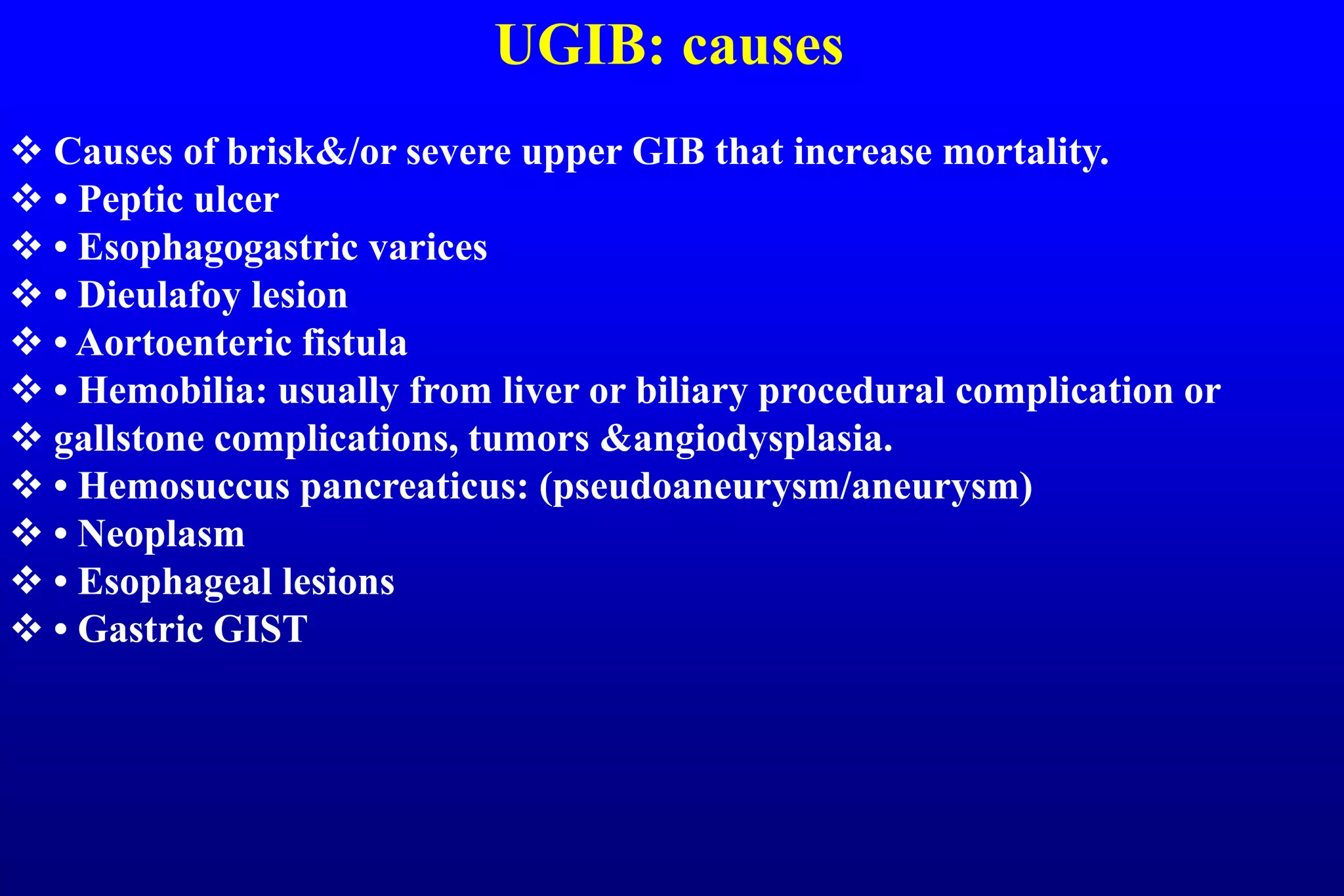
