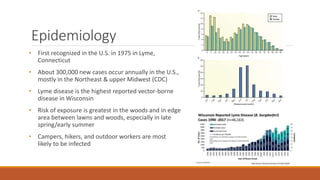
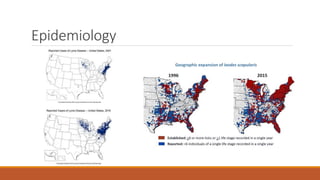
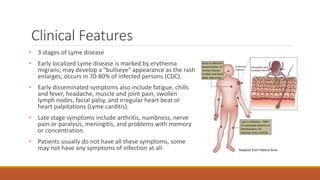
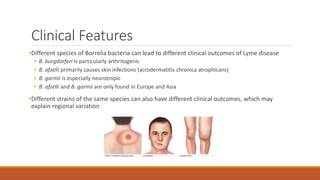
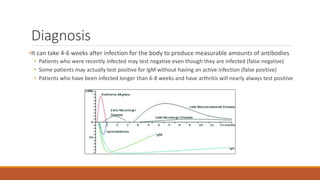
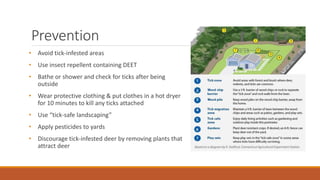
This document provides comprehensive information about Lyme disease, detailing its causative agent, life cycle, transmission, clinical features, diagnosis, treatment, and prevention strategies. It highlights the significant number of annual cases in the U.S., particularly in the Northeast and Midwest, and discusses the complexities of persistent symptoms post-treatment and the controversy surrounding 'chronic Lyme disease.' Educational resources and guidelines for prevention, as well as references for further reading, are also included.