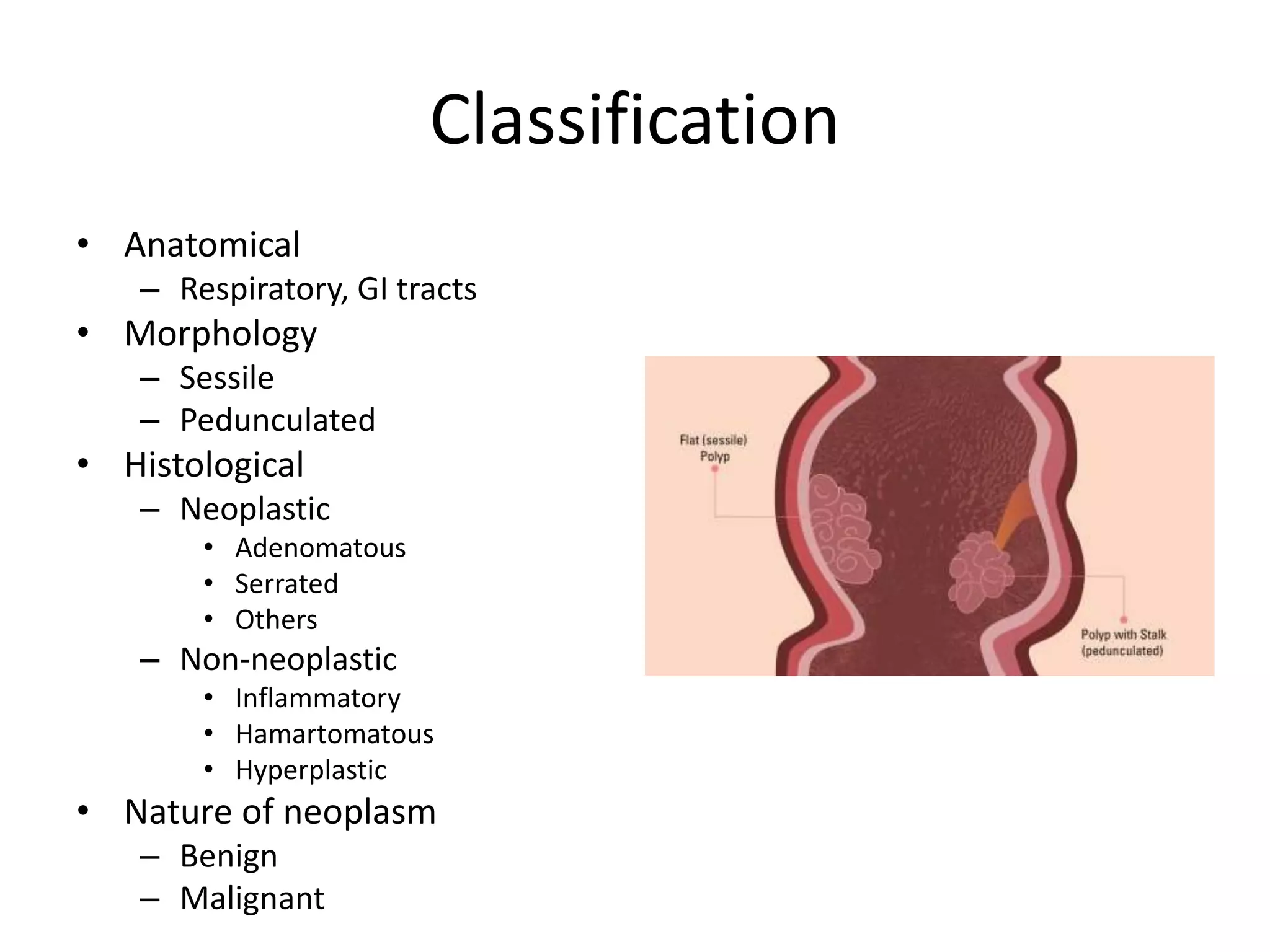
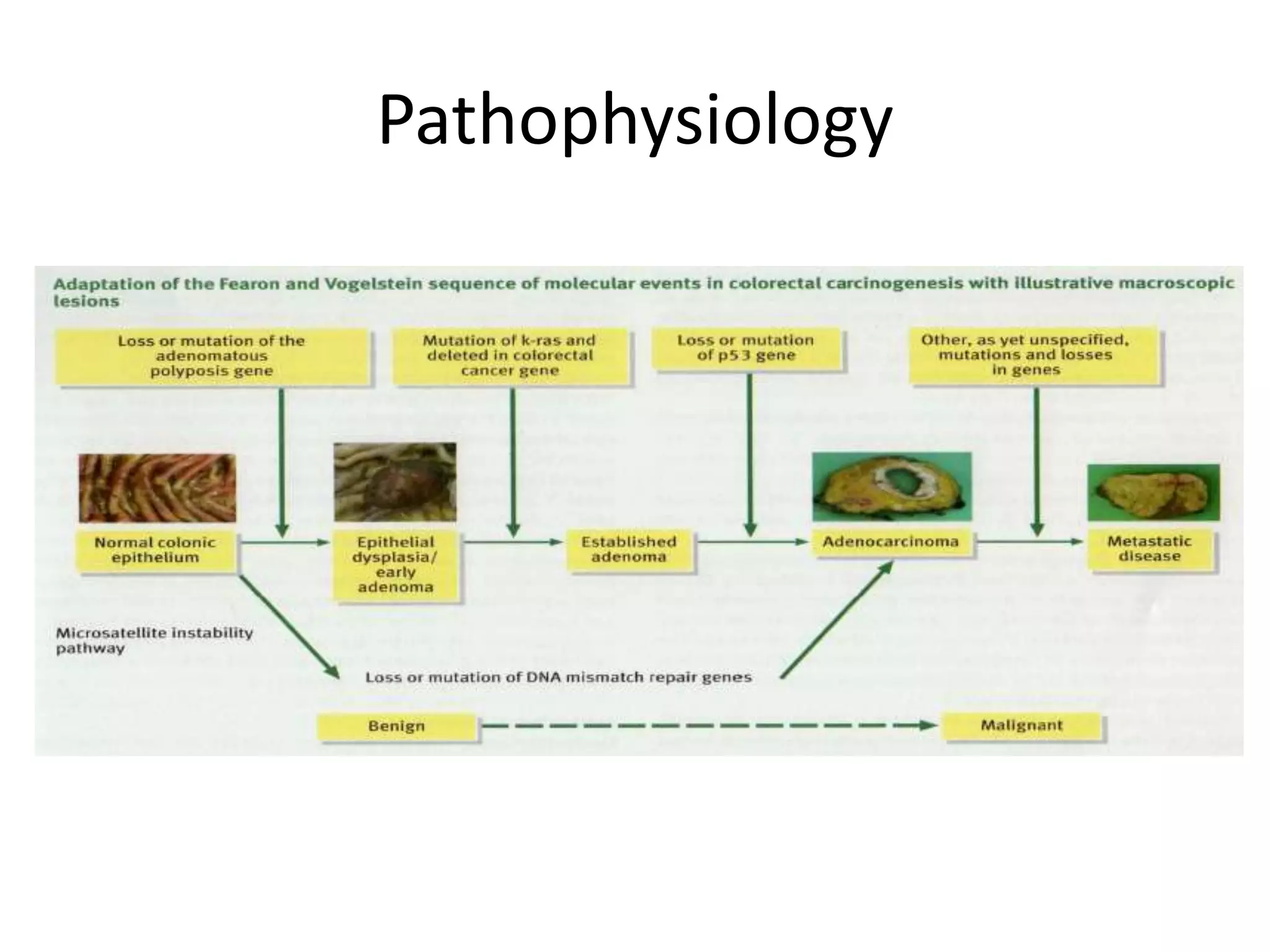
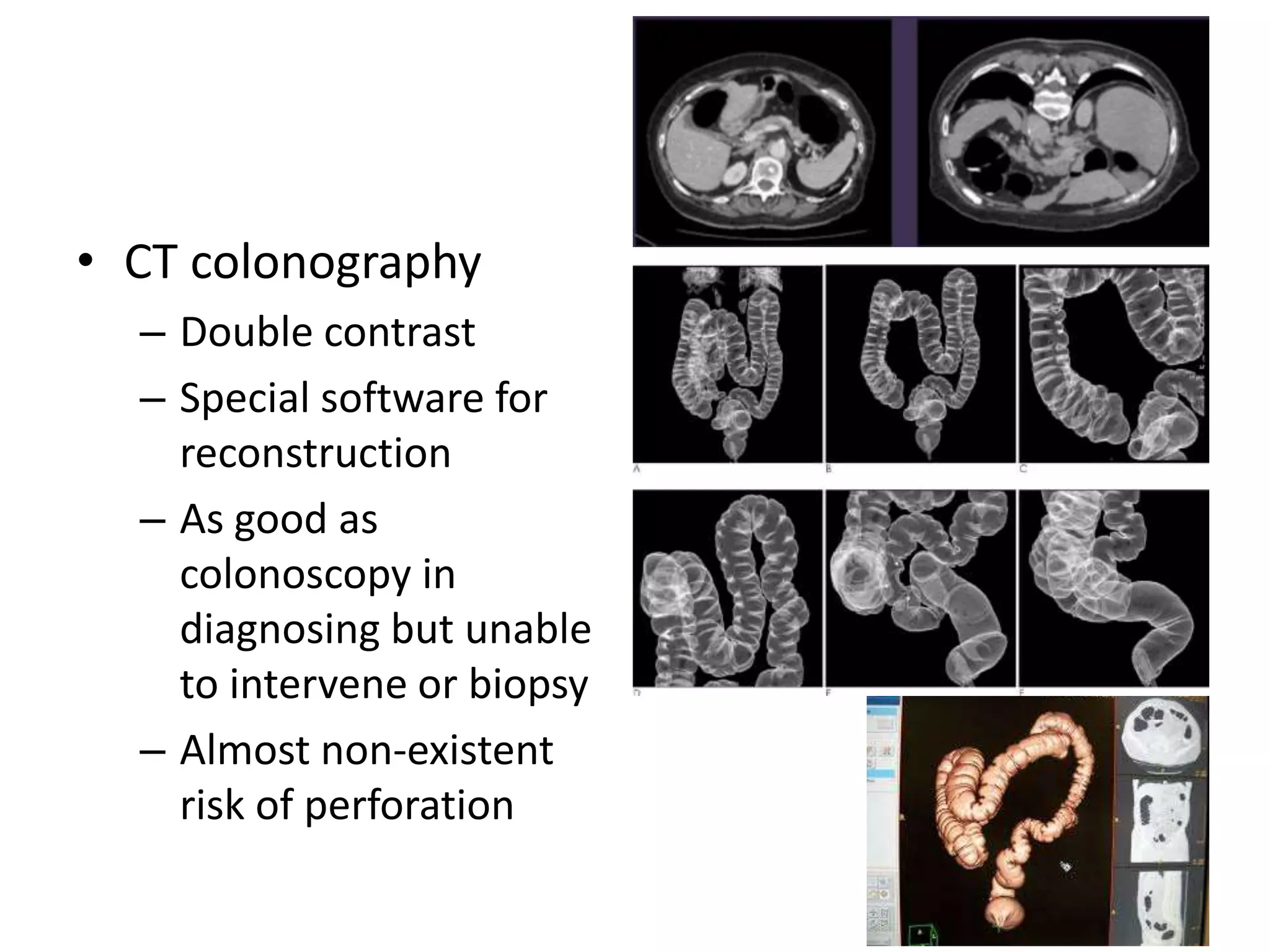