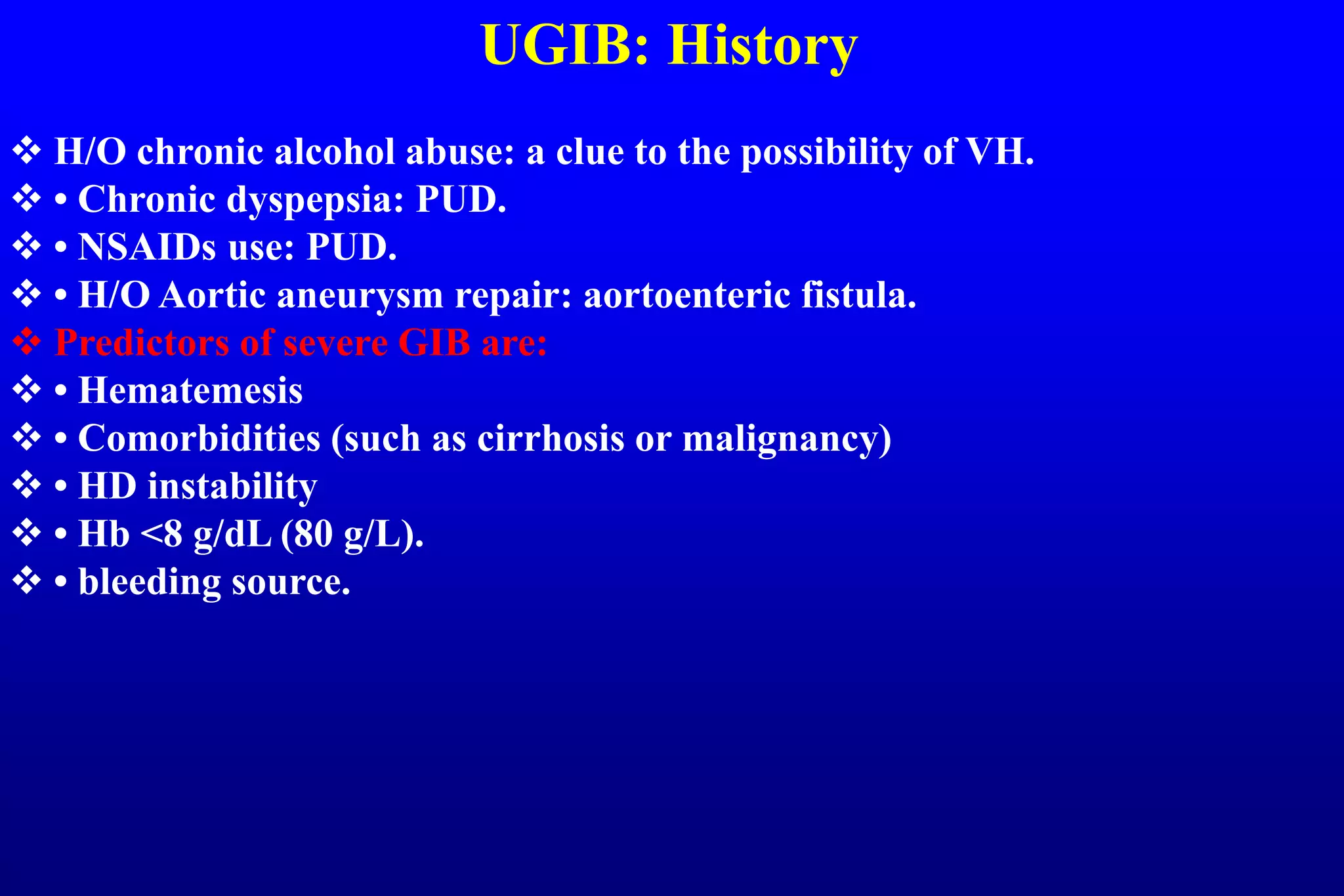
