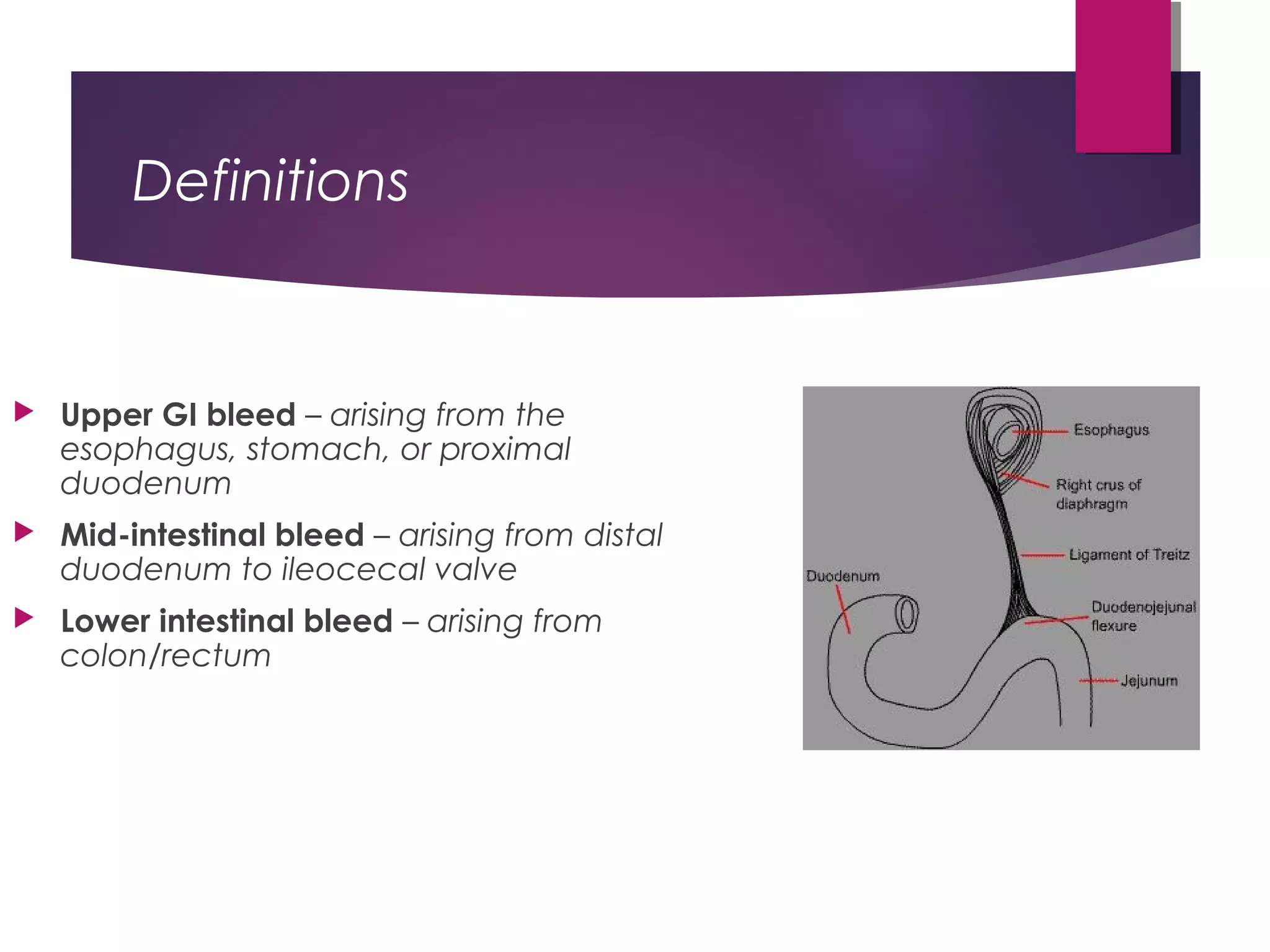
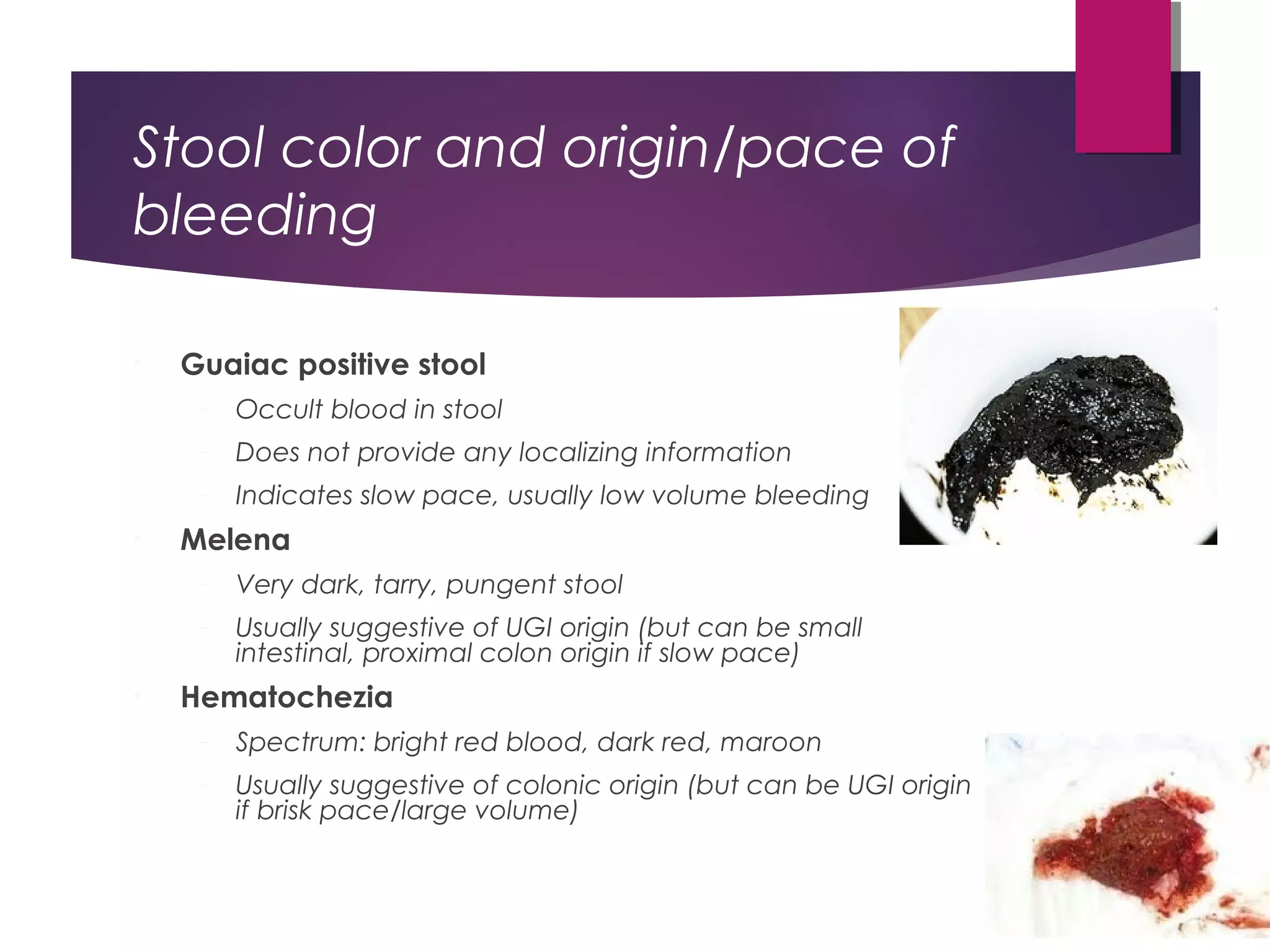
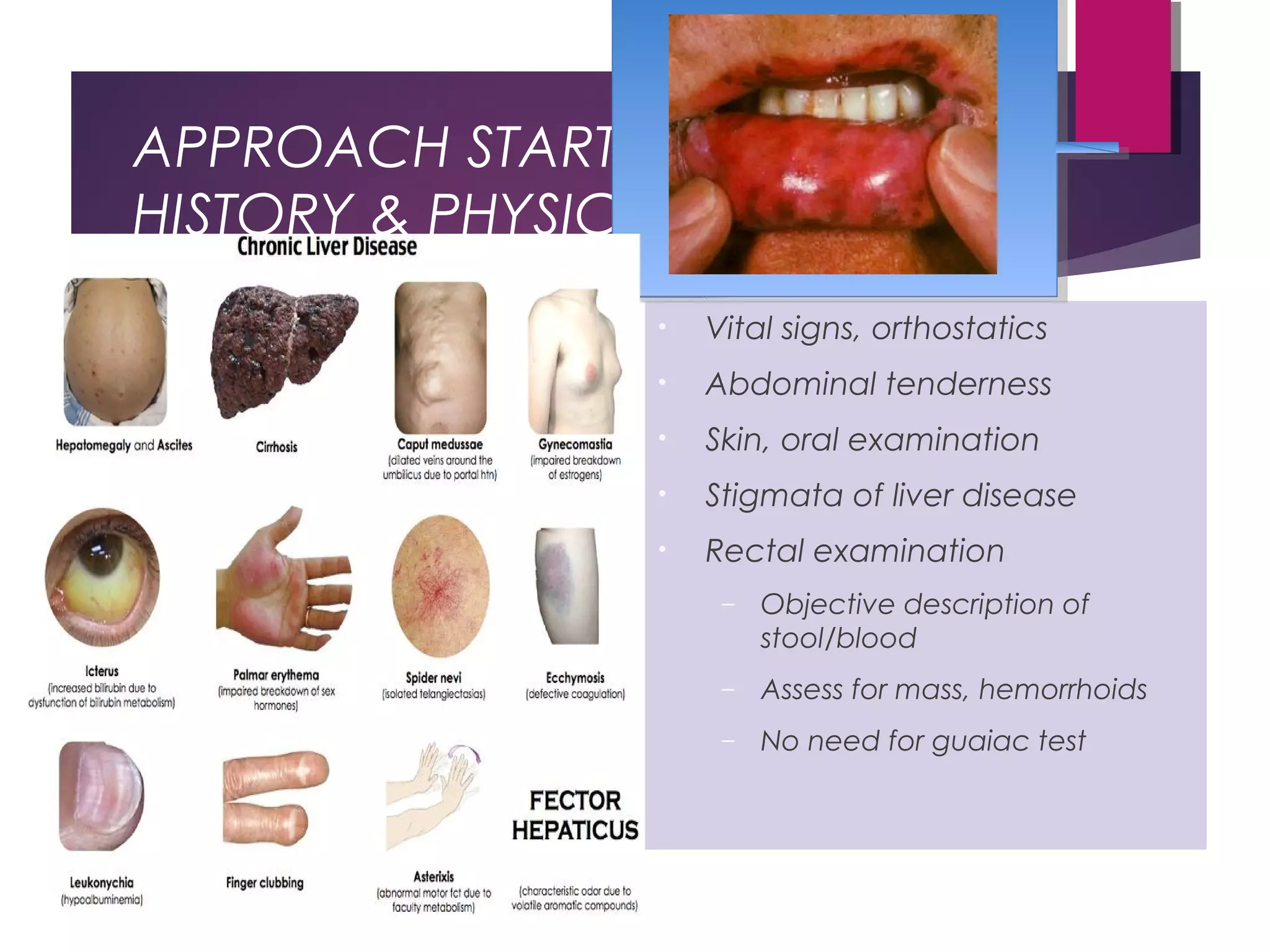
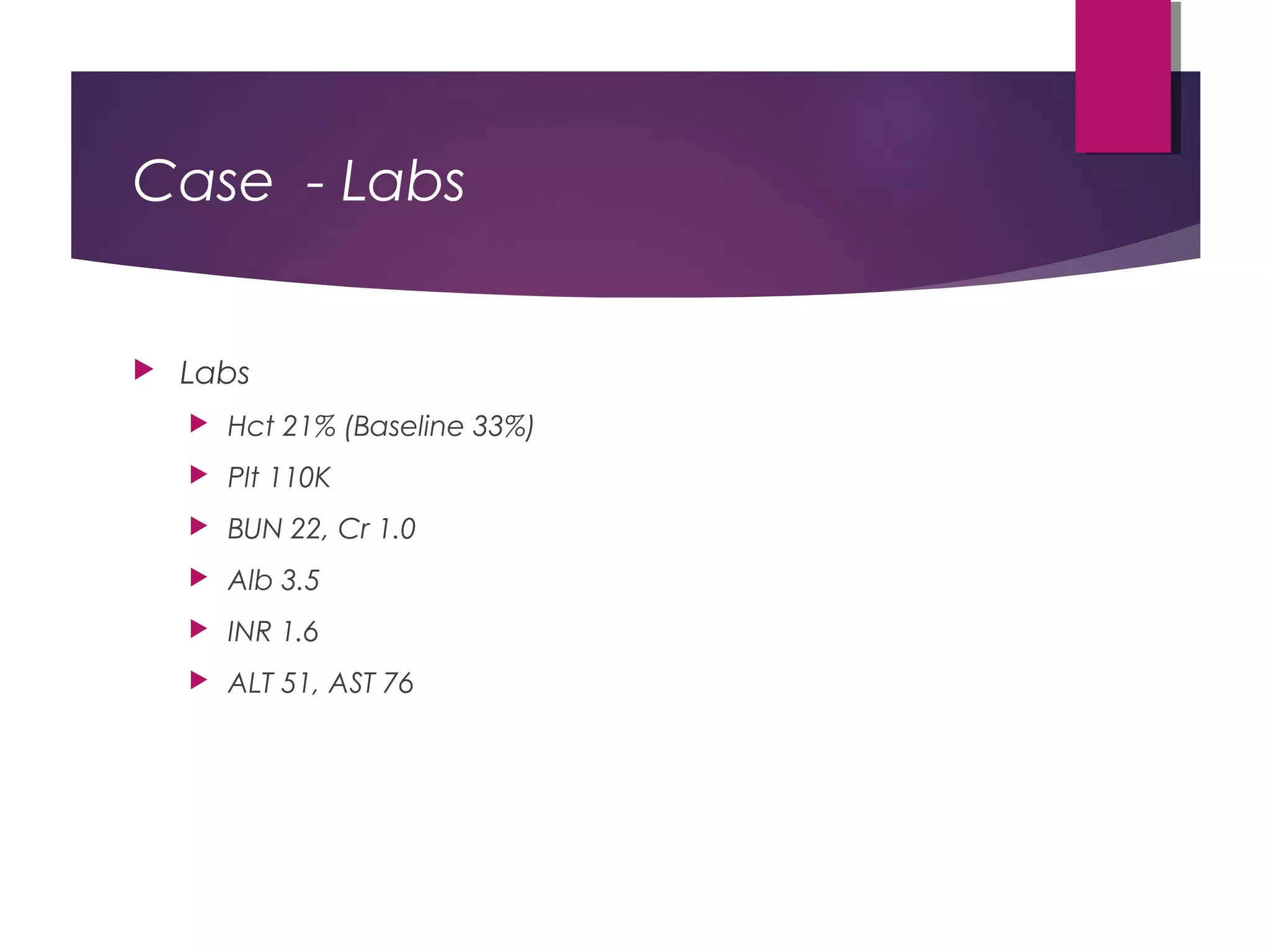
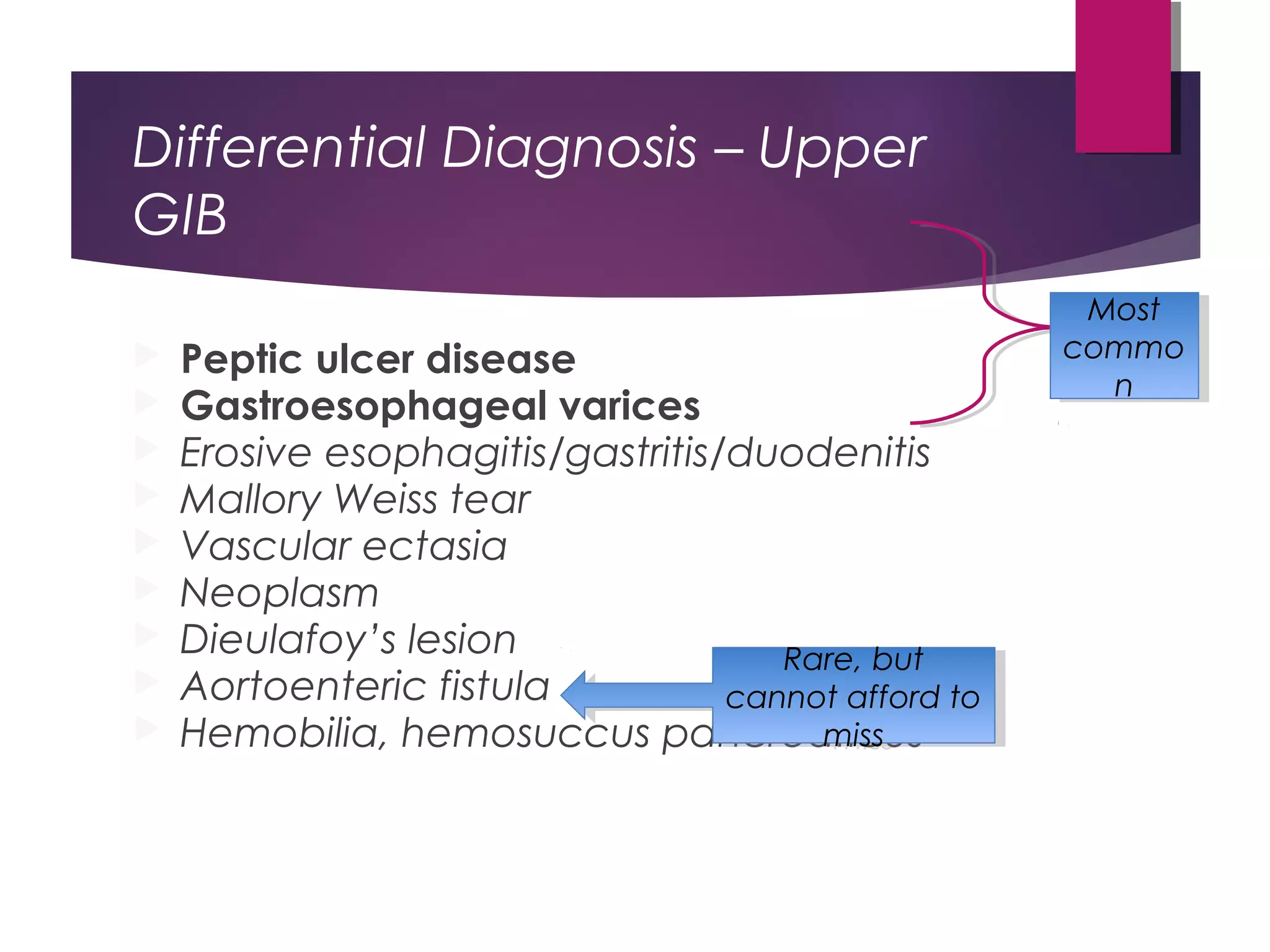
