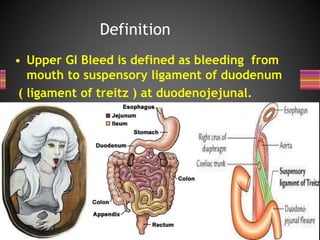
1. Gastrointestinal bleeding is a common presenting problem in the emergency room, with upper GI bleeding having an annual incidence of approximately 47 per 100,000 people.
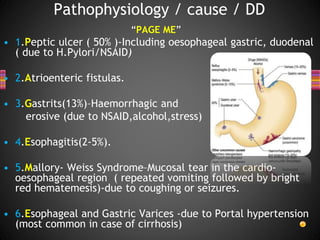
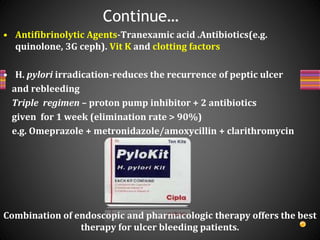
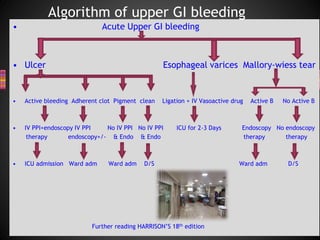
2. The main causes of upper GI bleeding include peptic ulcers, esophageal varices, gastritis, and esophagitis.
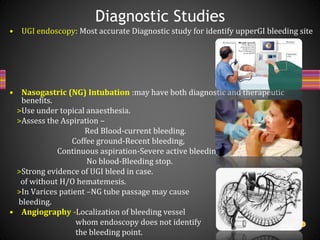
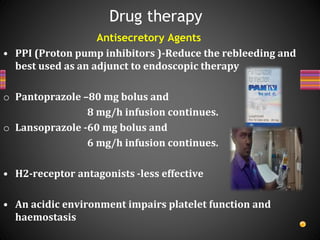
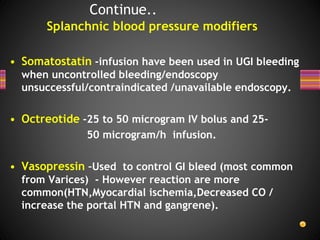
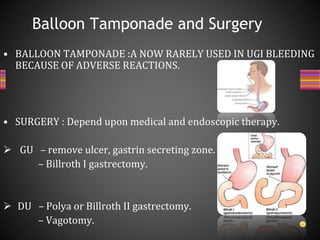
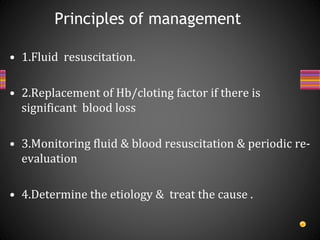
3. The initial priorities in management are resuscitation through fluid resuscitation and blood transfusion if needed, followed by endoscopy to determine the source of bleeding and provide endoscopic therapy if active bleeding is detected.