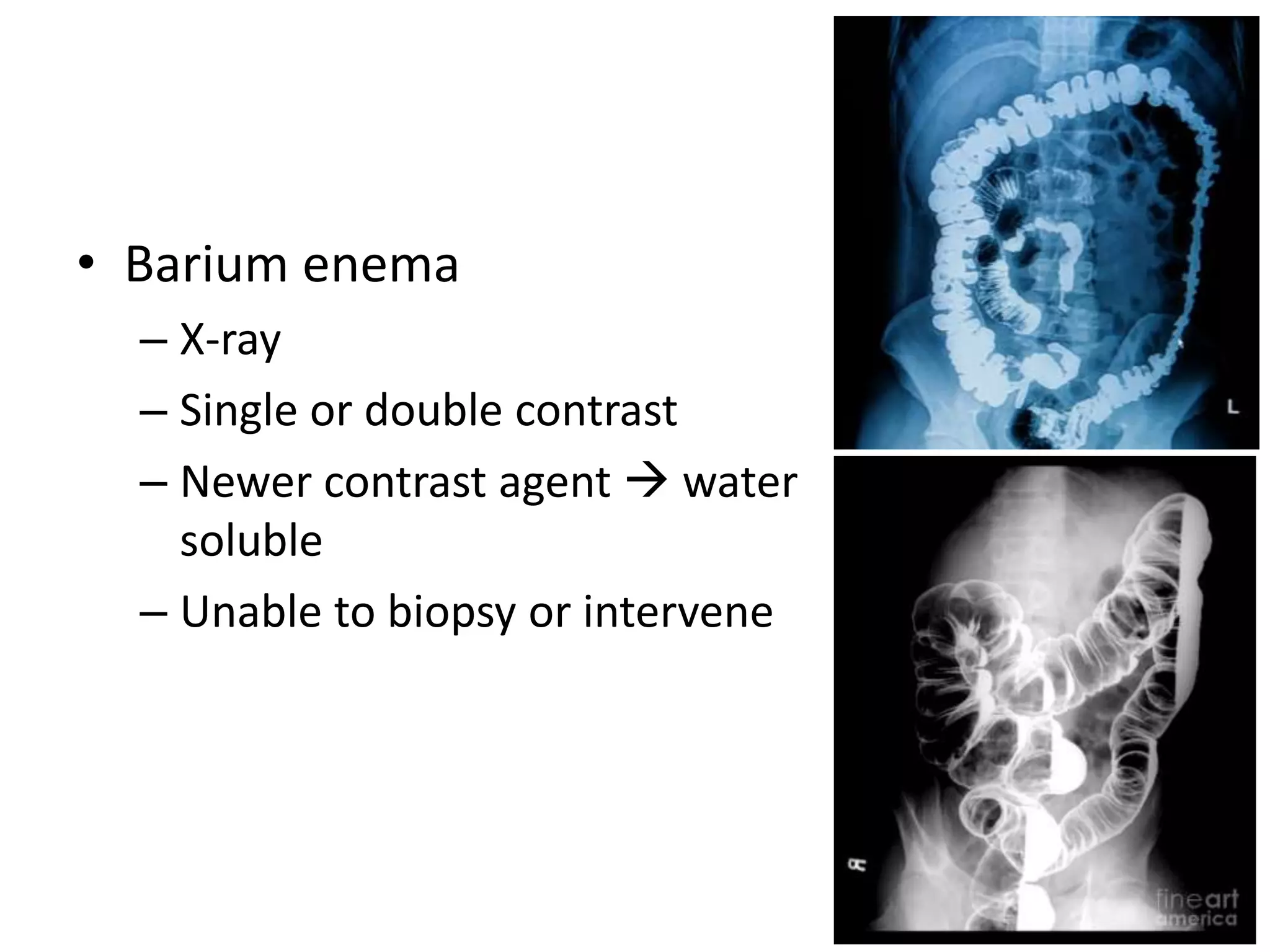
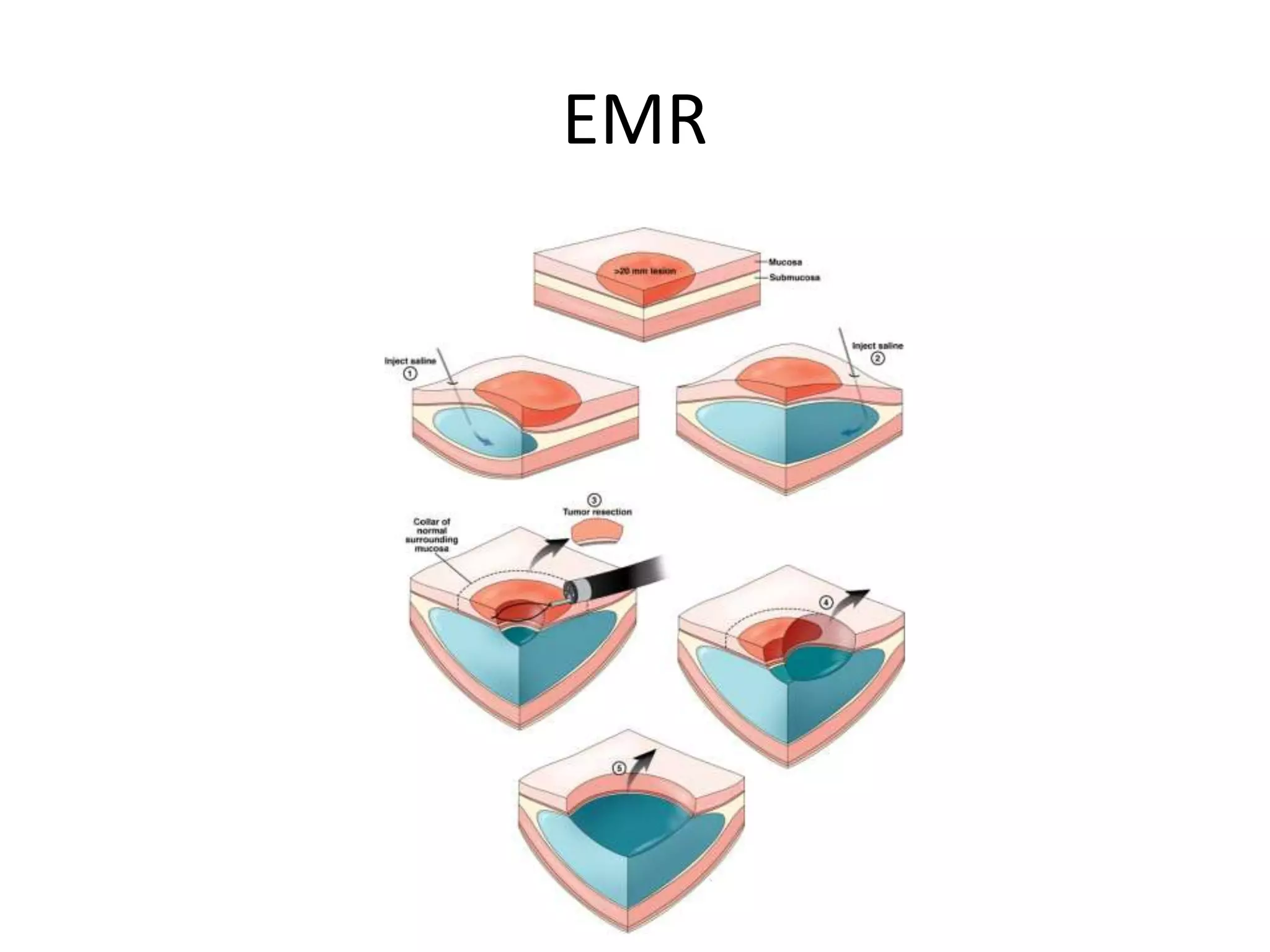
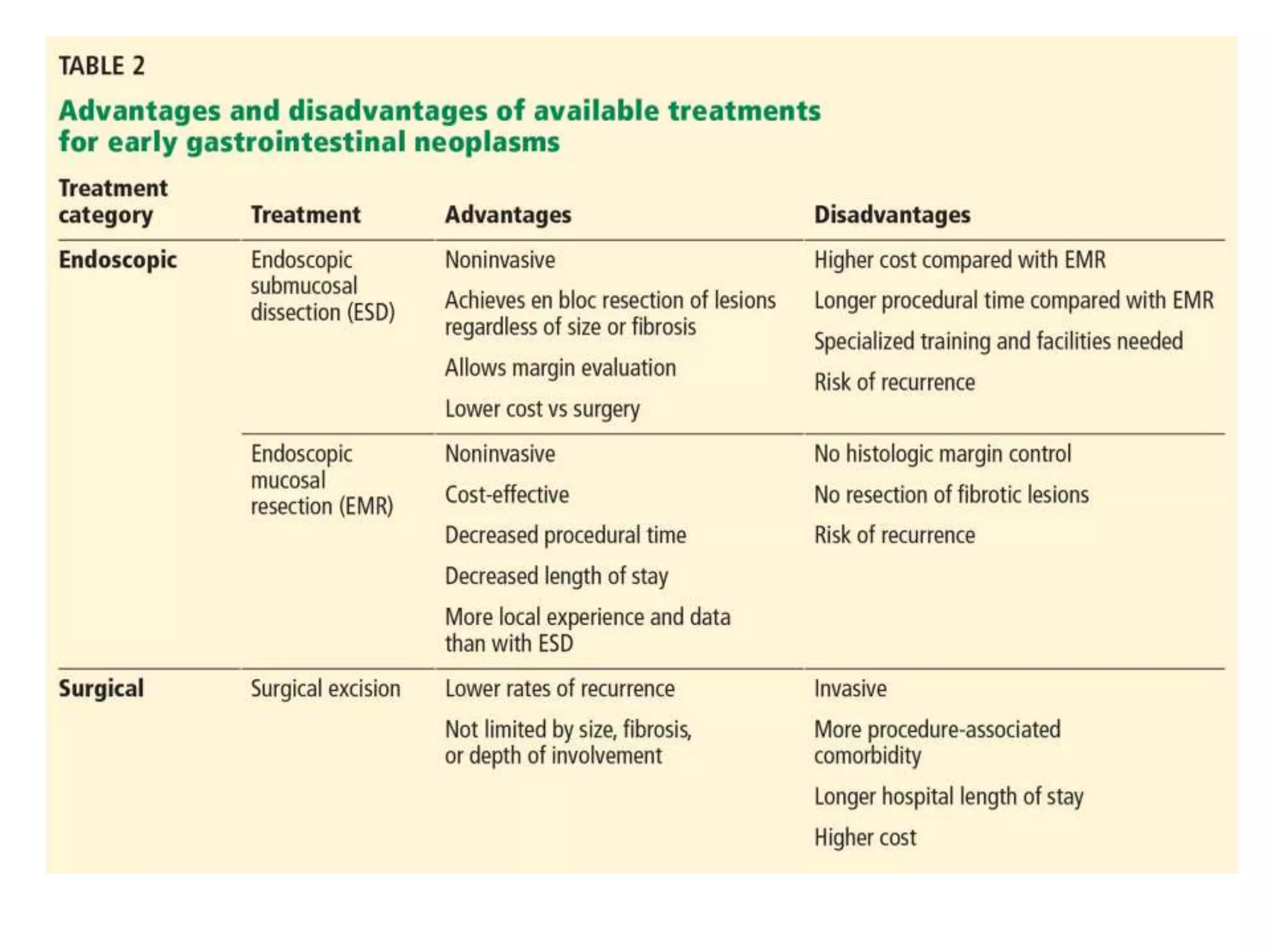
This document provides a comprehensive overview of colorectal polyps, detailing their definition, classification (anatomical, morphological, histological), and the associated risk of malignancy. It outlines the clinical features, diagnostic methods (like colonoscopy and CT colonography), and management strategies, including endoscopic and surgical options. Emphasis is placed on identifying neoplastic versus non-neoplastic types and their implications for treatment and cancer risk.