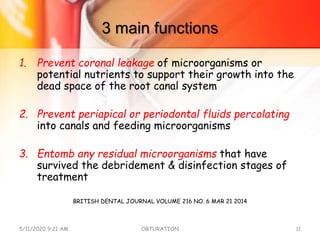
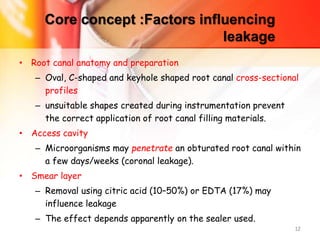
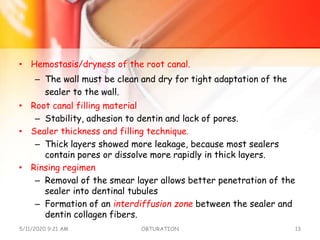
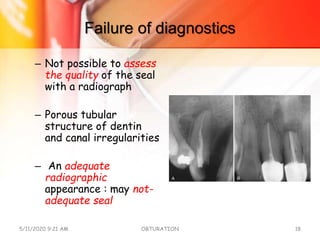
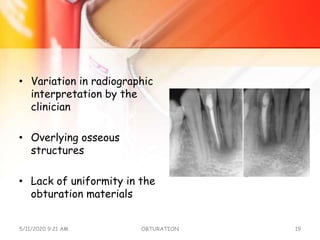
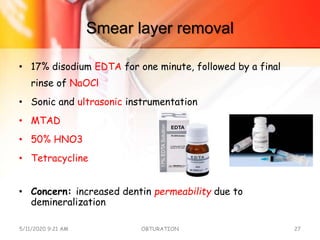
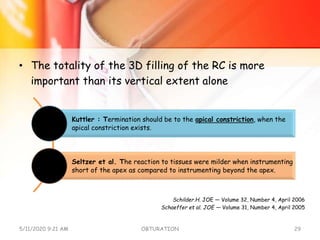
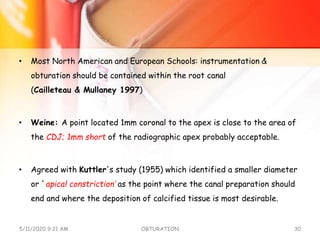
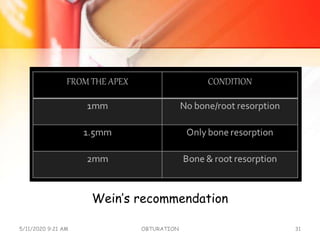
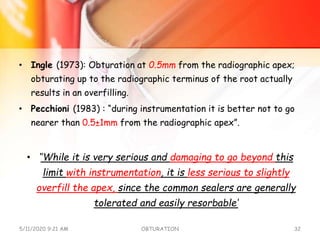
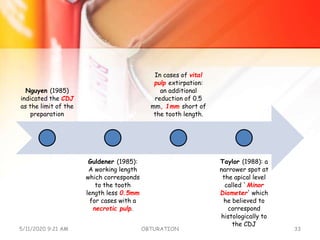
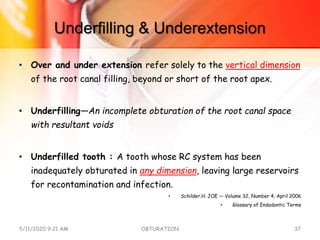
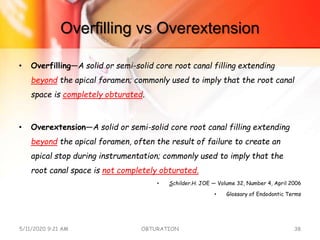
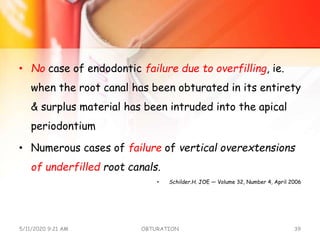
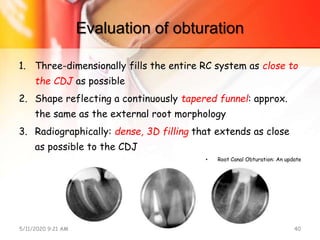
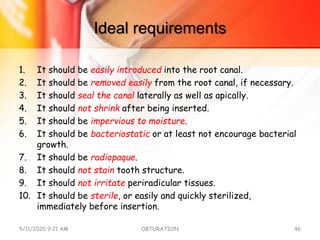
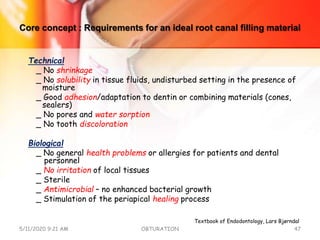
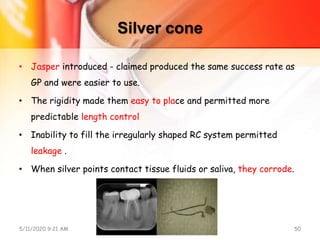
