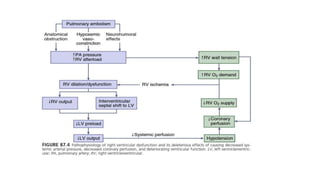
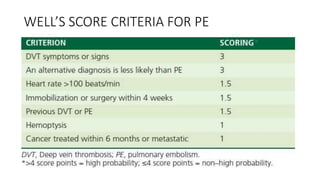
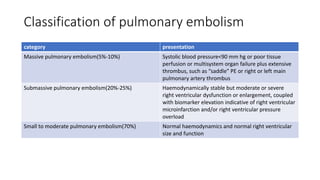
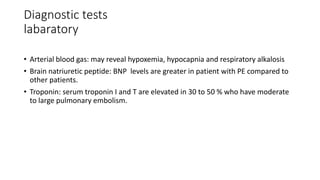
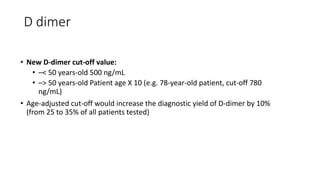
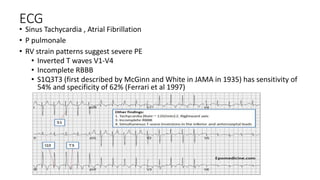
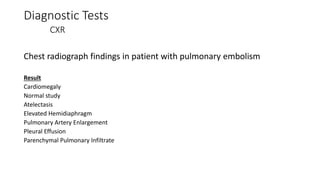
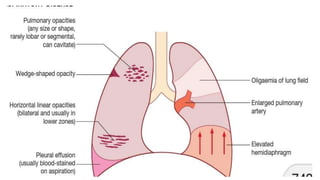
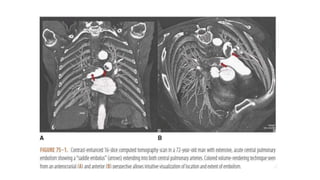
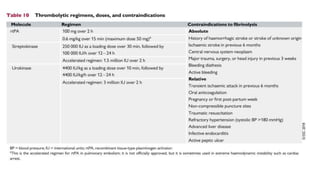
Pulmonary embolism (PE) occurs when a blood clot forms in the veins (usually in the legs) and travels to the lungs. It can be life-threatening and is a major cause of hospital deaths. Risk factors include prolonged bed rest, recent surgery, cancer, and certain genetic conditions. Symptoms may include sudden shortness of breath, chest pain, and coughing up blood. Diagnosis involves blood tests, imaging like CT scans, and assessment of clinical probability based on risk factors and symptoms. Treatment depends on severity but typically involves blood thinners, oxygen supplementation, and in some cases thrombolysis or surgery to break up clots. Preventing recurrence requires identifying risk factors and continuing anticoag
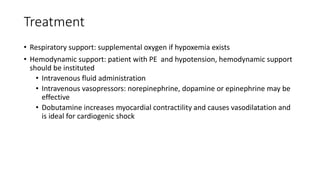
![Treatment
Initiation of anticoagulation therapy
• Anticoagulation - parenteral anticoagulation [unfractionated heparin (UFH), low molecular
weight heparin (LMWH), or fondaparinux] over the first 5–10 days
• Parenteral heparin should overlap with the initiation of a vitamin K antagonist (VKA);
alternatively, it can be followed by administration of one of the new oral anticoagulants:
dabigatran or edoxaban. rivaroxaban or apixaban
• Oral treatment with one of these agents should be started directly or after a 1–2 day
administration of UFH, LMWH or fondaparinux
• In this latter case, acute-phase treatment consists of an increased dose of the oral
anticoagulant over the first 3 weeks (for rivaroxaban), or over the first 7 days (for apixaban)](https://image.slidesharecdn.com/peclassnursing-231129063838-a7c1070f/85/Pulmonary-Embolism-for-Nurses-pptx-26-320.jpg)