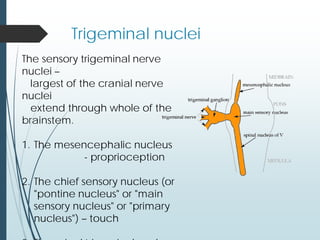
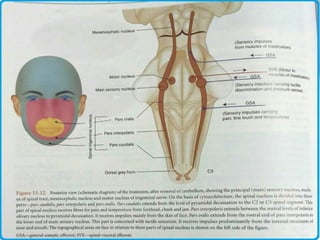
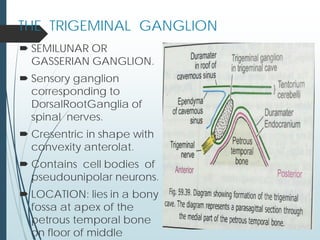
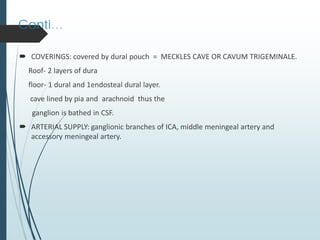
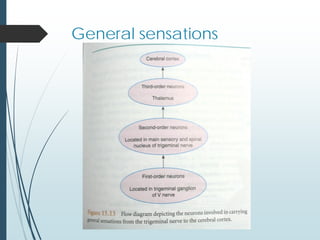
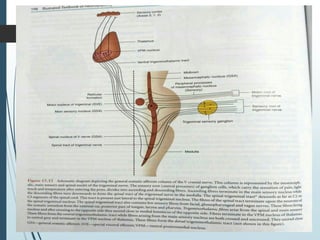
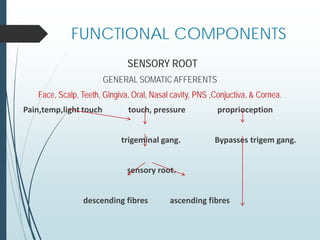
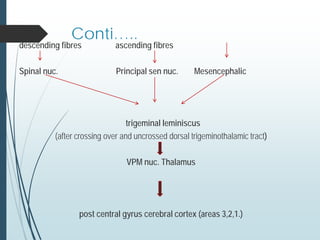
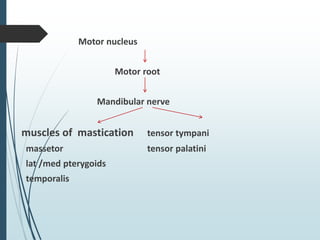
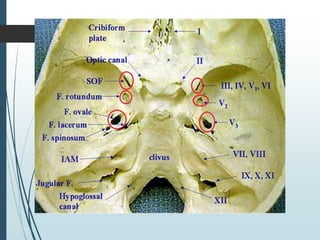
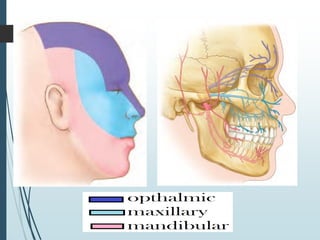
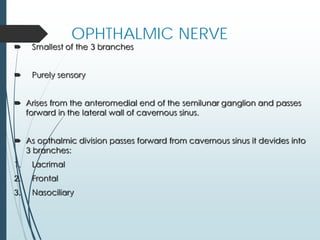
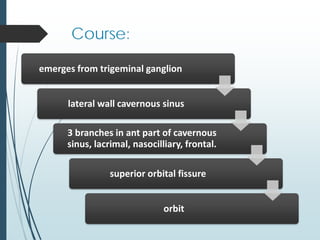
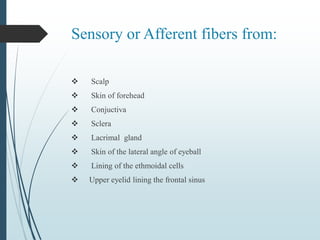
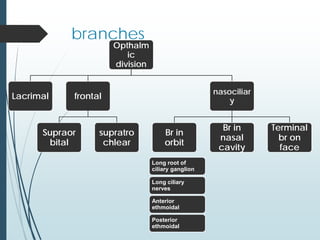
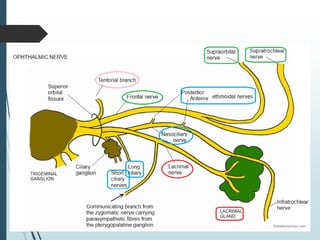