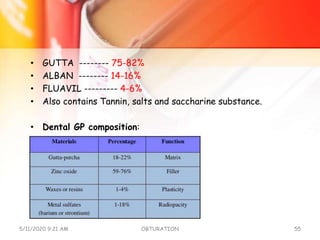
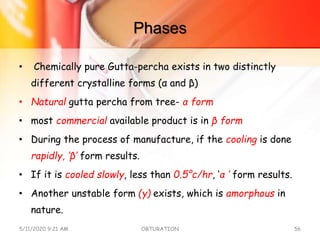
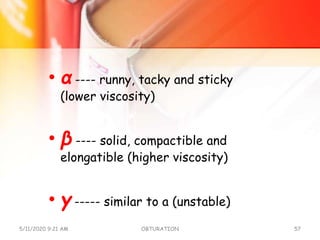
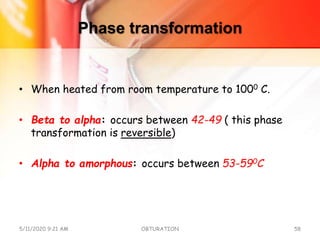
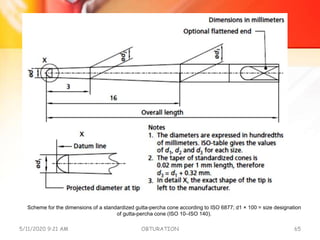
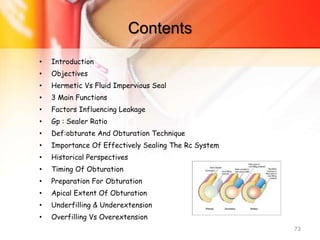
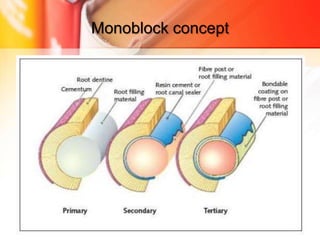
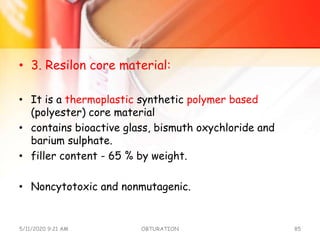
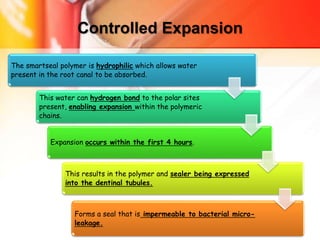
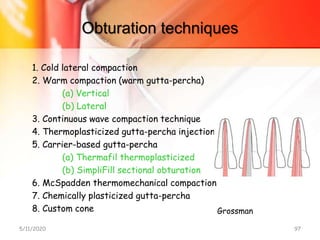
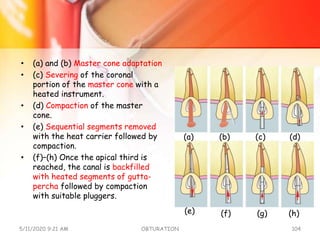
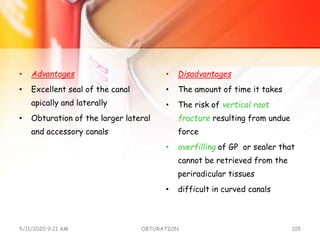
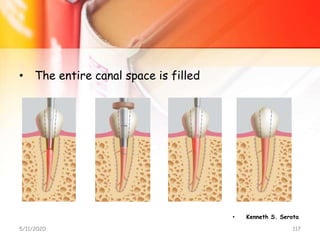
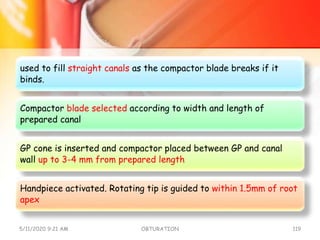
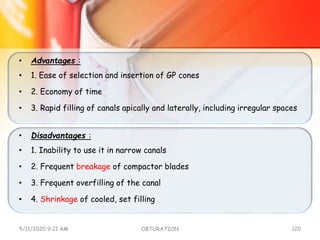
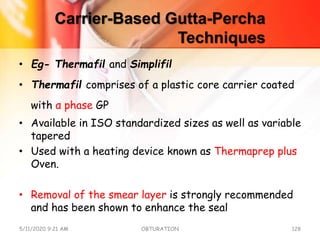
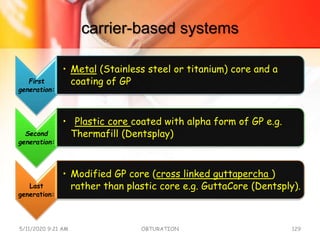
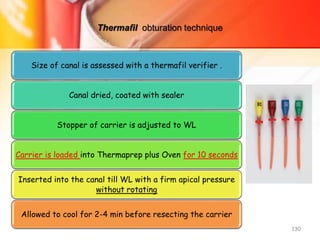
