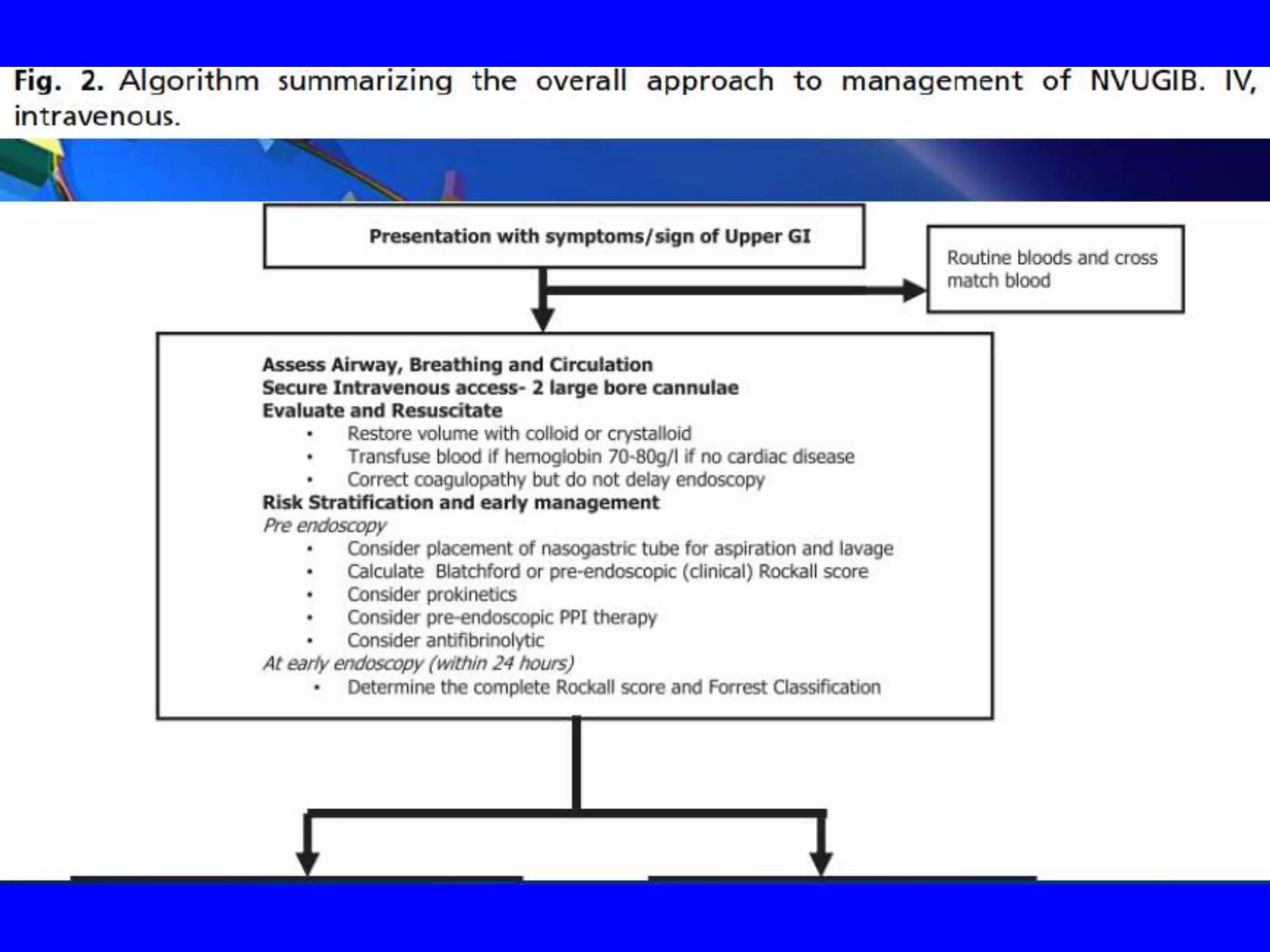
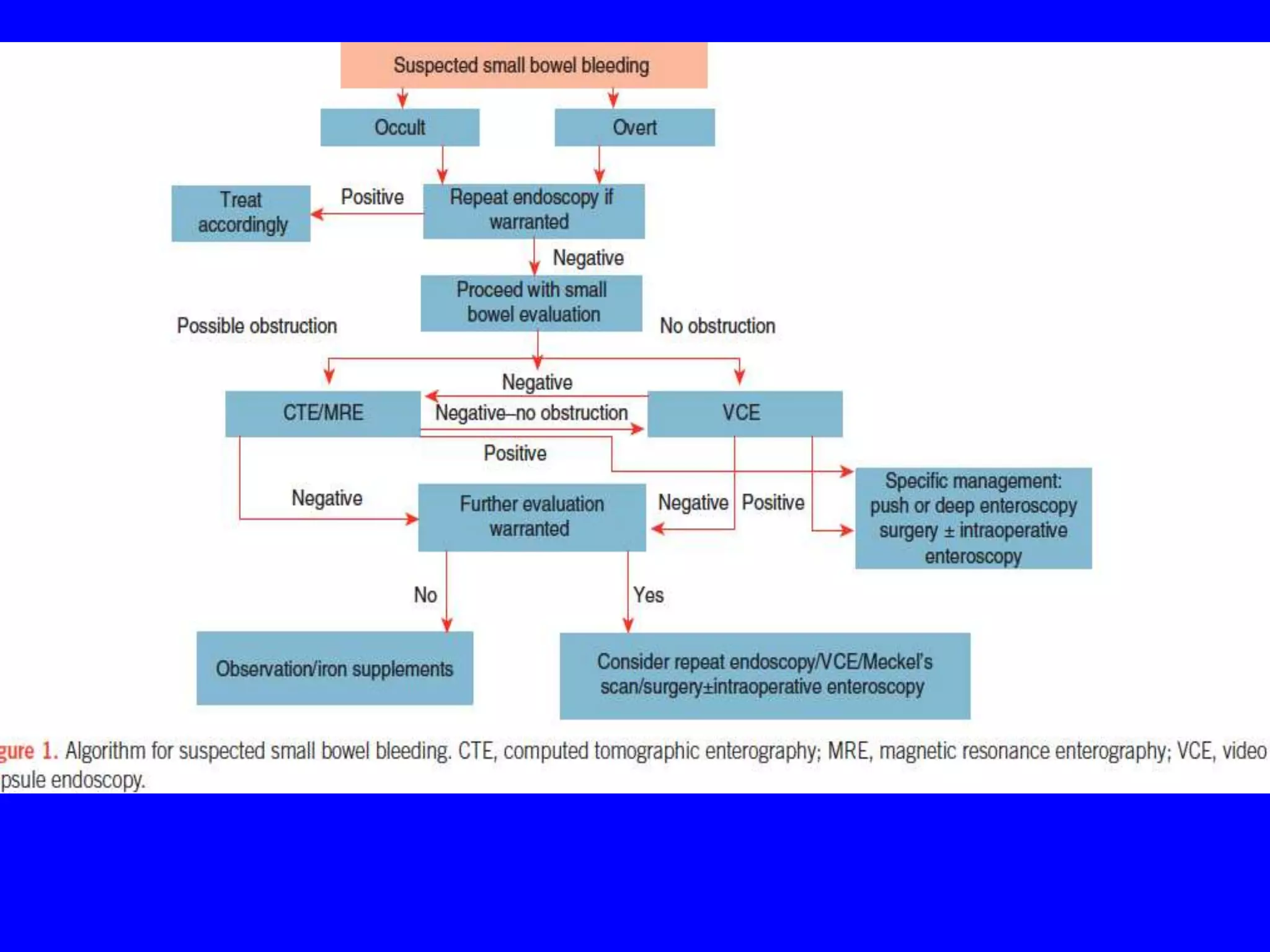
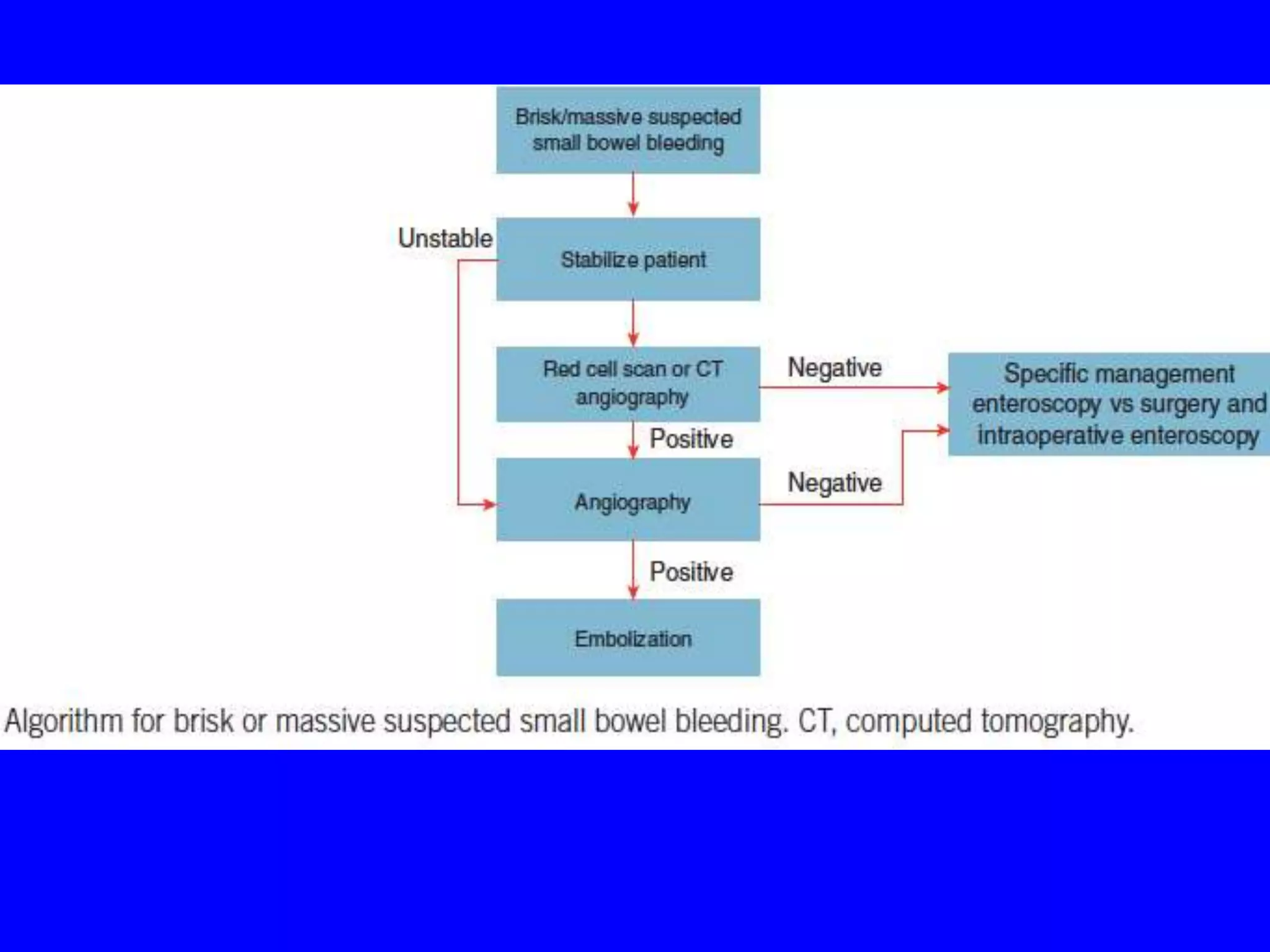