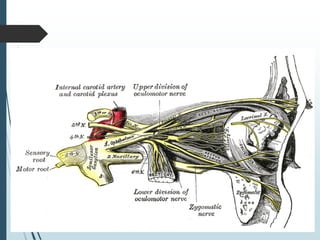
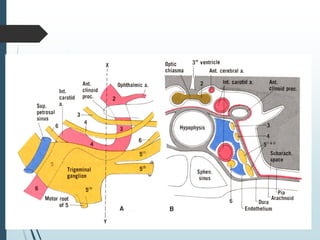
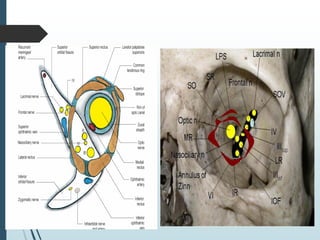
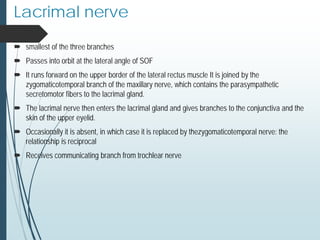
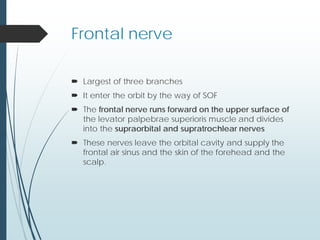
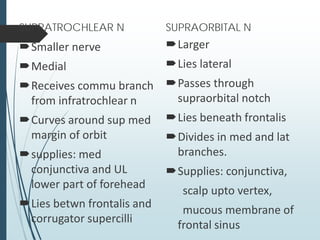
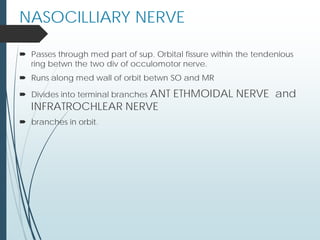
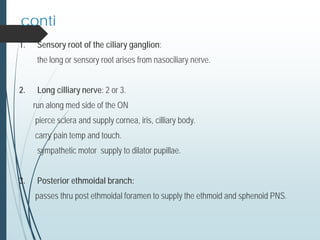
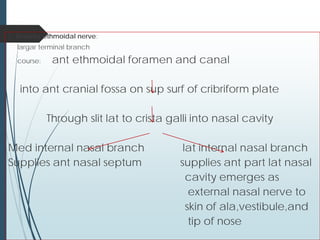
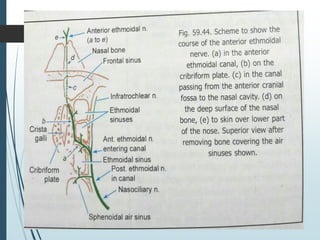
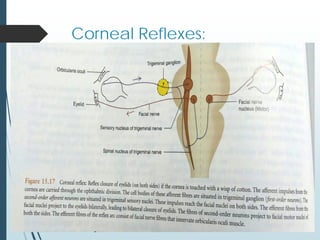
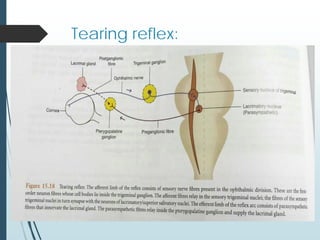
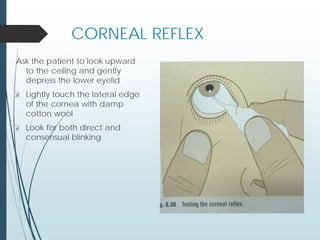
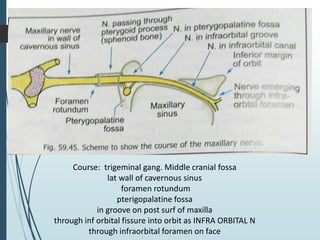
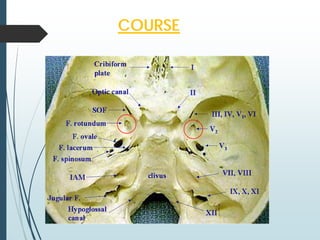
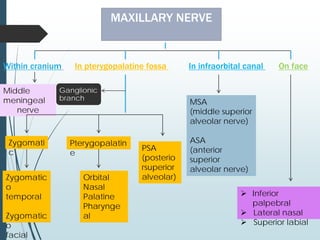
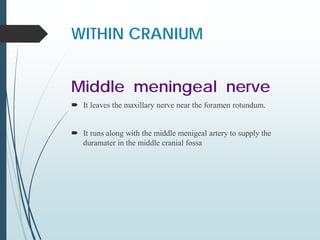
