1) The patient, a 41-year-old male, has been feeling drunk and unable to walk properly or think clearly for several weeks.
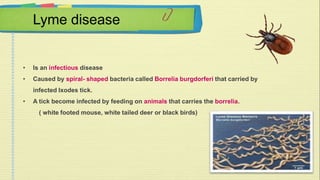
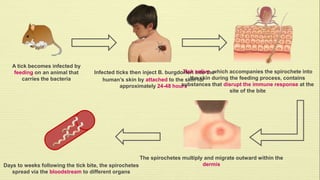
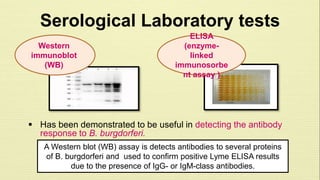
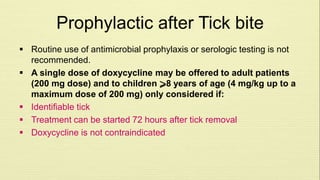
2) Lyme disease is caused by the bacteria Borrelia burgdorferi, which is transmitted through the bite of infected blacklegged ticks.
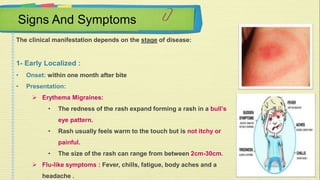
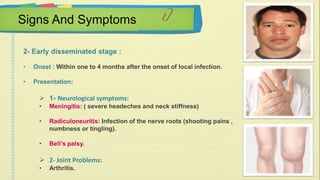
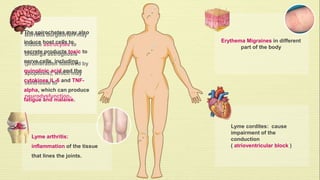
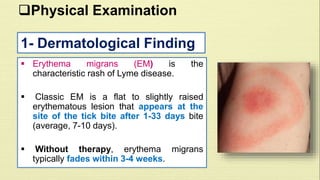
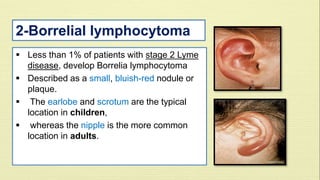
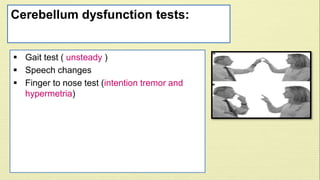
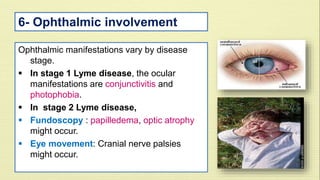
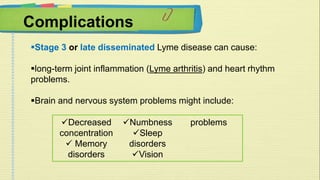
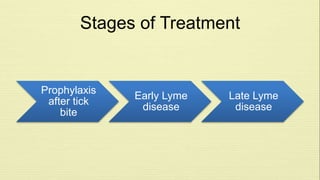
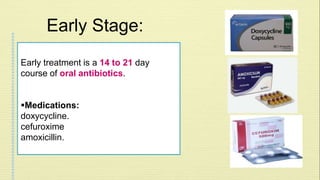
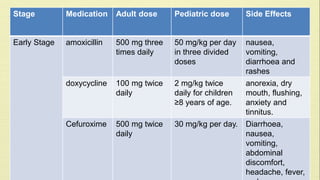
3) The presentation of symptoms depends on the stage of infection, ranging from a bullseye rash in the early localized stage to neurological or heart problems in later disseminated stages.