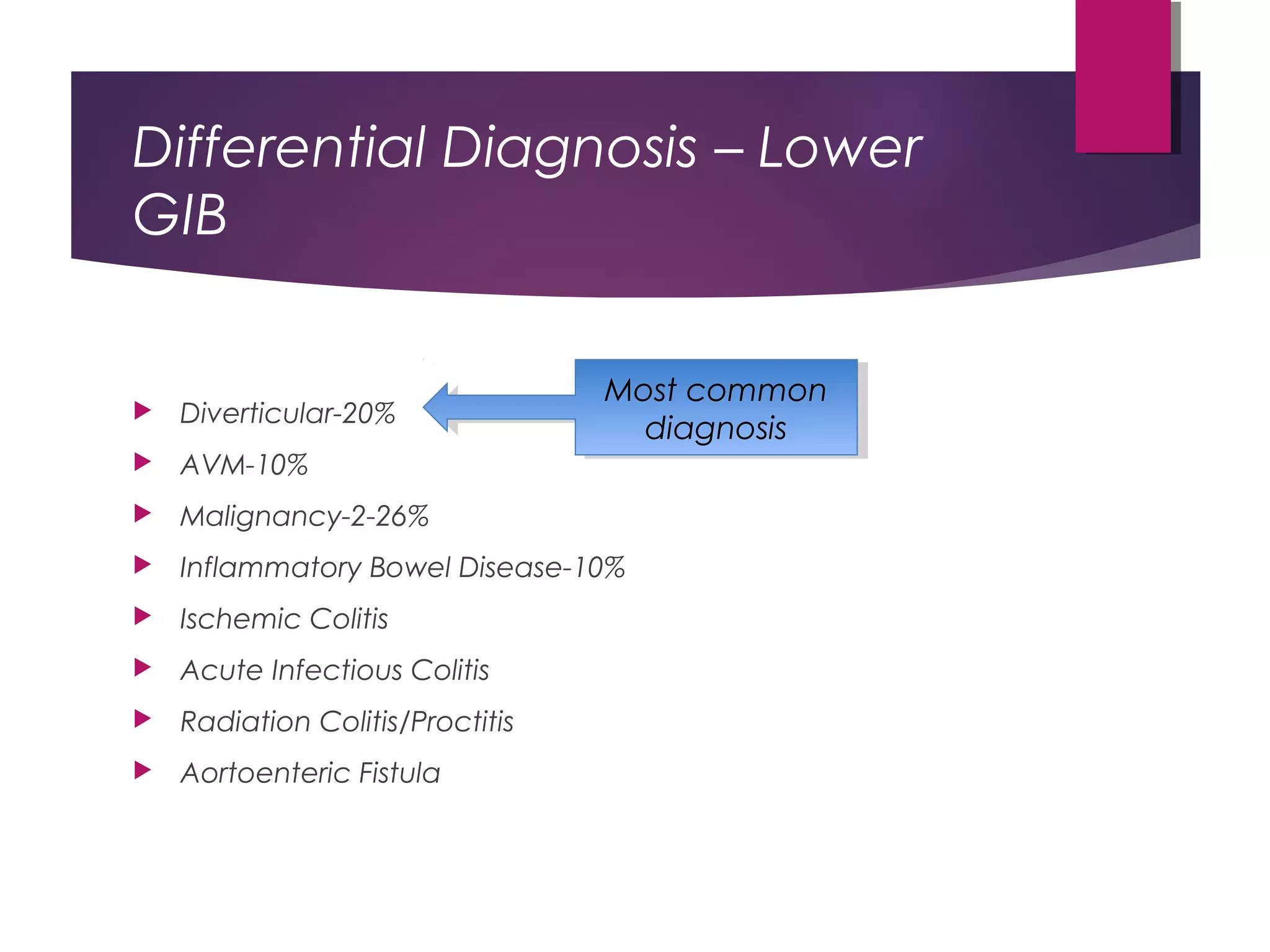
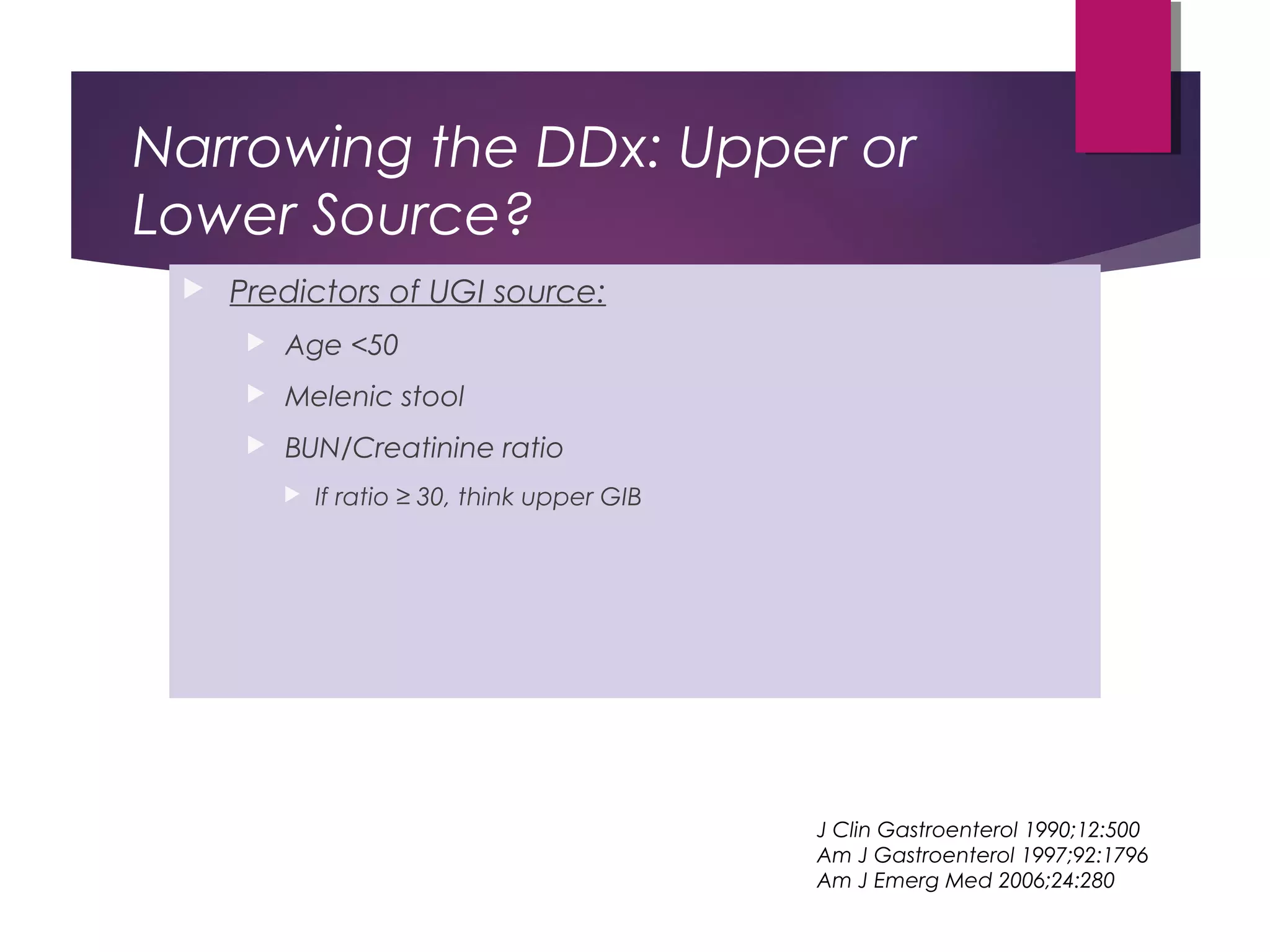
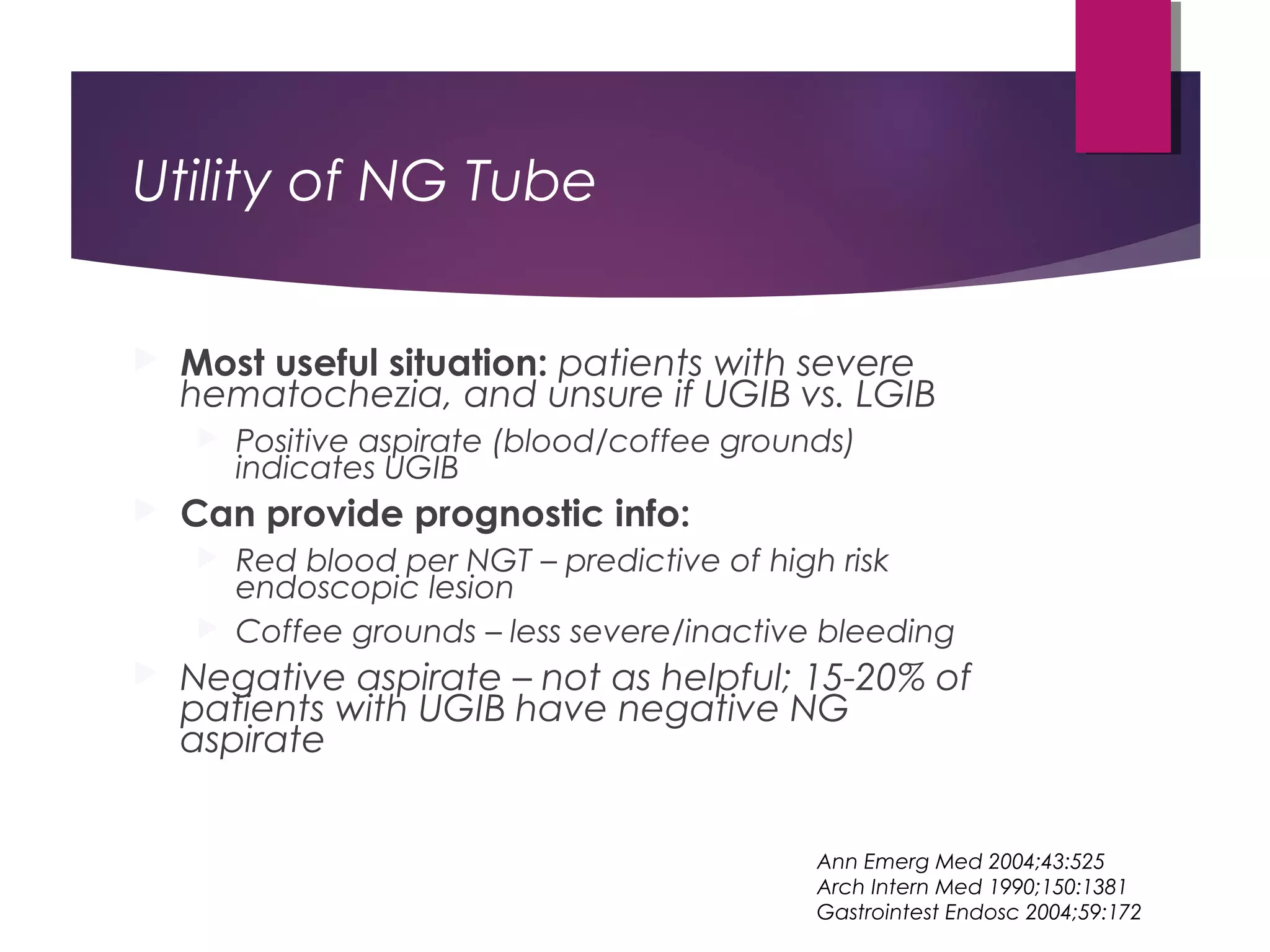
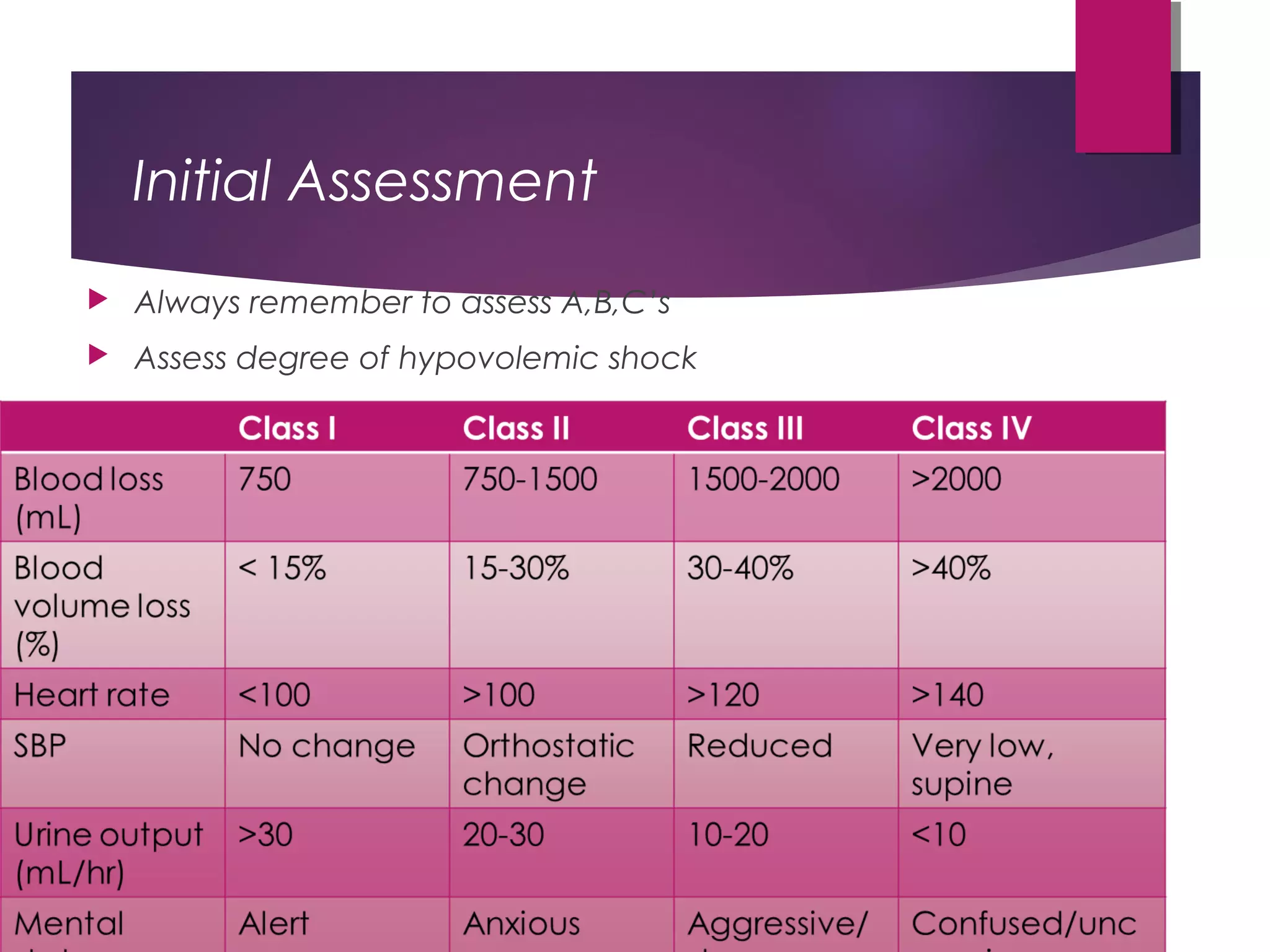