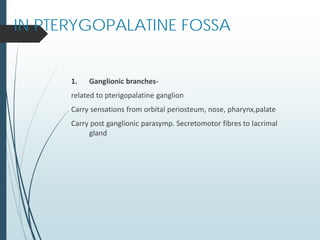
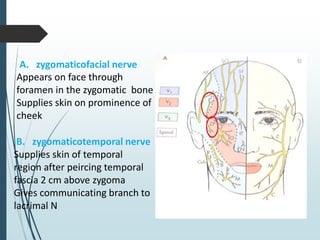
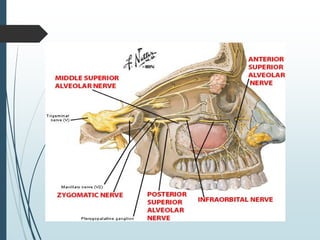
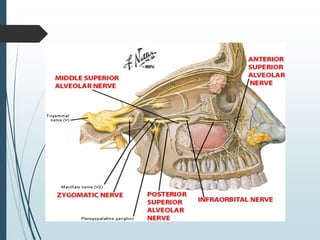
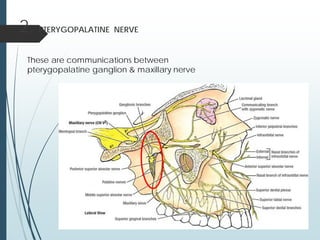
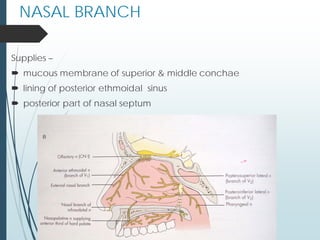
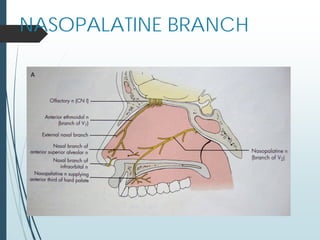
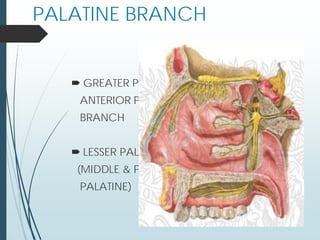
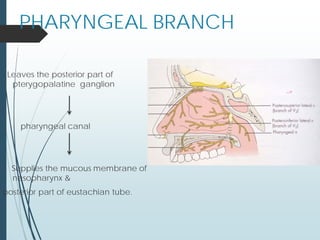
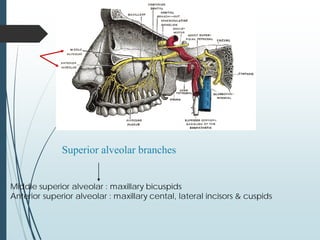
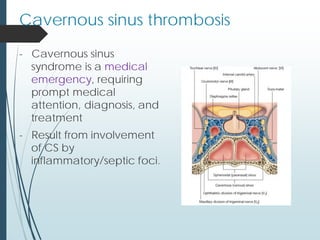
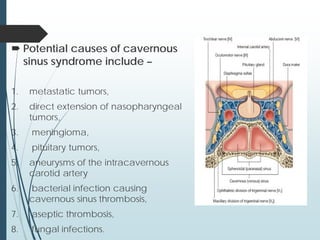
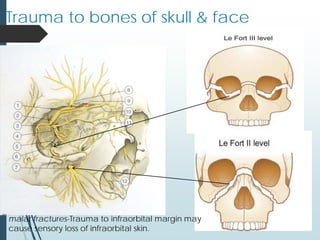
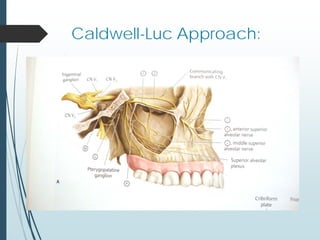
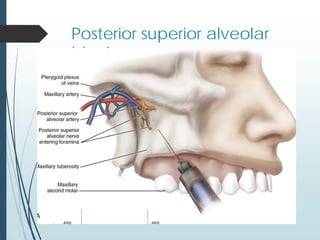
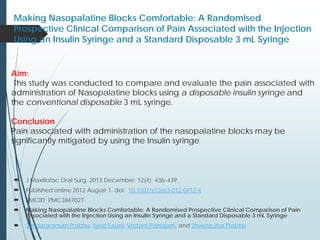