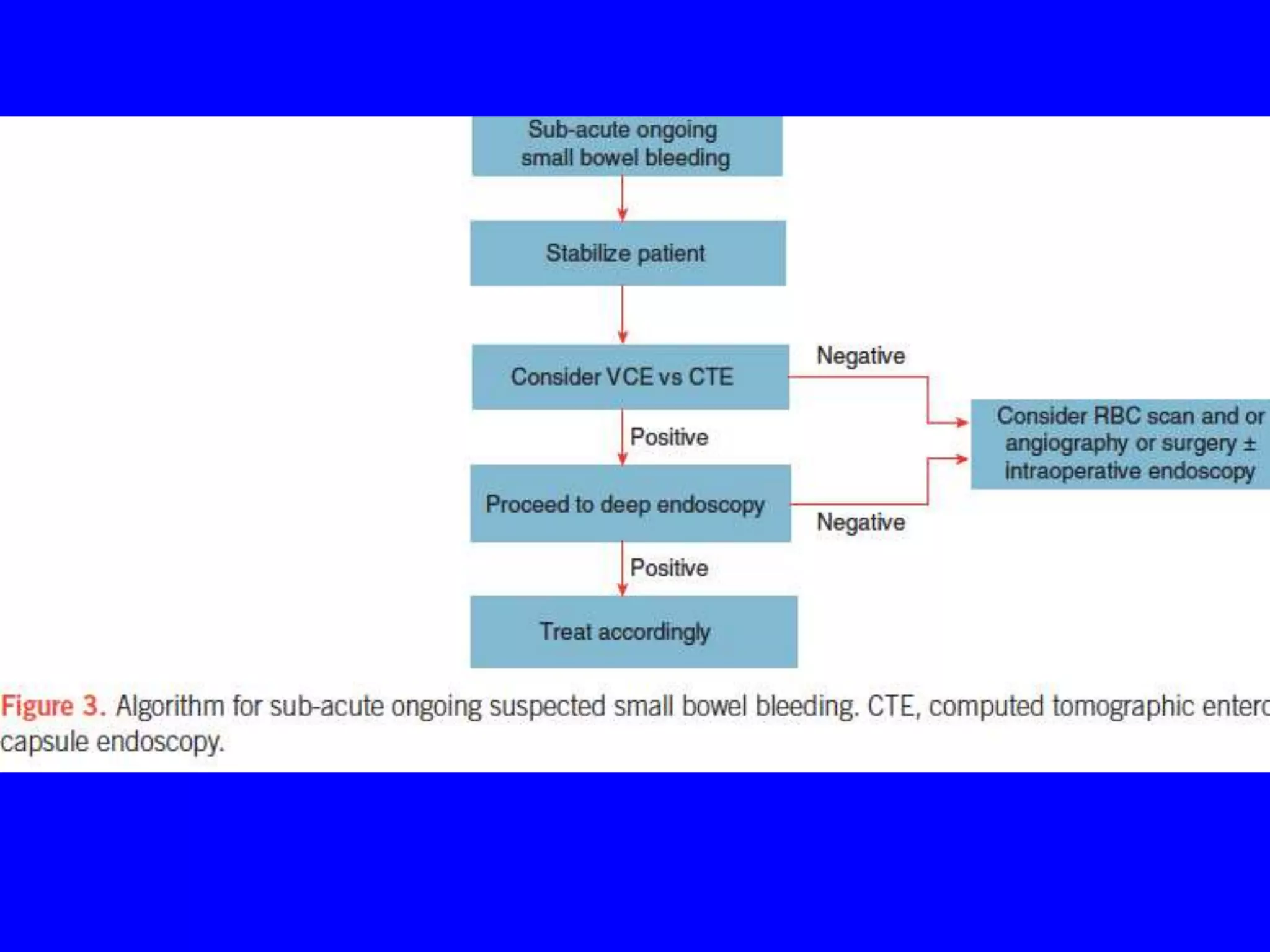
This document provides an overview of gastrointestinal bleeding (GIB), including the different