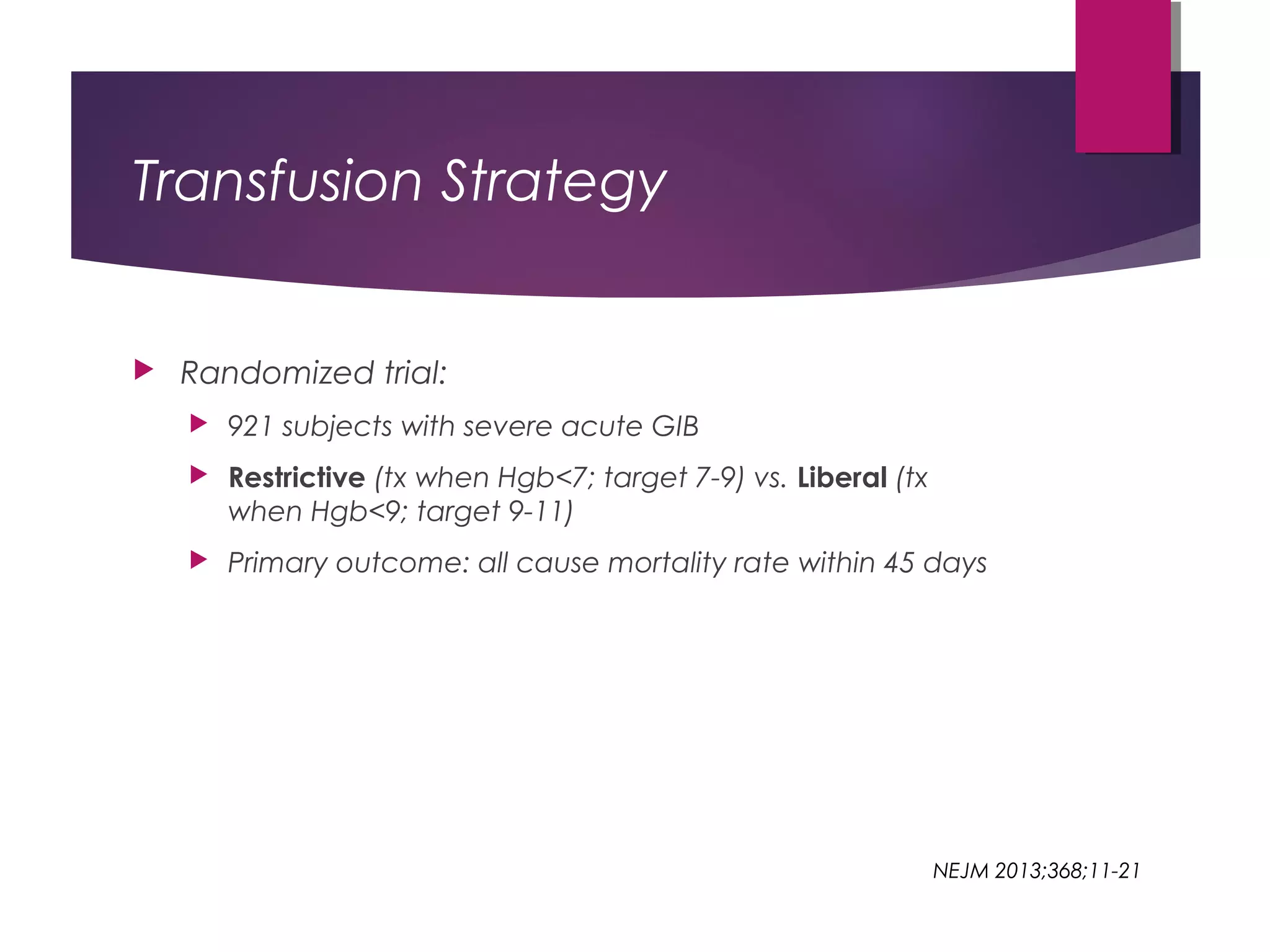
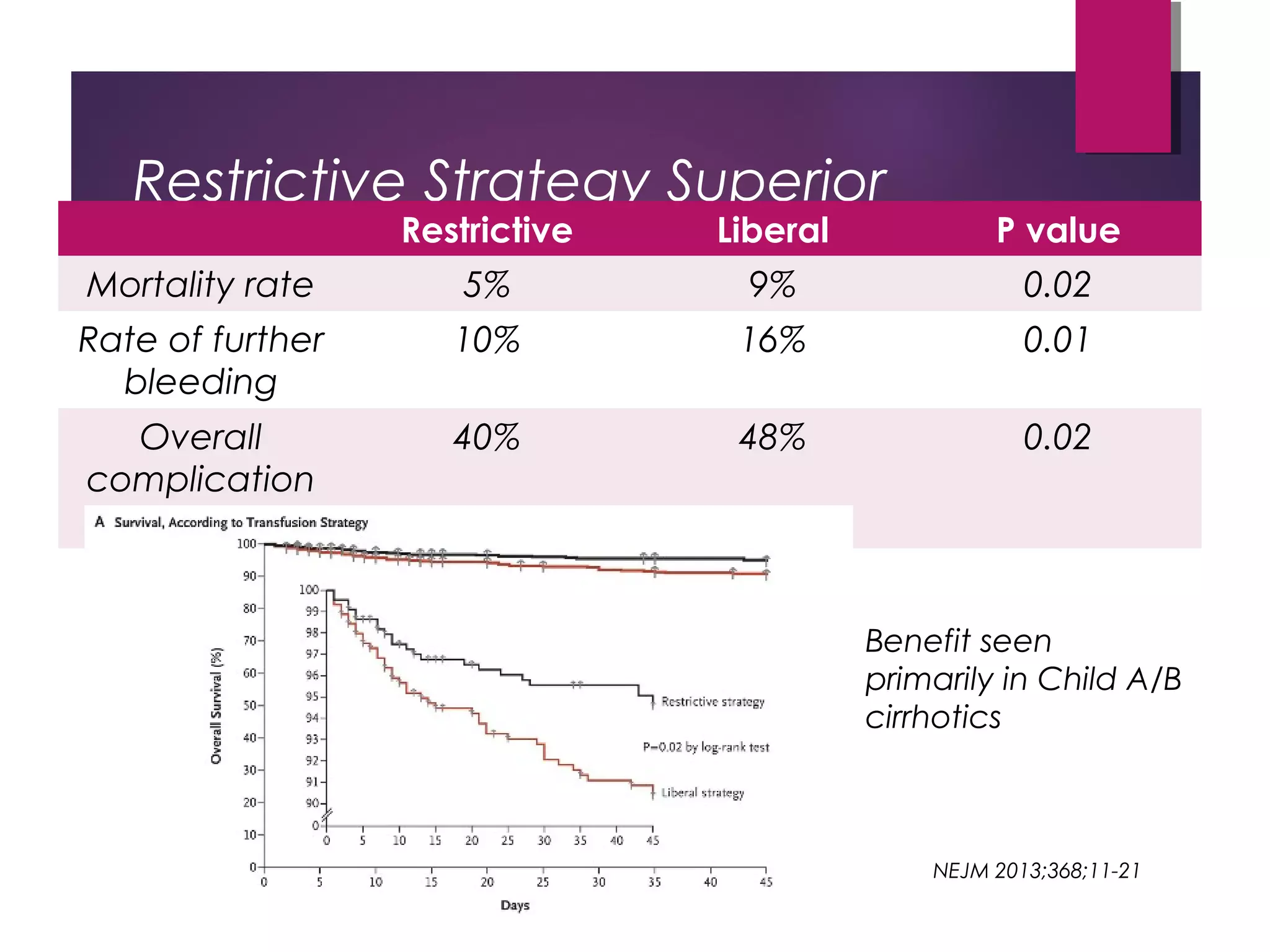
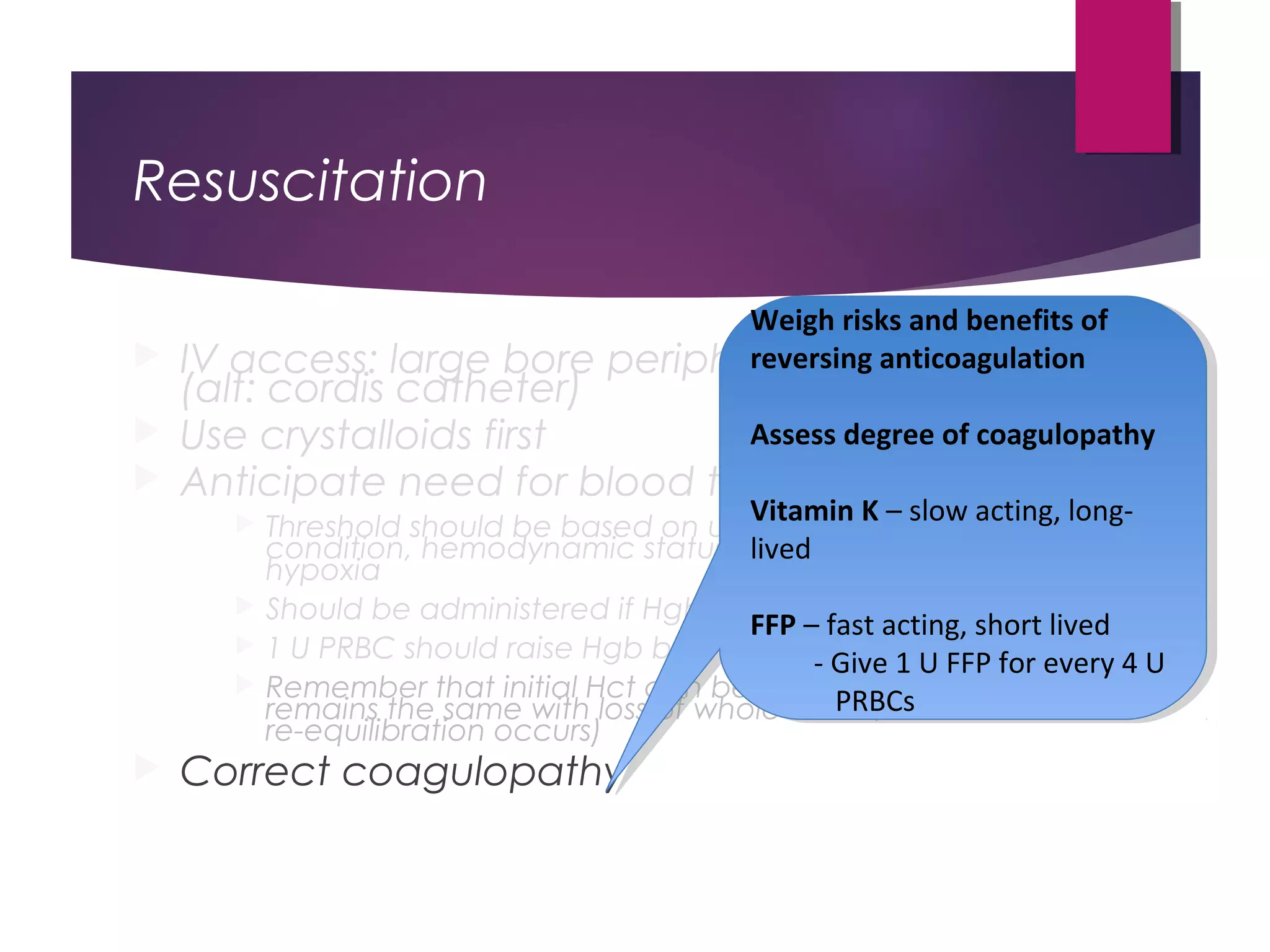
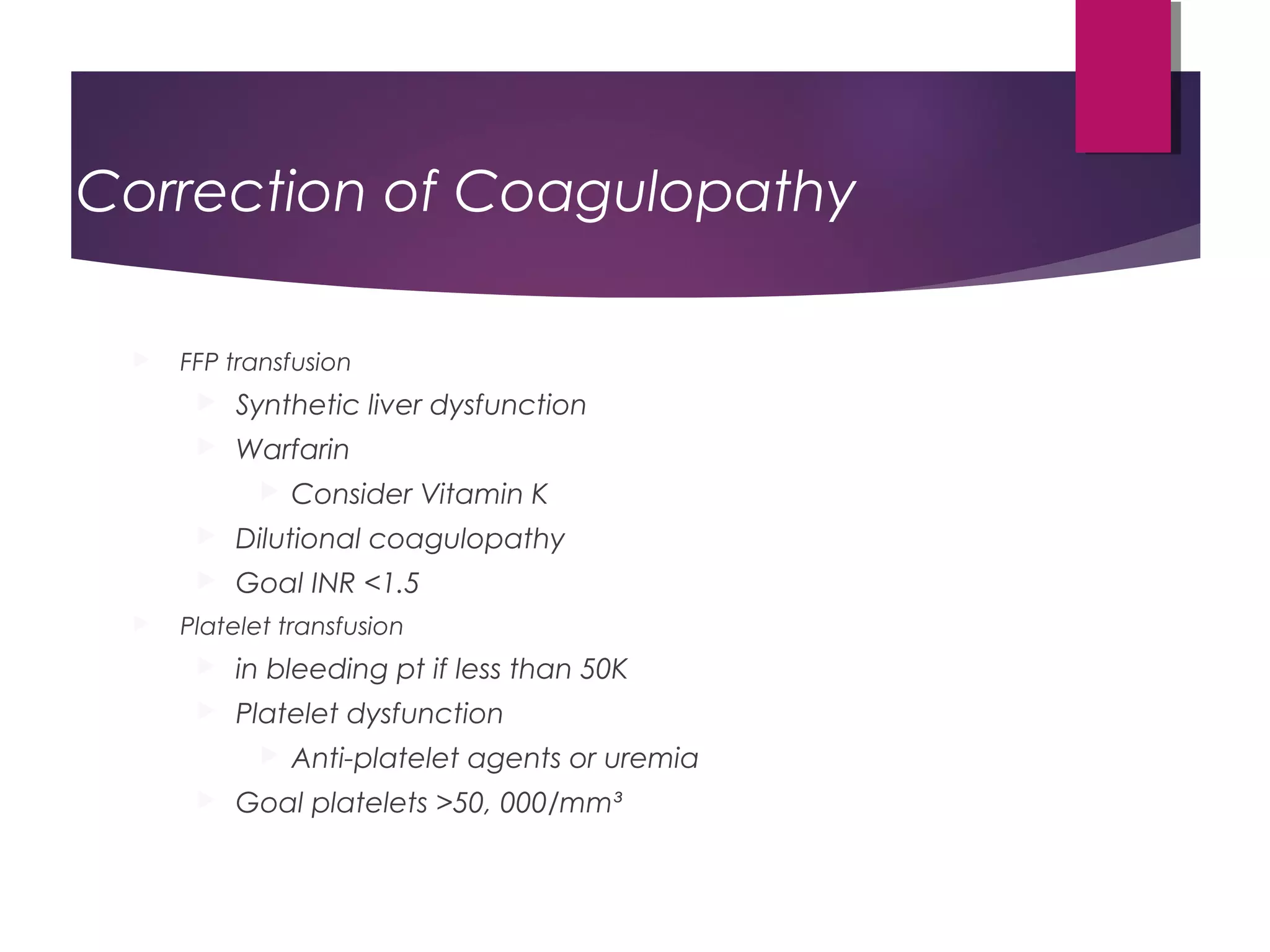
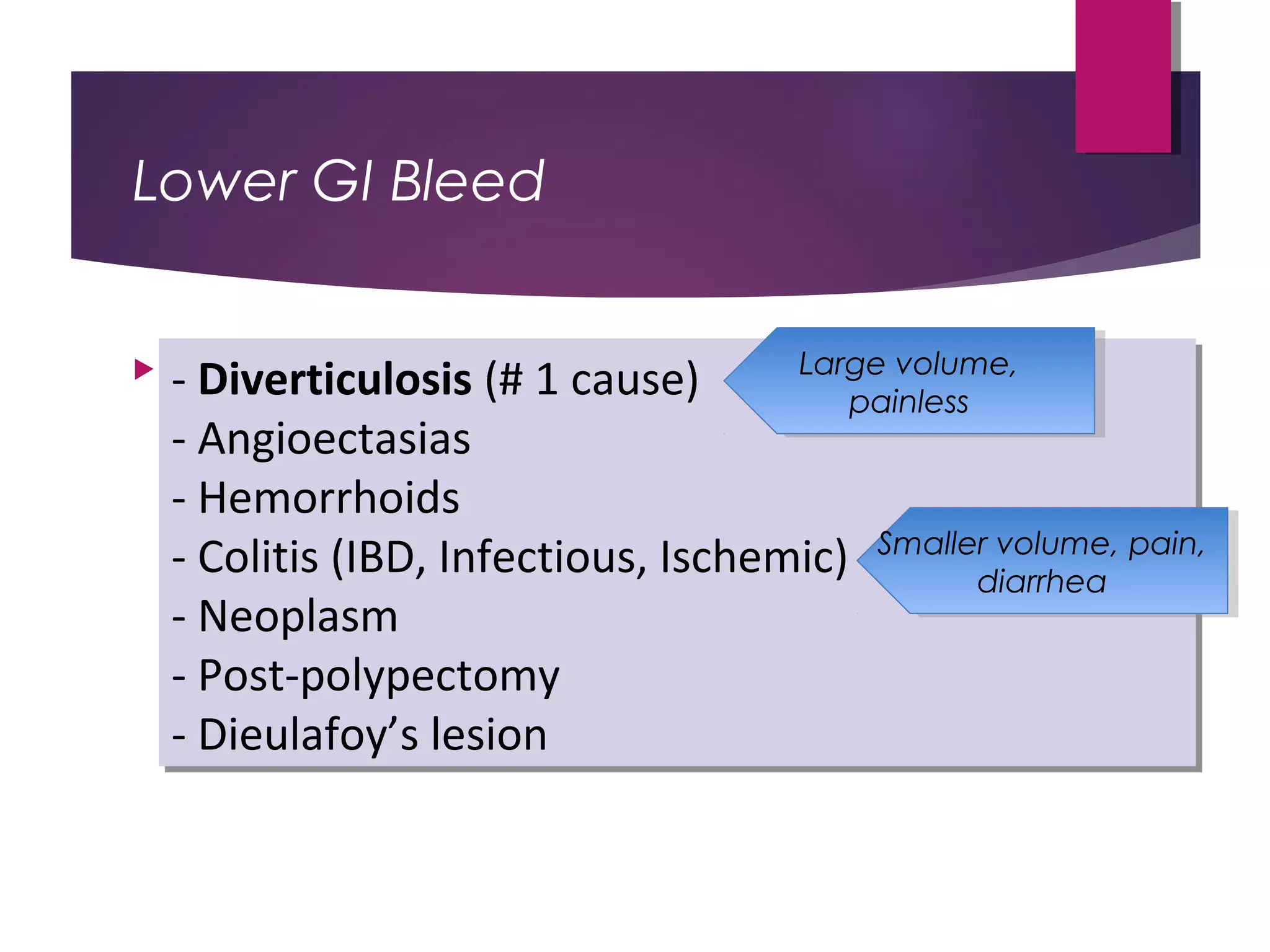
