1. Chronic diarrhea is defined as persistent changes in stool consistency and increased stool frequency lasting over 4 weeks.
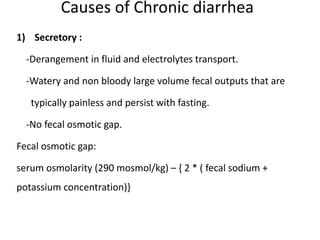
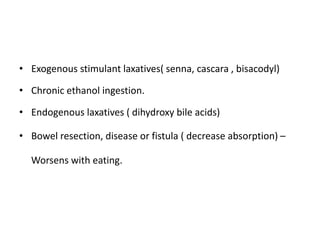
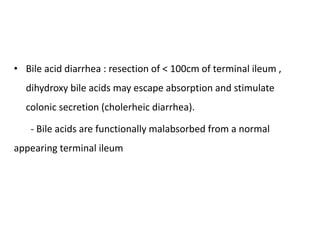
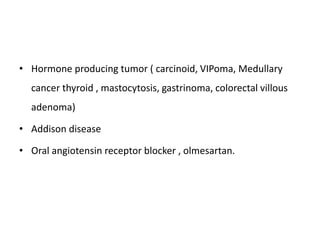
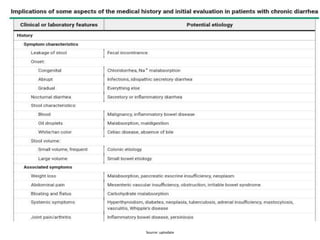
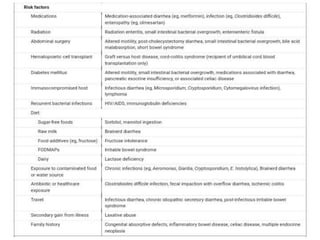
2. The causes of chronic diarrhea include secretory, osmotic, steatorrheal, inflammatory, dysmotility, and iatrogenic factors.
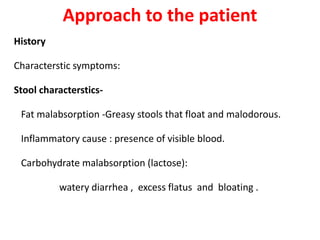
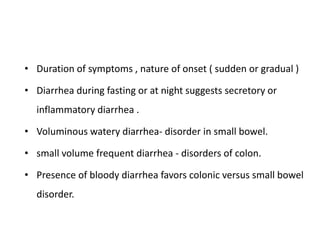
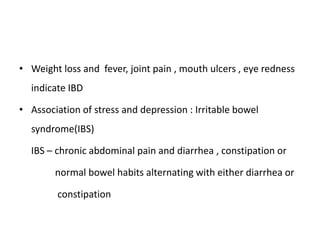
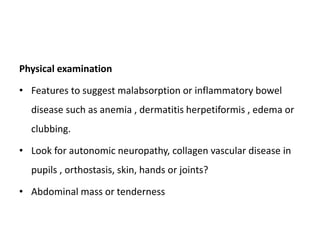
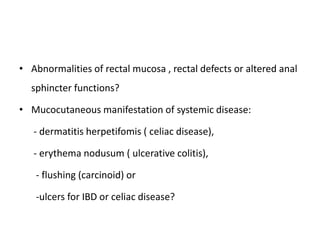
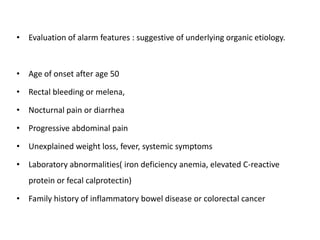
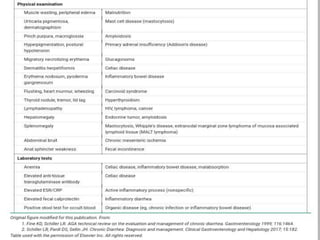
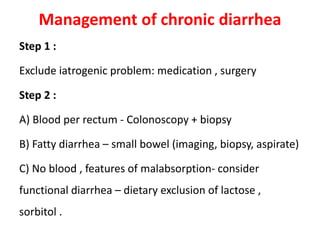
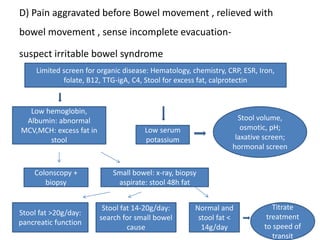
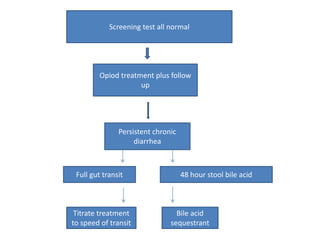
3. The approach to a patient with chronic diarrhea involves obtaining a detailed history and physical exam, followed by screening tests and further testing depending on the results to identify the underlying cause and guide management.