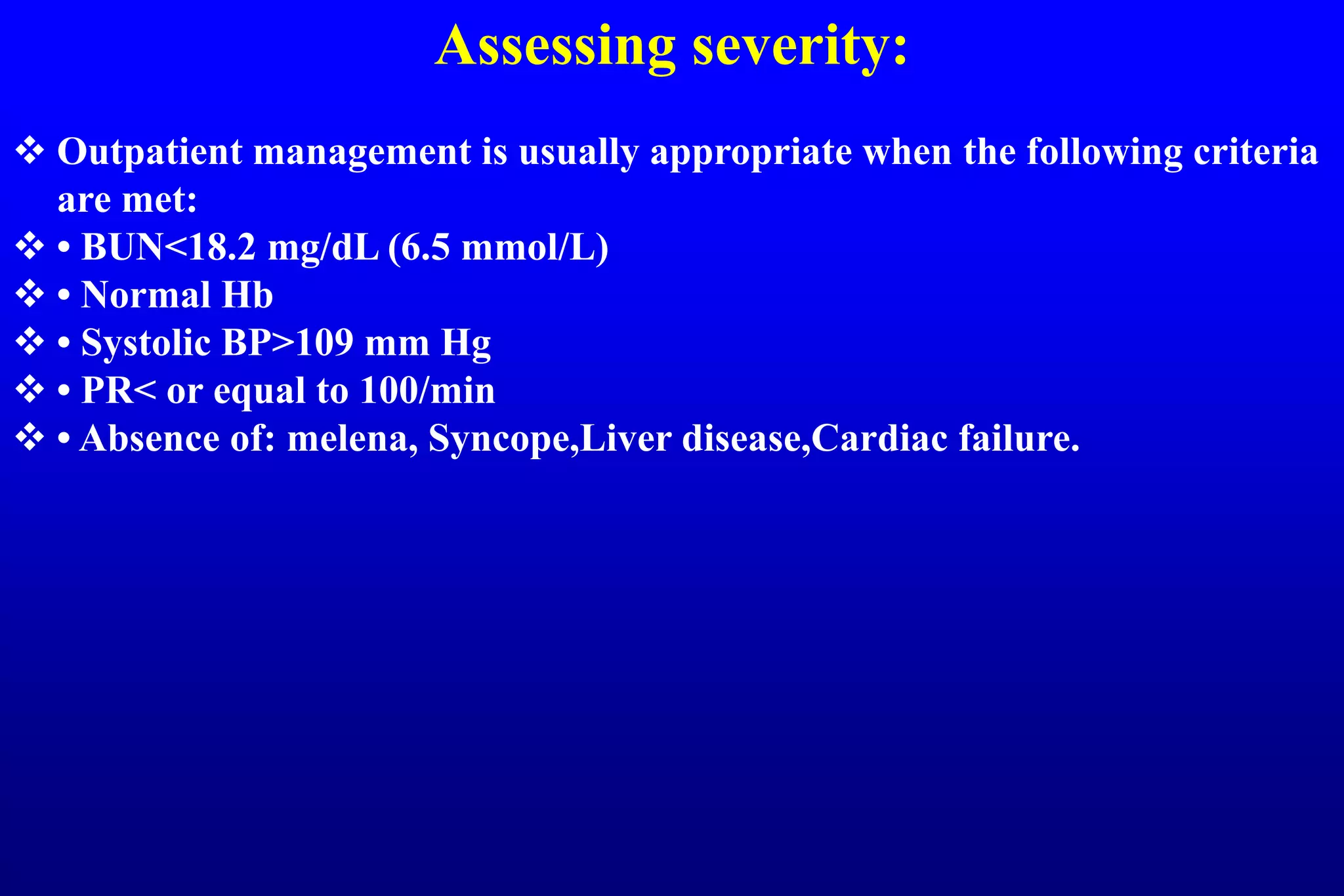
