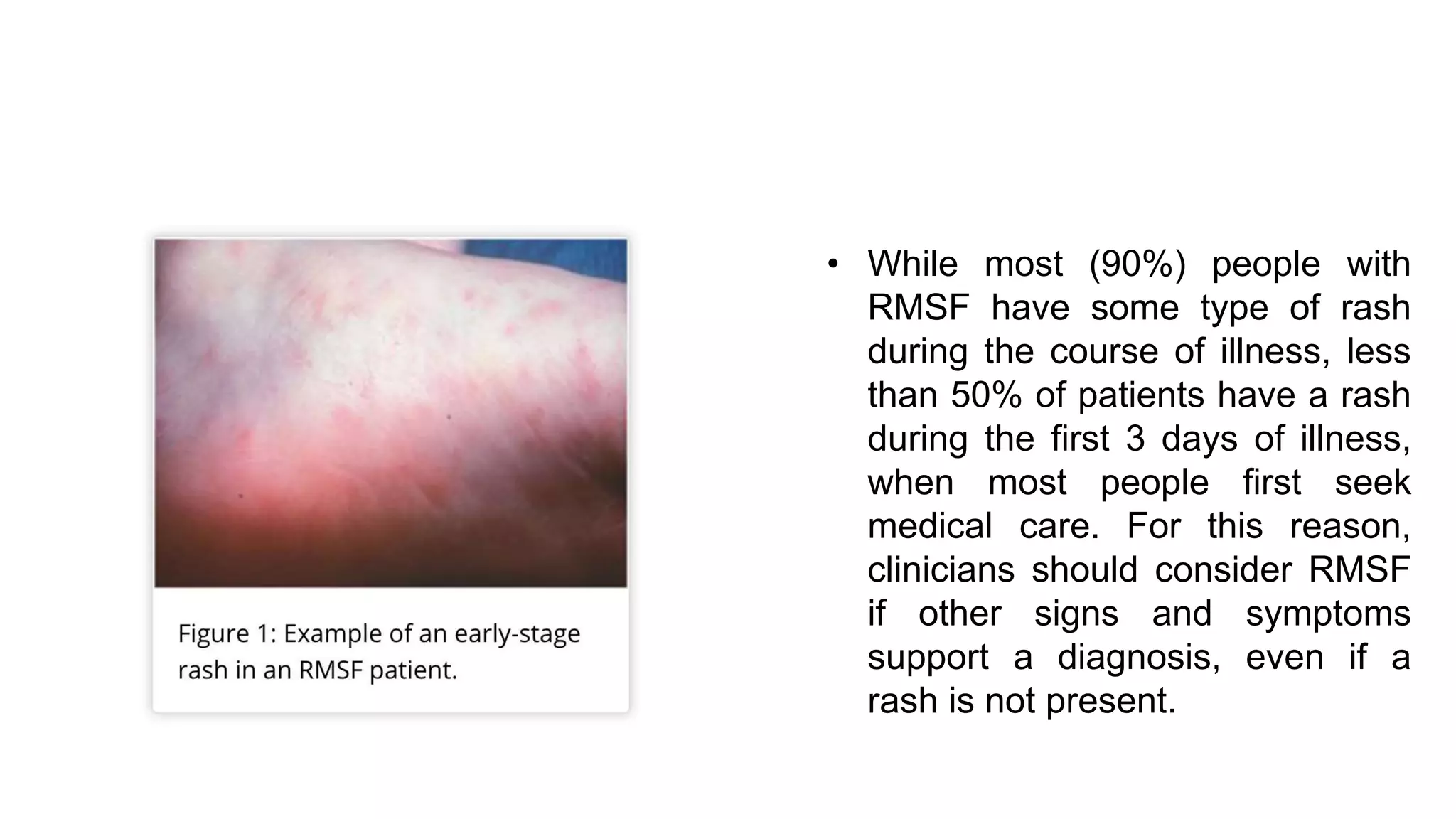
Anaplasmosis is a tickborne disease caused by Anaplasma phagocytophilum, primarily transmitted through blacklegged ticks, with cases peaking during the warmer months. Symptoms include acute febrile illness, with potential severe manifestations, and it can be difficult to diagnose in early stages, necessitating presumptive treatment based on clinical suspicion. Prompt recognition and early treatment with doxycycline is critical to prevent severe outcomes, while laboratory confirmation is also important for disease monitoring.