types (upper, lower, small intestinal bleeding), typical causes, clinical presentations, evaluation, and management. Some key points:
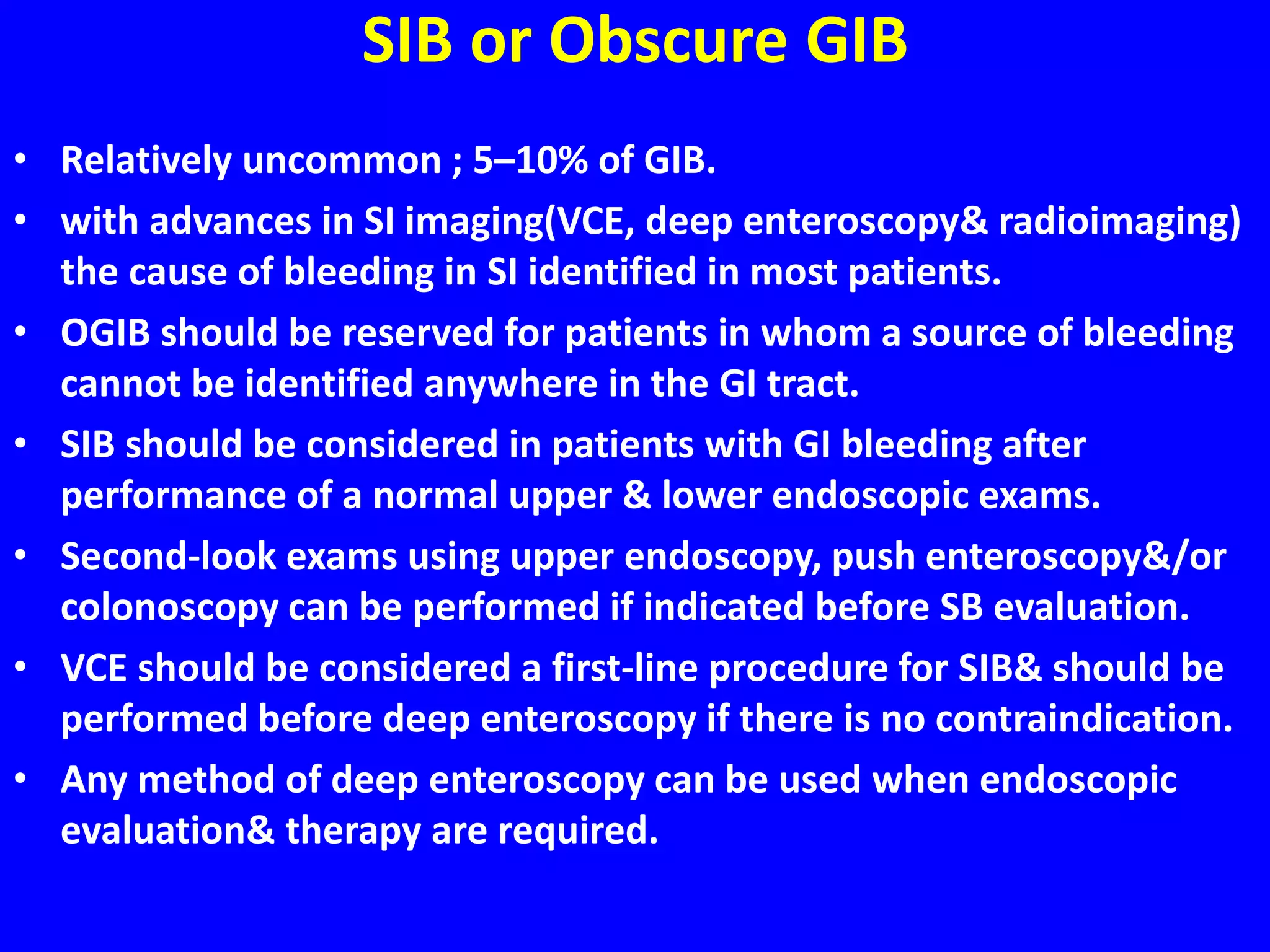
- Upper GIB is the most common type, accounting for 80% of cases, while small