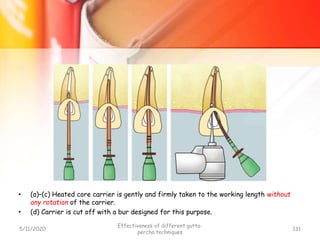
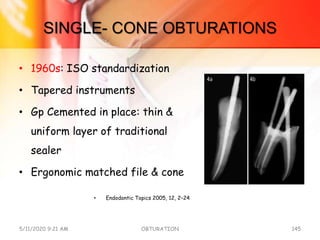
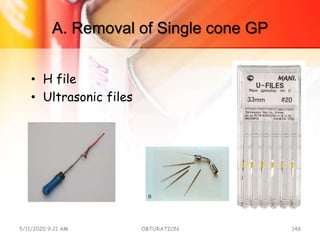
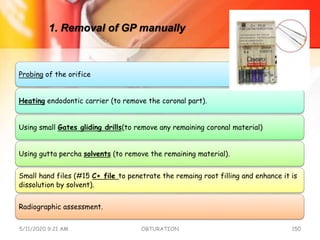
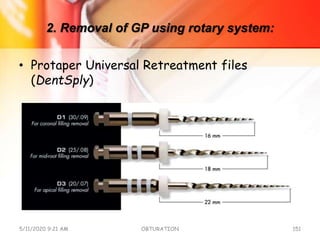
The document discusses the significance and techniques of obturation in endodontics, emphasizing that comprehensive sealing of the root canal is crucial for treatment success. It covers various aspects including definitions, materials used, historical perspectives, and factors affecting leakage, highlighting the importance of achieving a hermetic seal. The document also reviews the challenges and considerations in evaluating the quality of obturation, including methods of clinical and radiographic assessment.