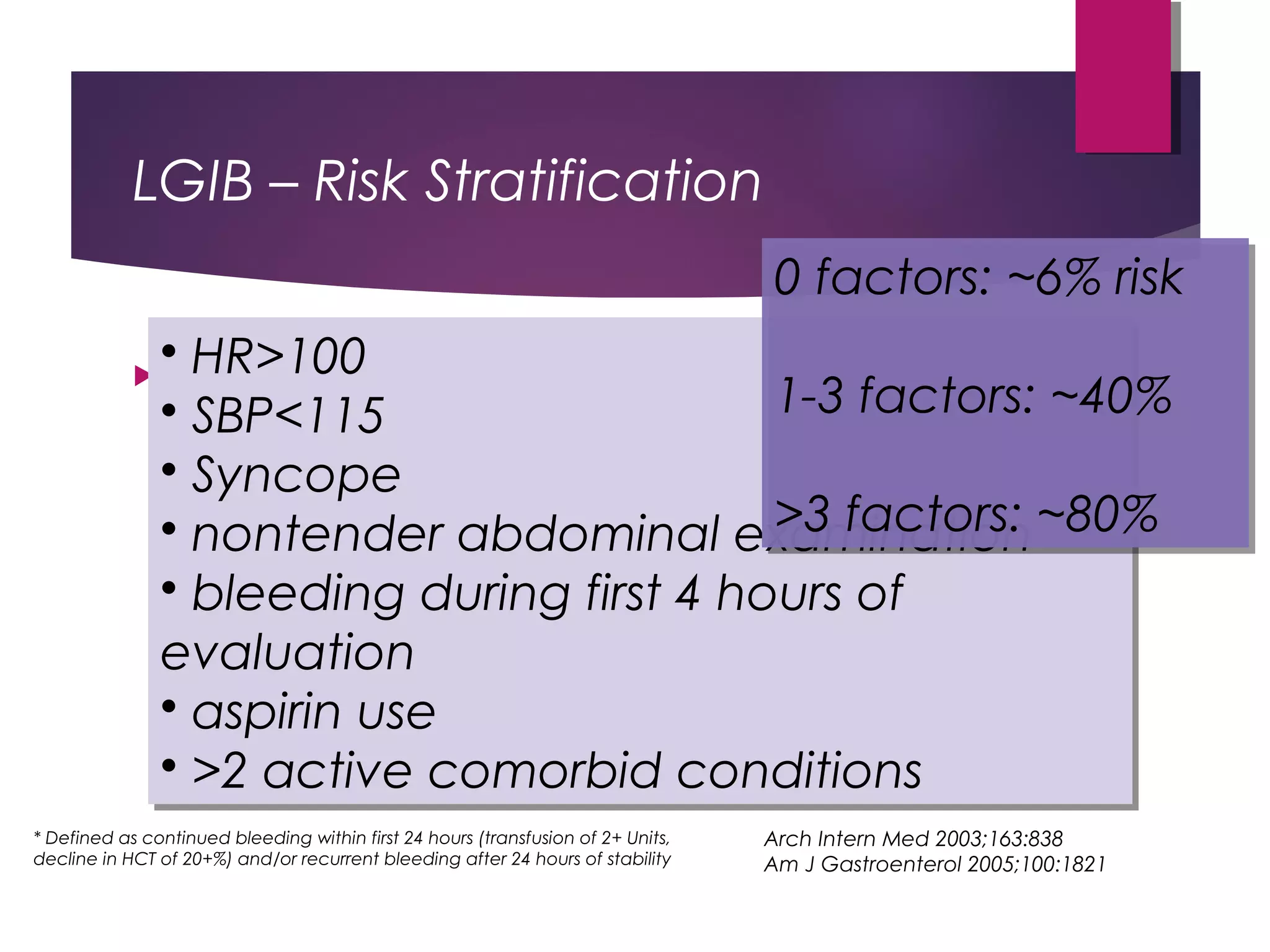
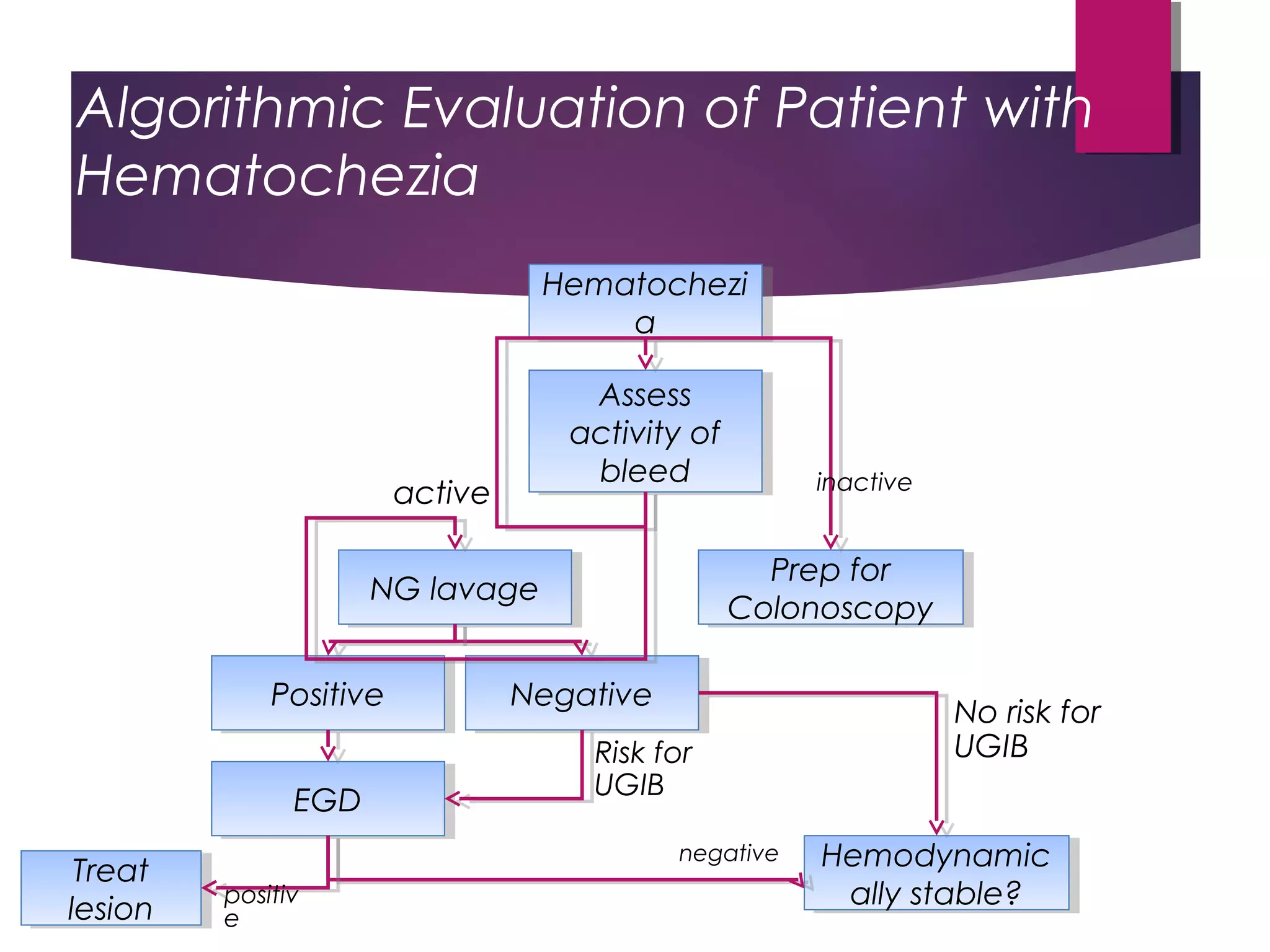
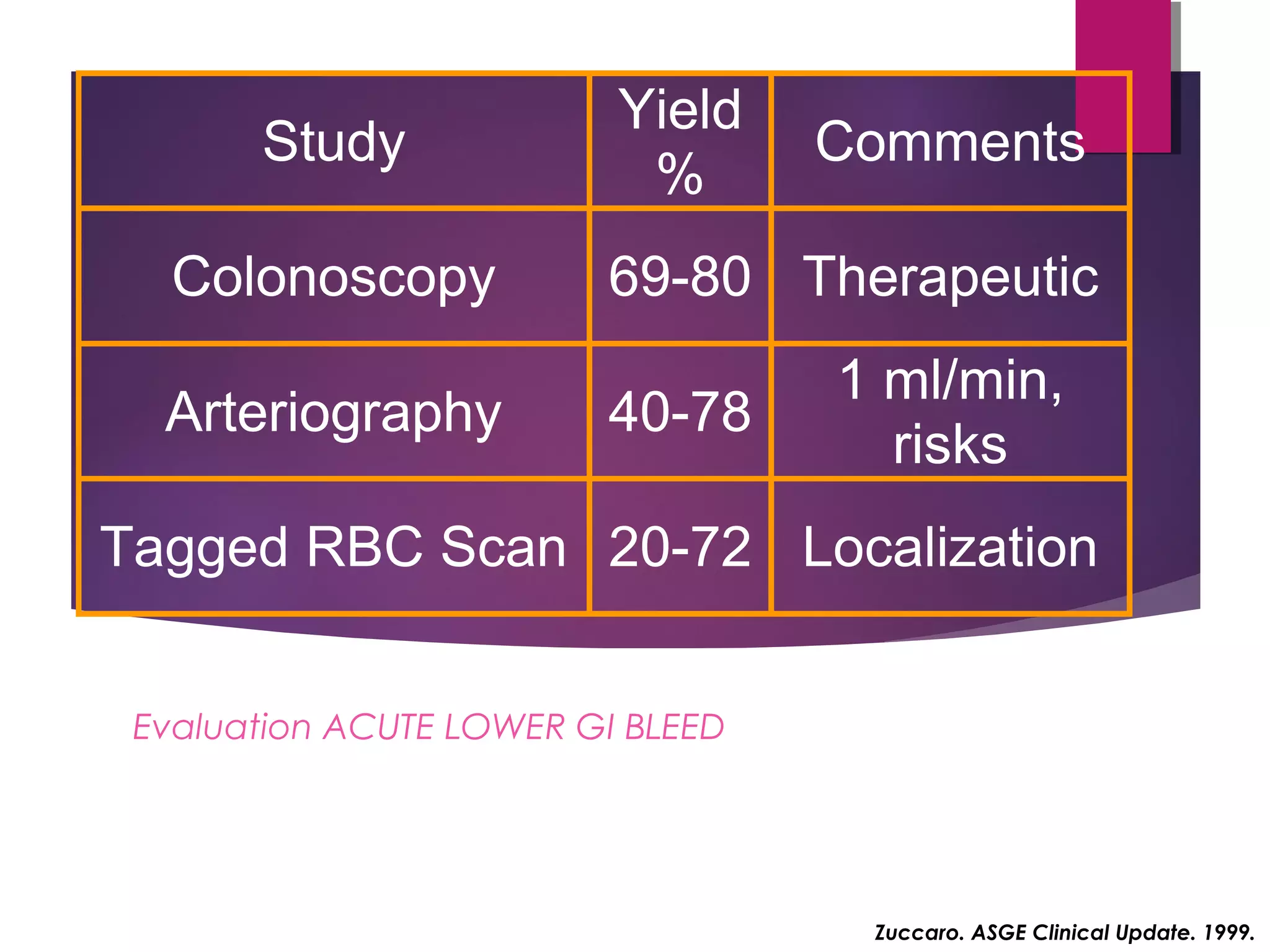
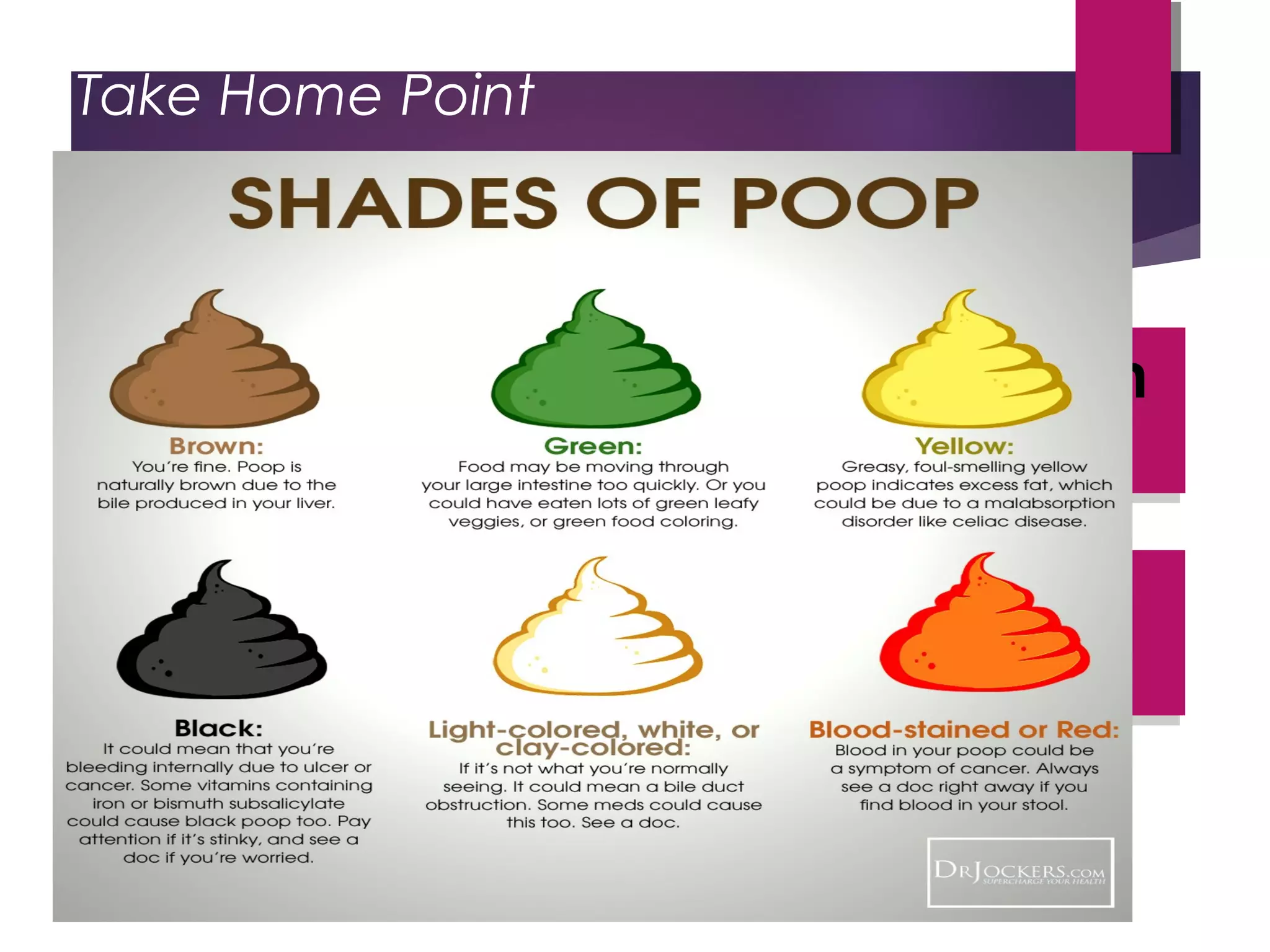
This document discusses the approach and management of acute lower gastrointestinal bleeding. It begins by defining upper, mid, and lower GI bleeding based on their origins. Stool color and characteristics can provide clues to the source and pace of bleeding. The case presented is of a 68-year-old male with a large amount of maroon colored bleeding from the rectum. His history, physical exam, and labs are discussed. The differential diagnosis and risk stratification for upper vs lower GI bleeding are reviewed. Initial resuscitation priorities like IV access, fluid resuscitation, blood transfusion thresholds and strategies, and coagulopathy correction are outlined. Risk factors, diagnostic modalities, and the role of colonoscopy versus surgery for lower GI