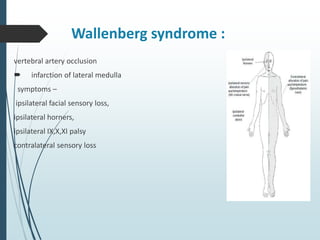
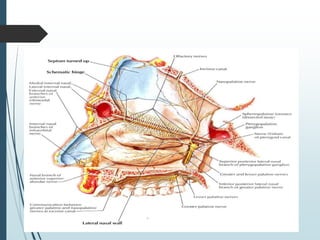
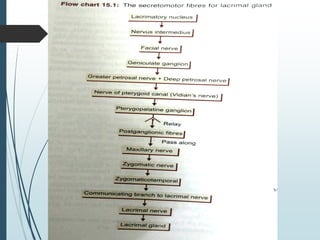
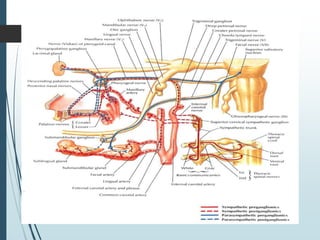
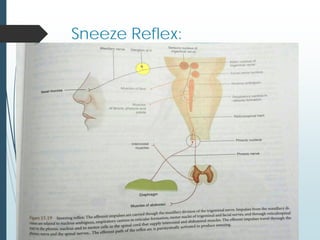
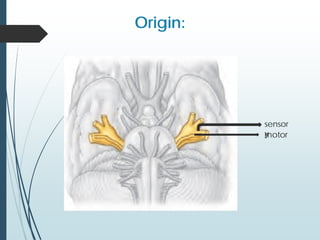
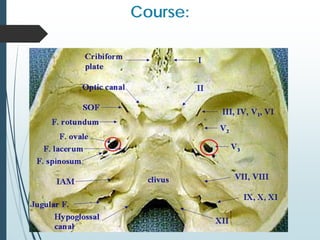
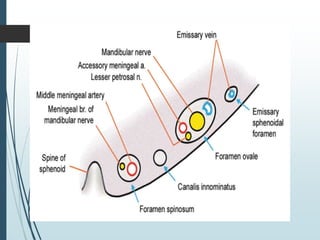
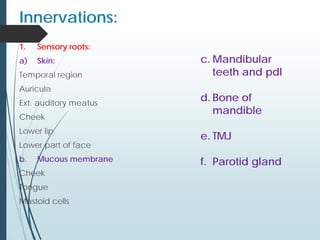
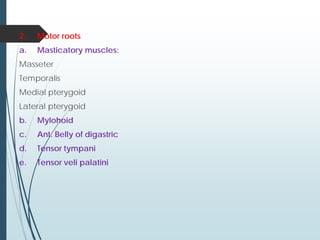
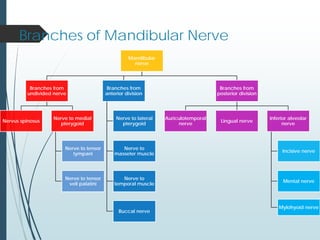
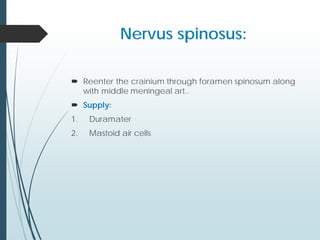
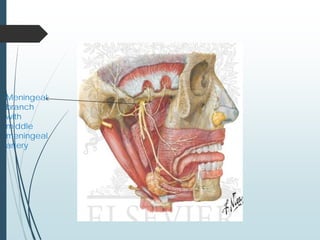
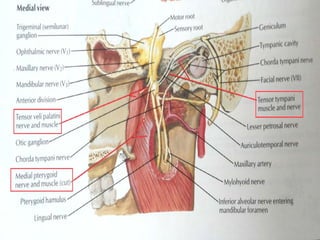
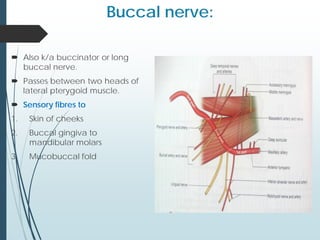
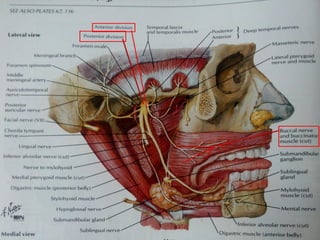
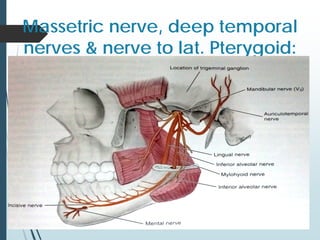
