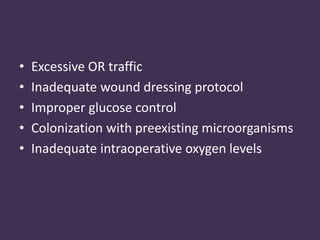
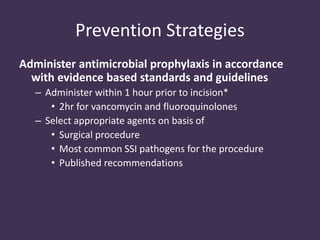
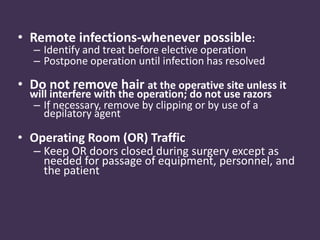
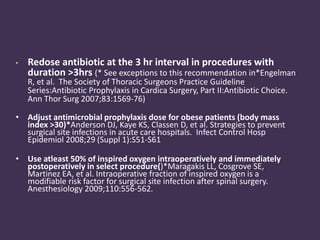
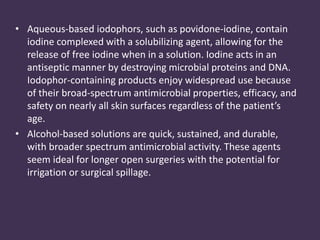
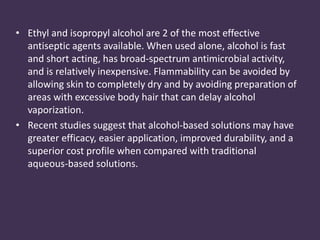
Proper aseptic technique and administration of antimicrobial prophylaxis are essential for preventing surgical site infections. The document discusses the history and evolution of aseptic techniques, including the use of sterile instruments and dressings. It provides detailed steps for surgical hand scrubbing and gloving using aseptic technique. The timing and appropriate selection of antimicrobial agents for prophylaxis is important to reduce infection risks according to several studies discussed.