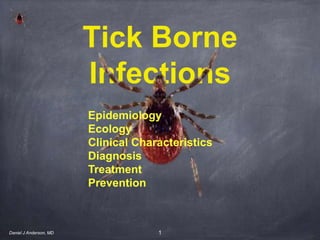
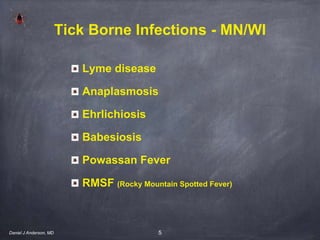
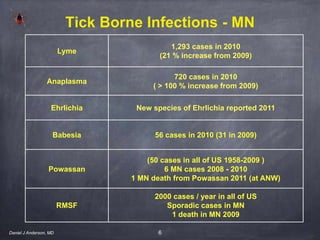
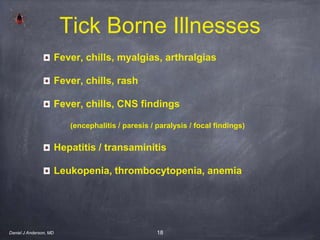
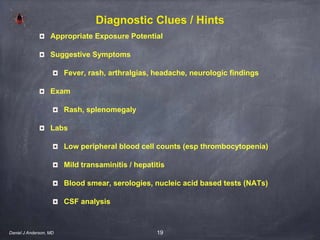
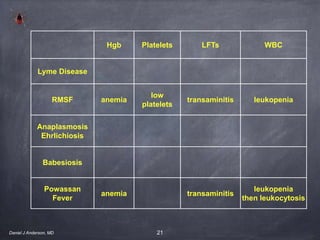
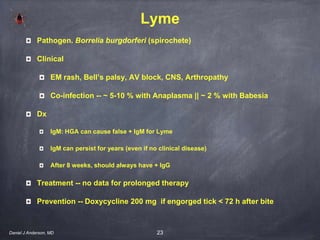
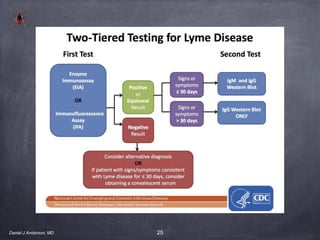
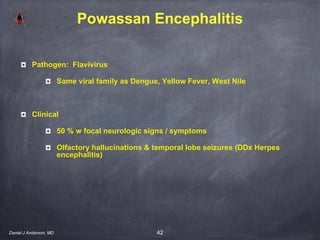
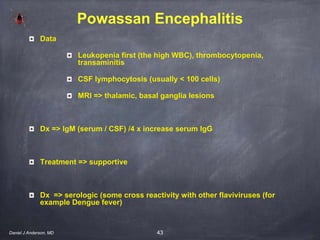
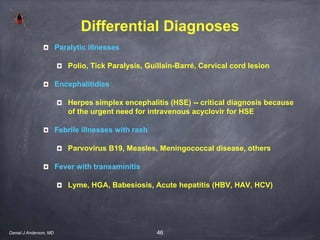
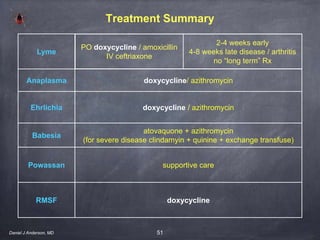
This document provides an overview of tick-borne infections including Lyme disease, anaplasmosis, ehrlichiosis, babesiosis, Powassan virus, and Rocky Mountain spotted fever. It discusses the epidemiology, ecology, clinical presentation, diagnosis, treatment and prevention of these infections. Key points include expanding ranges for ticks and infections, new diagnostic tests such as nucleic acid tests, similarities and differences between diseases, and recommendations for doxycycline treatment of most infections.
![2
Tick-Borne Infections
Challenges
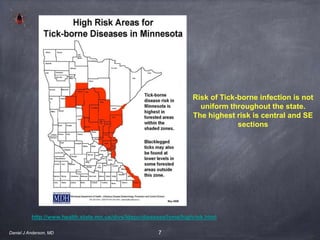
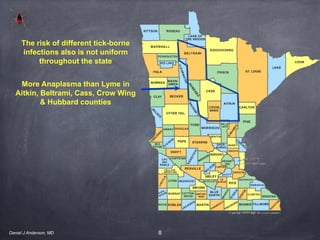
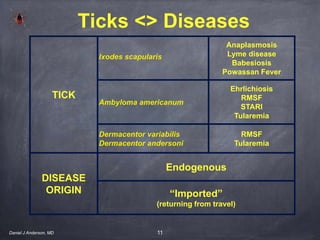
Expanding / changing geography of ticks / infections
New infections / newly recognized “old” infections
Newly identified -- new Ehrlichia species 2011
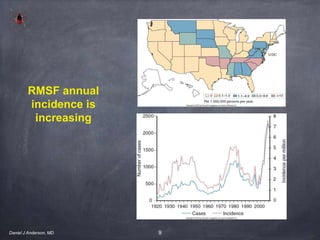
Old infections | new to MN -- Powassan fever, RMSF
Clinical clues that might suggest tick-borne infection
Fever plus [rash, severe headache, mild hepatitis]
low blood cell counts [esp platelets]]
Diagnostic tests -- blood smear, serology, PCR
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-2-320.jpg)

![24
Lyme Diagnosis
Clinical diagnosis (ie no serology needed) if exposure to deer tick AND
Bilateral Bell’s Palsy
III ° AV block or complete heart block [CHB]
Characteristic erythema migrans [EM] rash
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-24-320.jpg)
![33
Human Granulocytic Anaplasomsis [HGA]
Pathogen Anaplasma phagocytophilum
Clinical
up to 35 % coinfected with Lyme and/or Babesia
fever, chills, headache, myalgia, and malaise,cough, diarrhea, confusion,
and lymphadenopathy,
17 % severe multisystem organ failure / SIRS / even death (Lyme does not
do this)
rash is not common
Data
leukopenia, thrombocytopenia,
mild hepatitis / transaminitis
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-33-320.jpg)
![34
Human Granulocytic Anaplasomsis [HGA]
Dx
Peripheral blood smear (in WBCs)
30 - 80 % + morulae
seen in granulocytes
Serology
NATs (PCR)
Treatment
Doxycycline (will also cover potential Lyme coinfection)
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-34-320.jpg)
![36
Human Monocytotropic Ehrlichiosis
[HME]
Pathogens
E canis / E chaffeensis / / E muris
Clinical
< 50 % with rash (but more often than with HGA)
More common farther south than Anaplasmosis (HGA)
Data -- Lymphopenia, morulae RARE on blood smear (vs HGA)
Dx -- Serology, PCR
Treatment - doxycycline
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-36-320.jpg)

![44
RMSF
Pathogen Rickettsiae rickettsii
Clinical (2 - 14 day [median 7] incubation)
fever, headache, nausea / emesis / diarrhea
rash usually ~ 3 days AFTER other signs
begins wrists / ankles
Data
thrombocytopenia (sometimes anemia) WBC often nl
coagulopathy, DIC, CXR changes
Dx serology (? PCR on clinical specimens)
Treatment
doxycycline early in course illness
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-44-320.jpg)

![53
Tick Removal
Grab Tick with tweezers close to skin
Pull steadily straight up
Clean area [alcohol, iodine, soap & H20]
Daniel J Anderson, MD](https://image.slidesharecdn.com/tickborneinfections-130612100056-phpapp01/85/Tick-borne-infections-53-320.jpg)