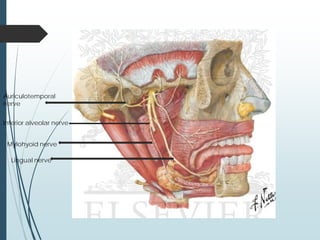
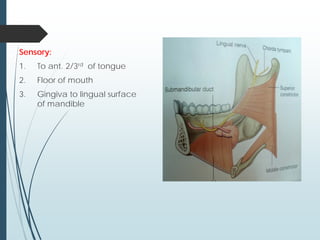
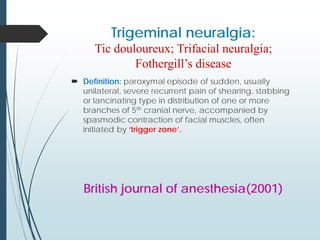
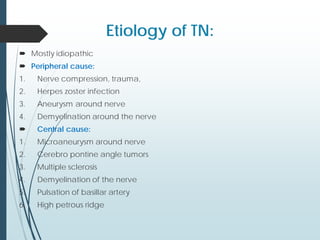
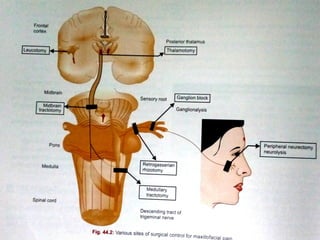
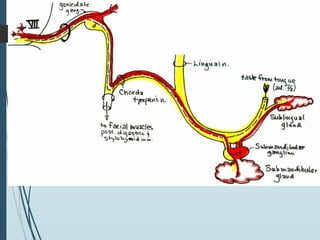
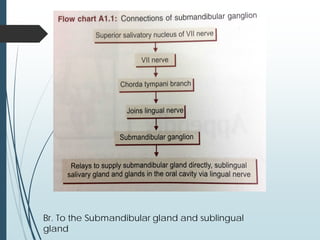
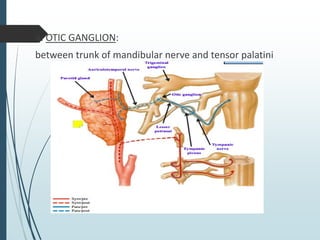
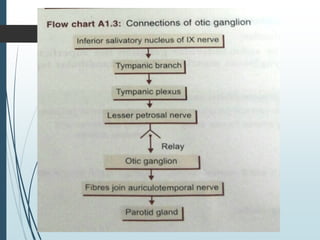
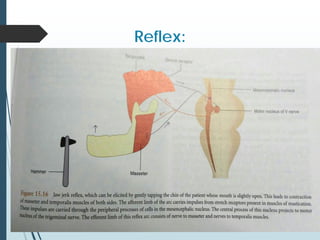
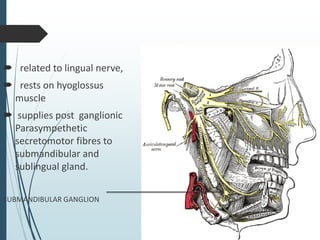
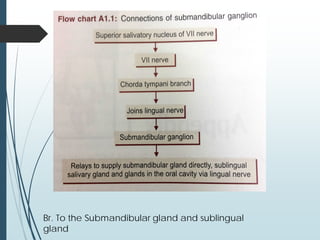
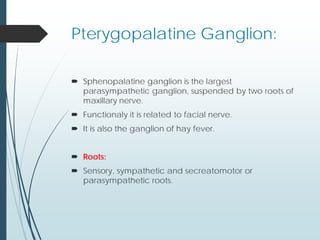
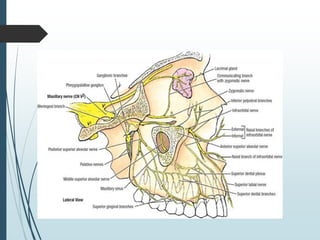
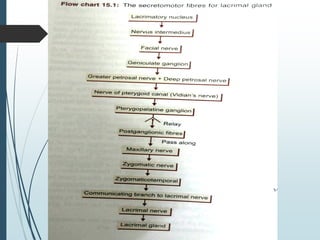
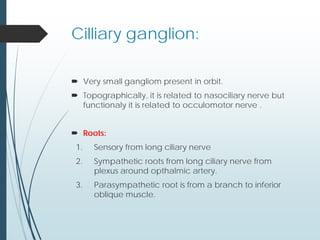