intestinal bleeding (SIB) is the least common at 5%.
- The most common presentations of upper GIB are melena (black tarry stool) and hematemesis (vomiting blood), while hematochezia (fresh red blood per rectum) is more typical of lower GIB.
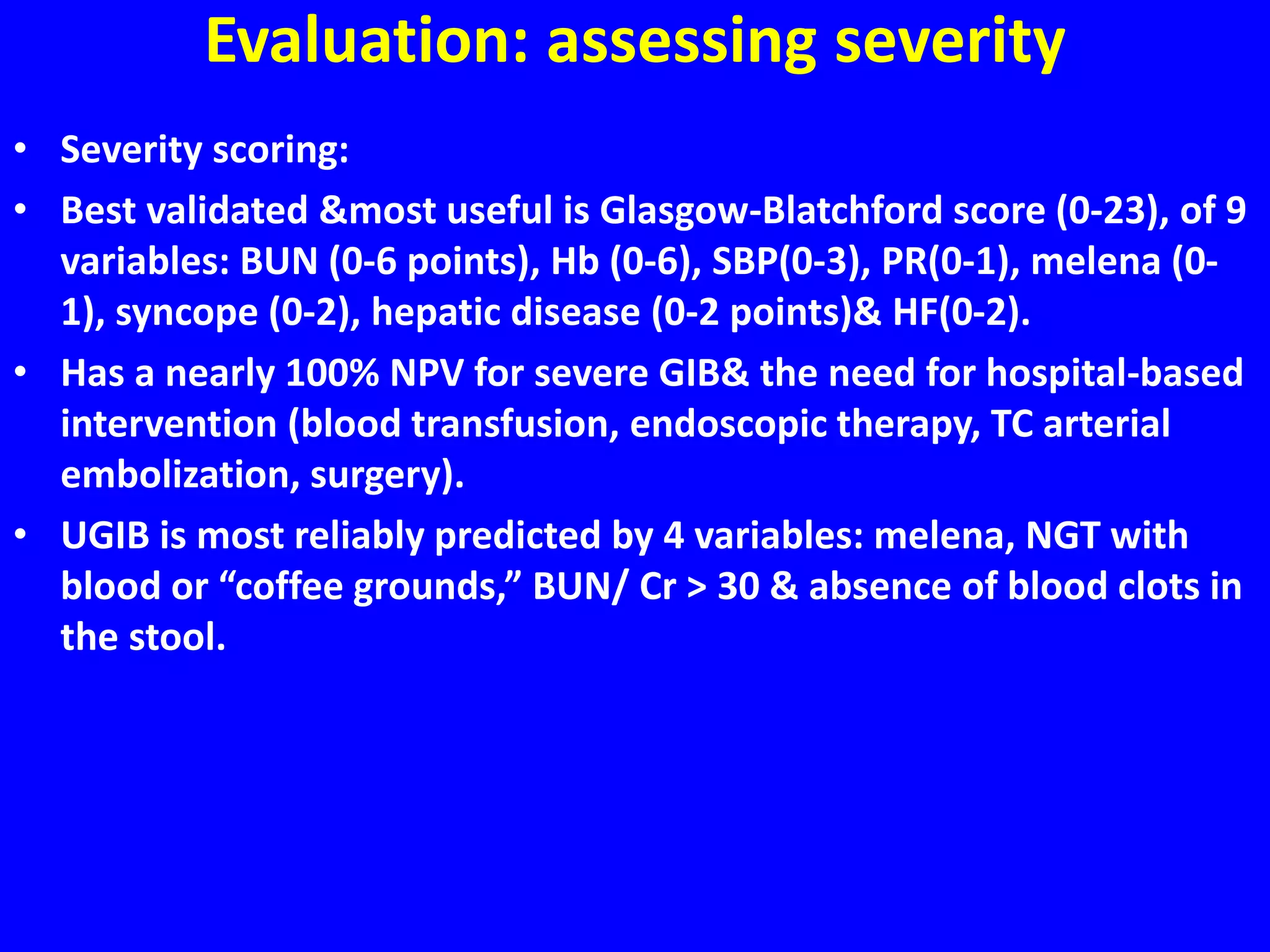
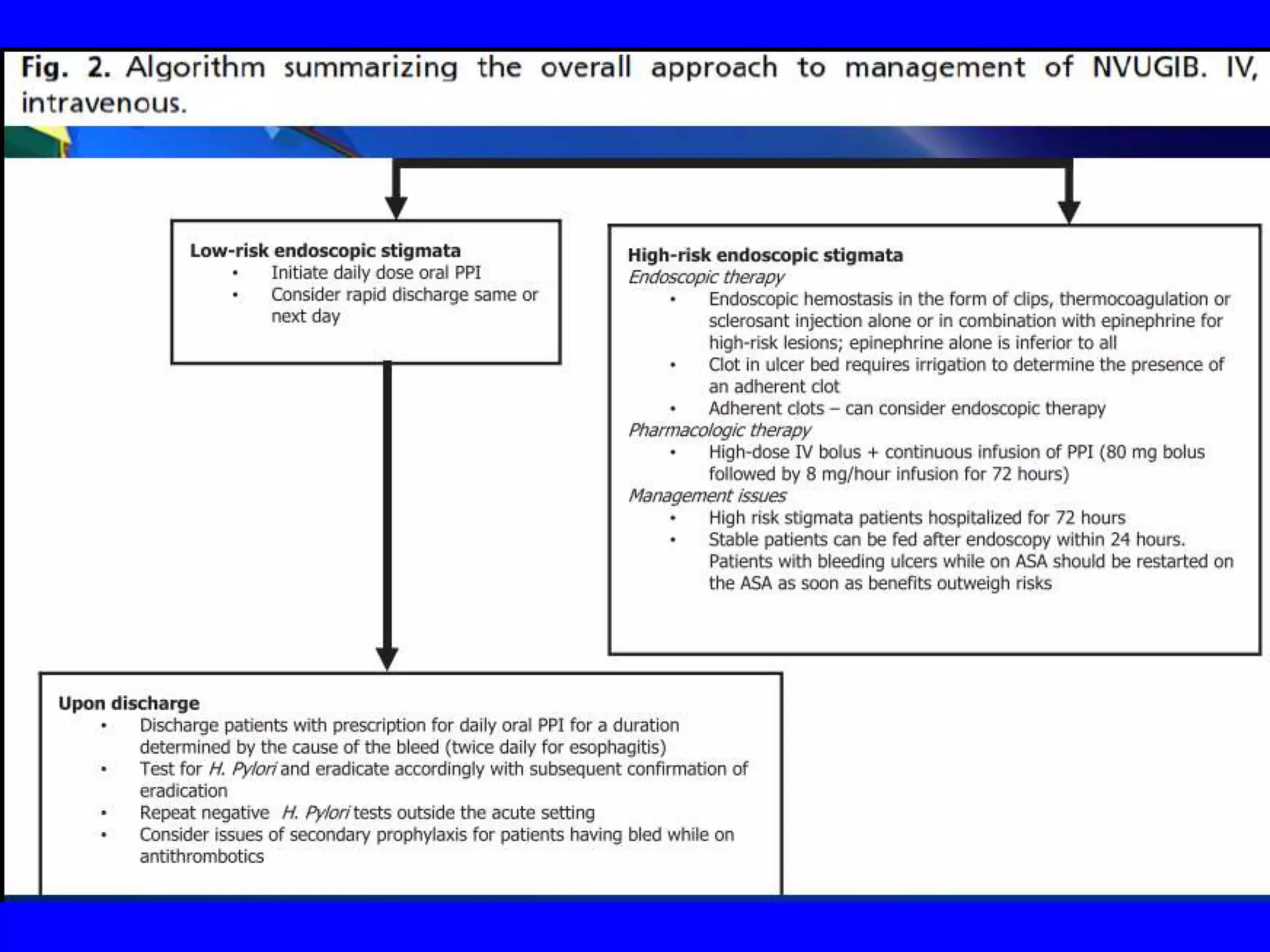
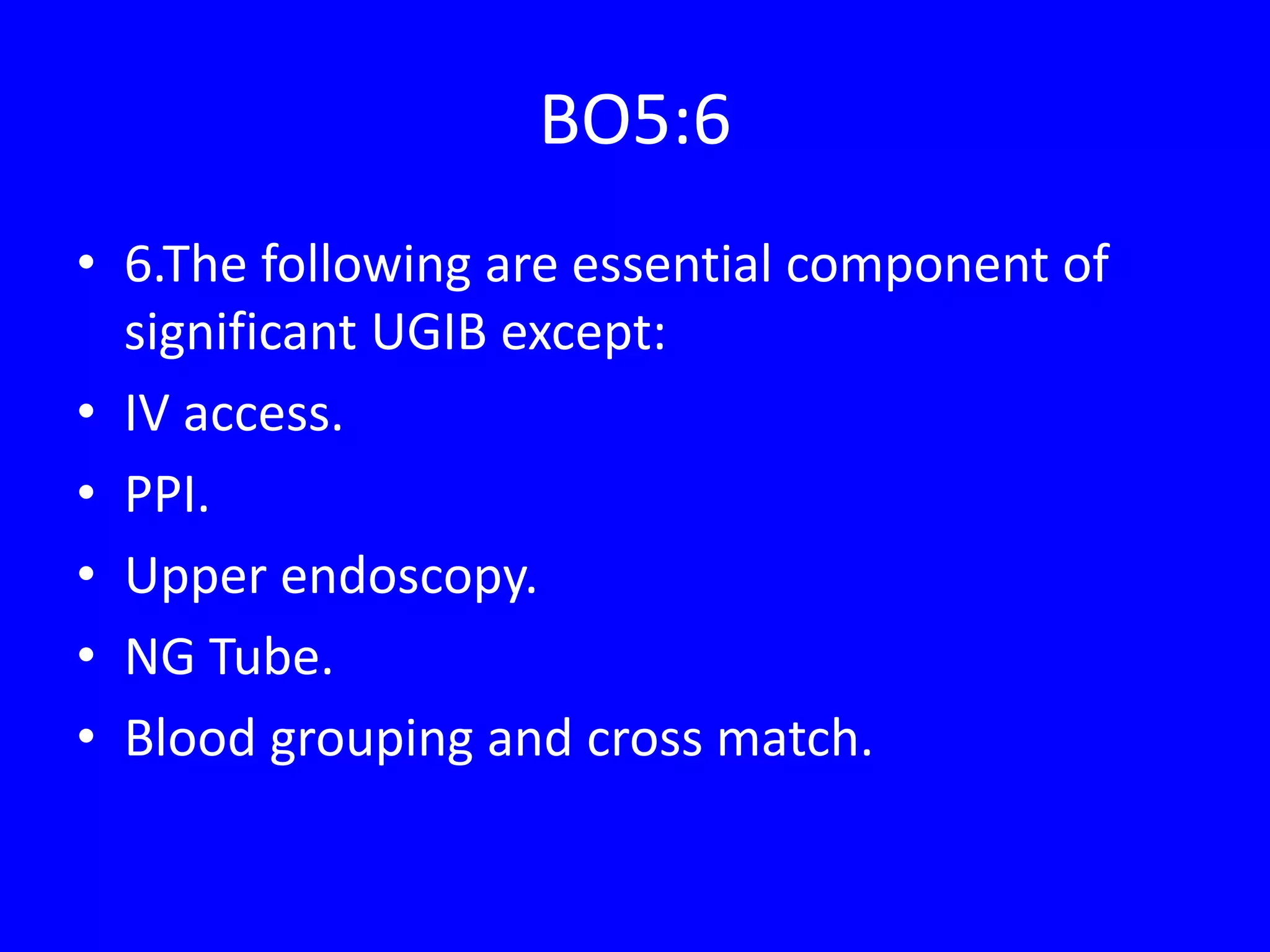
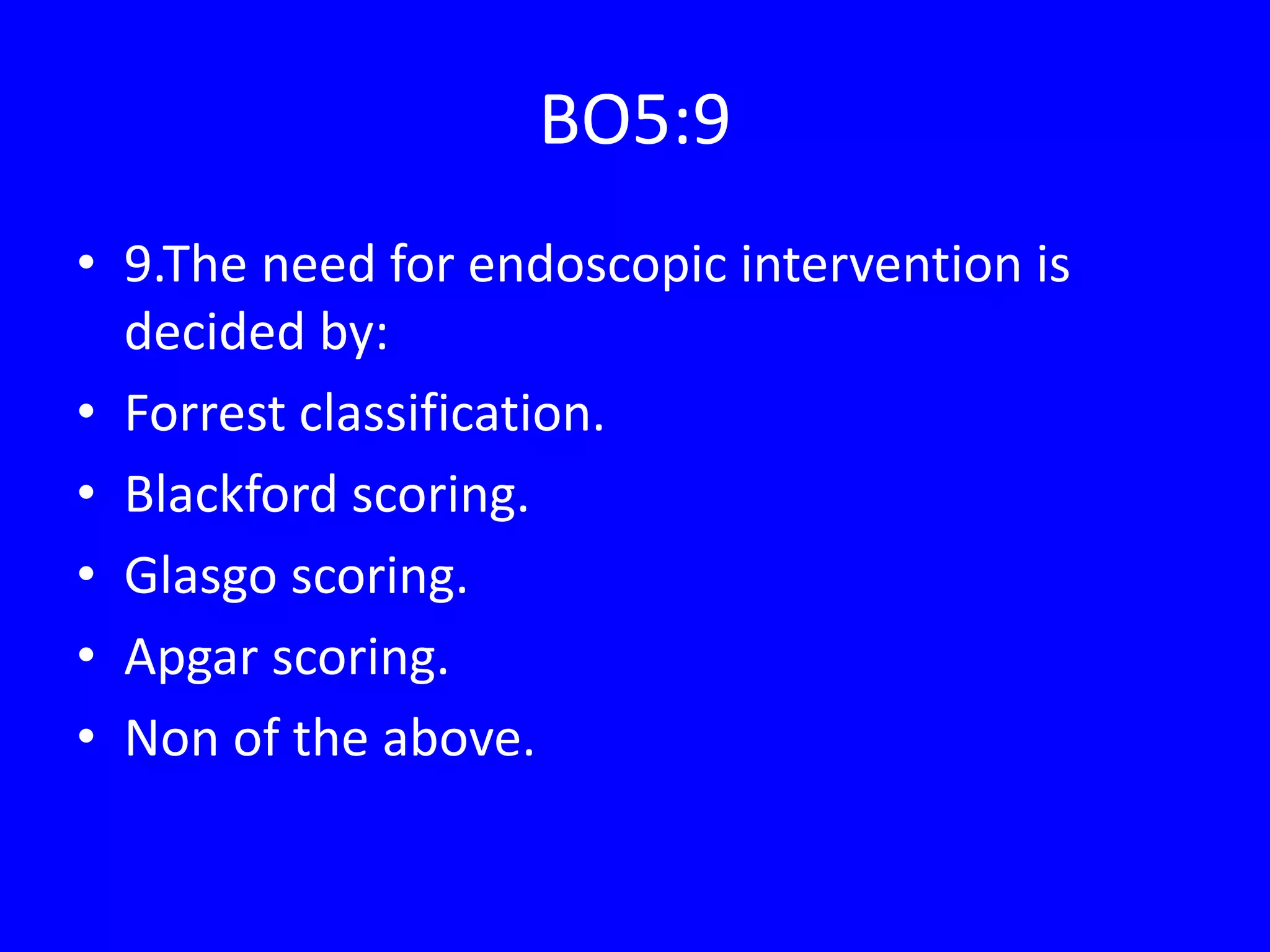
- Evaluation involves assessing severity using scoring systems like the Glasgow-Blatchford score to determine