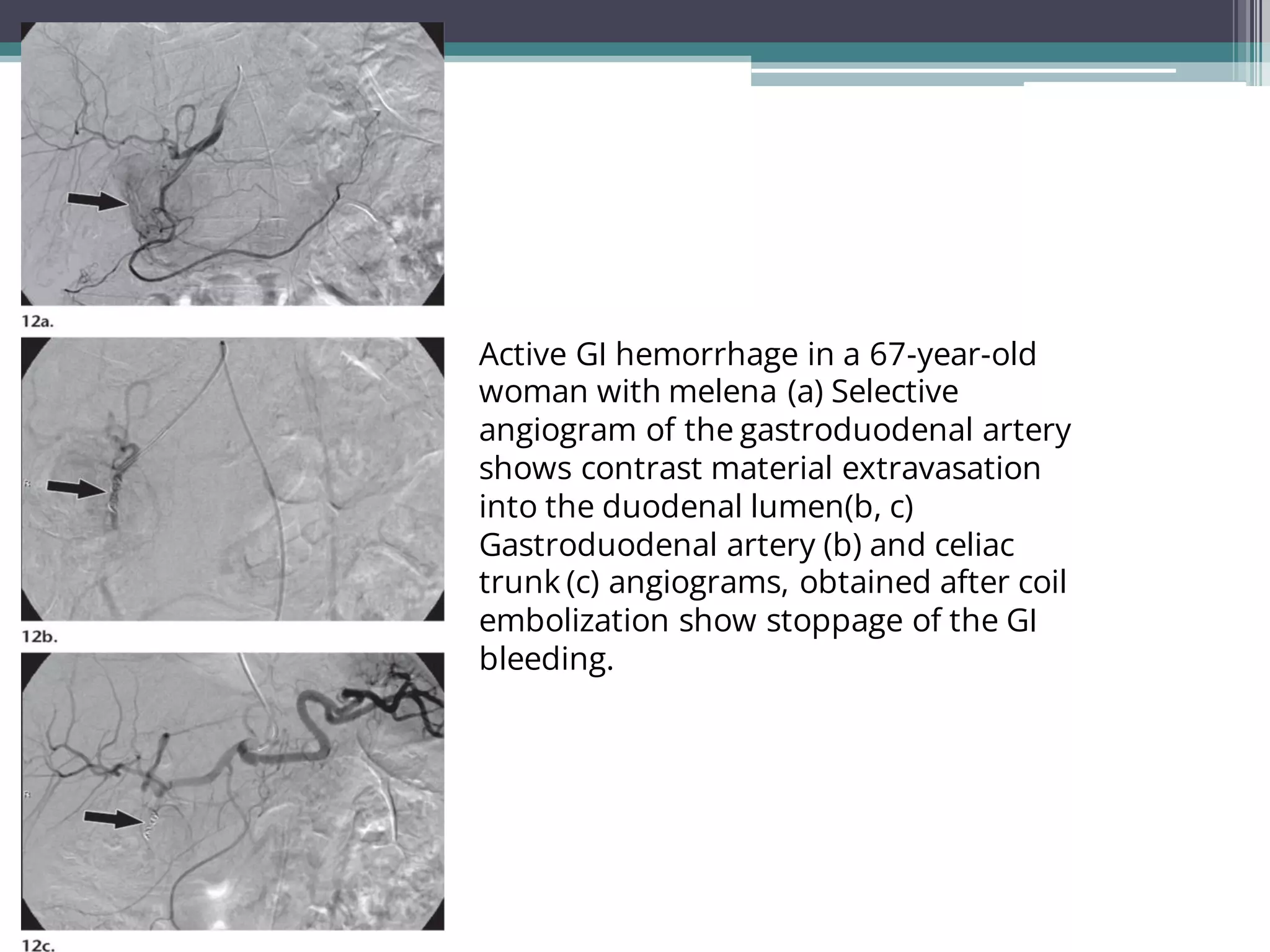
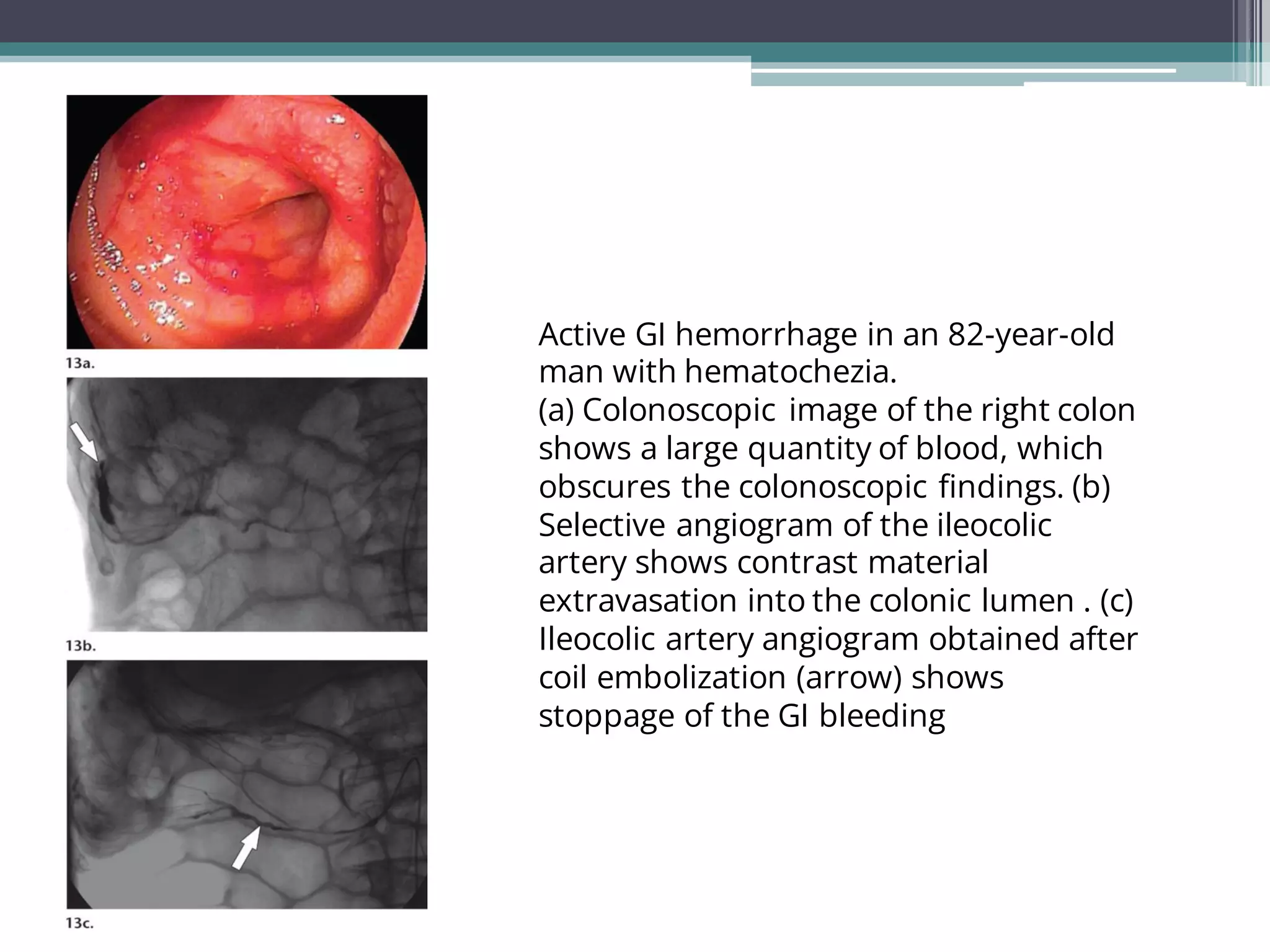
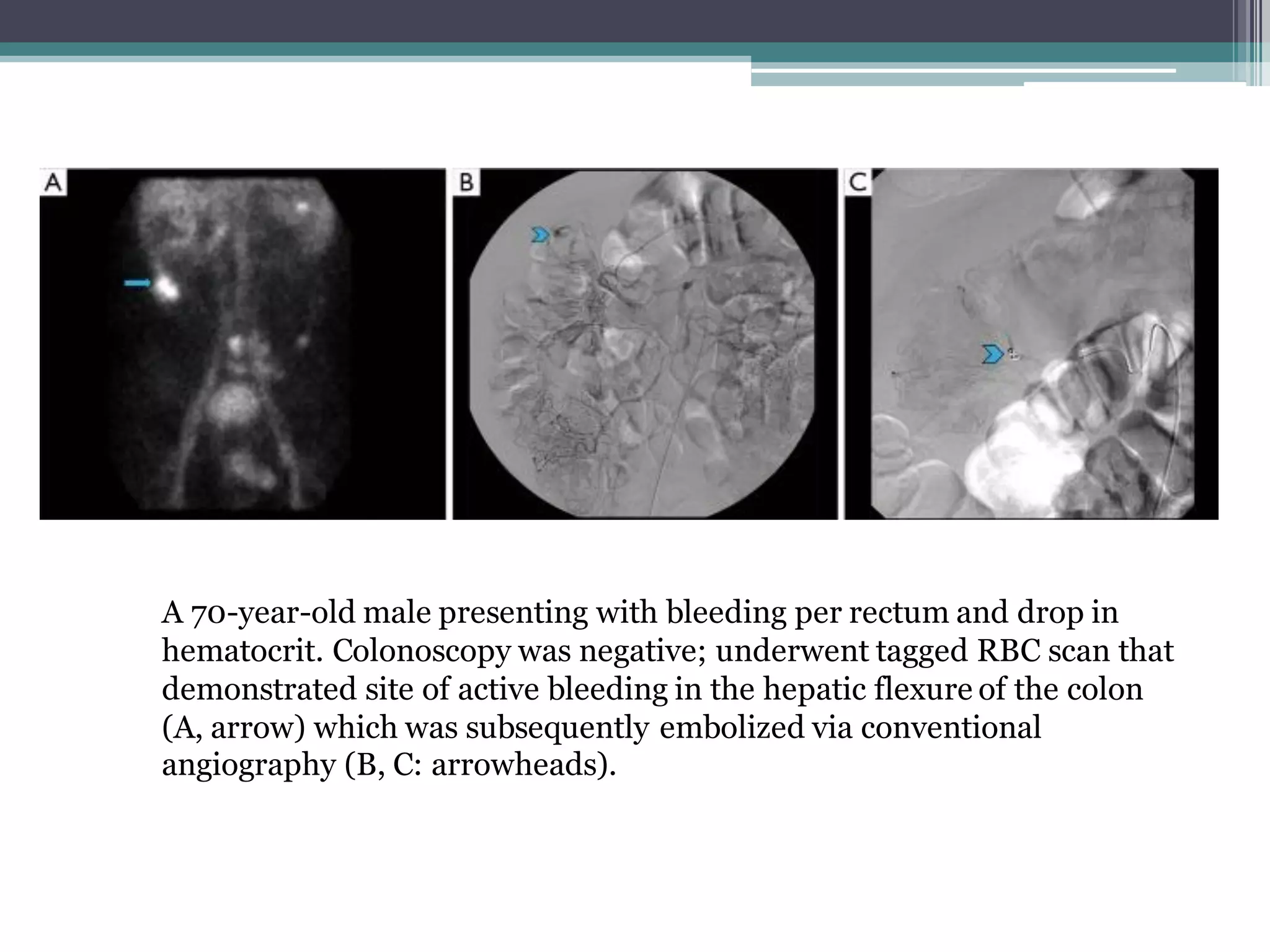
Lower gastrointestinal bleeding refers to bleeding from the small and large intestines. Common causes include hemorrhoids, diverticulosis, angiodysplasia, inflammatory bowel disease, colon polyps and cancer. Diagnostic evaluation involves colonoscopy, CT/CT angiography, capsule endoscopy, nuclear scintigraphy and angiography. Colonoscopy allows for both diagnosis and treatment but other imaging modalities are useful when colonoscopy is non-diagnostic or not possible. Angiography can localize the bleeding site and provide therapeutic embolization in unstable patients. Surgical or endoscopic intervention may be needed depending on the cause of bleeding.