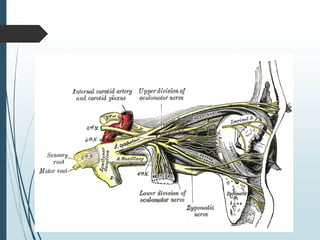
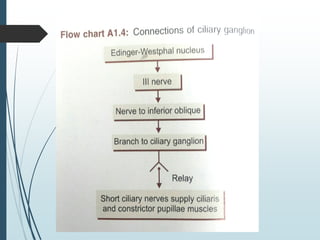
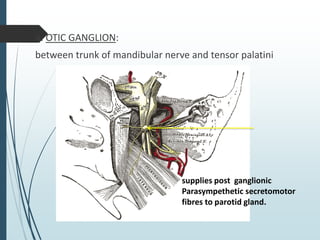
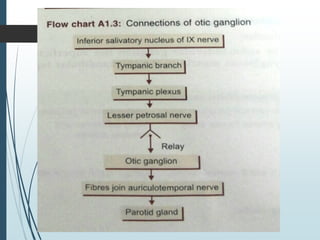
The document provides an extensive overview of the trigeminal nerve, detailing its anatomy, branches, and functions, and clinical implications such as trigeminal neuralgia and complications arising from injuries or infections. It discusses the sensory and motor components of the nerve and its associated ganglia, as well as clinical applications related to maxillary nerve injuries and pathologies. Additionally, it addresses conditions like cavernous sinus syndrome and syphilis affecting the trigeminal system.