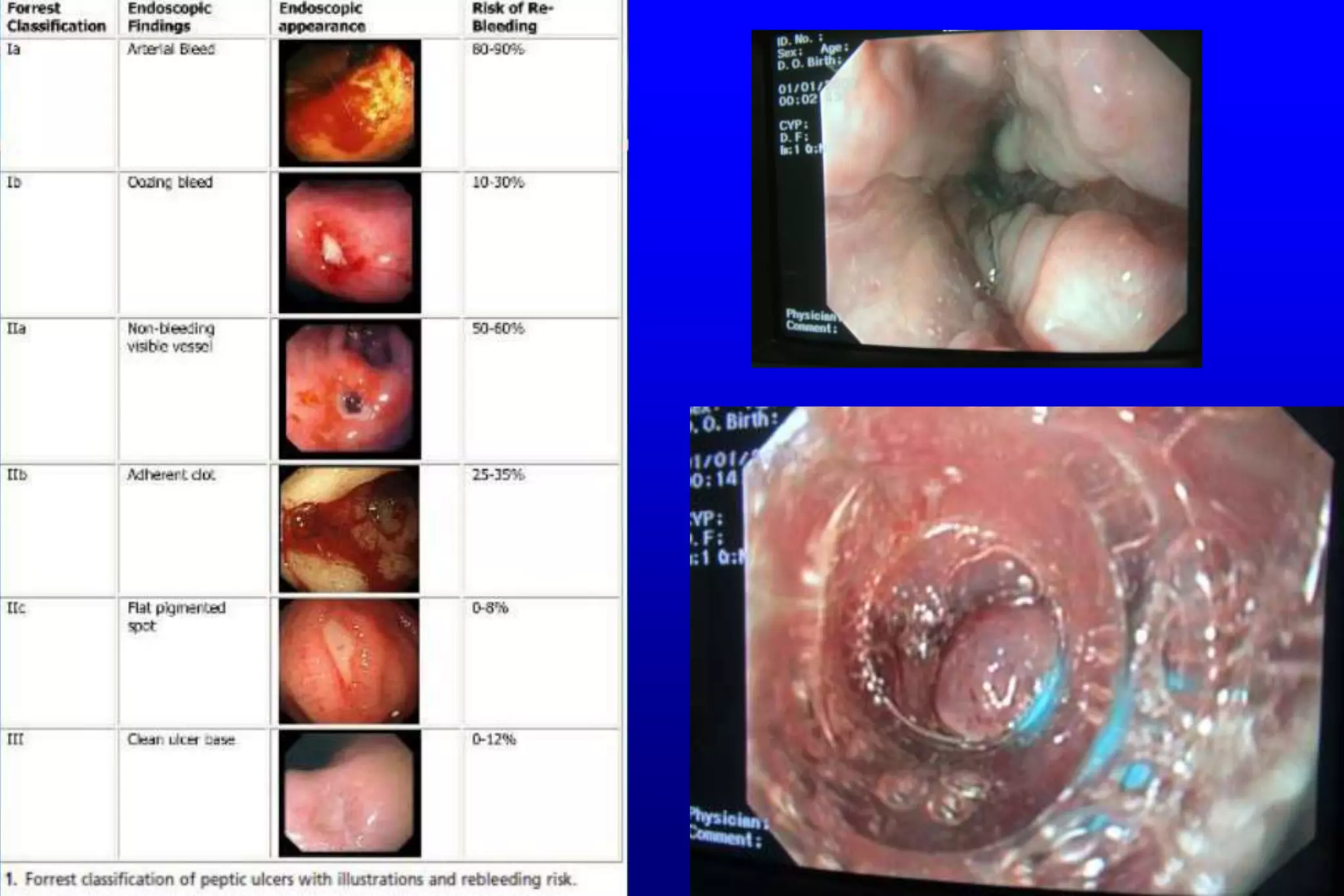
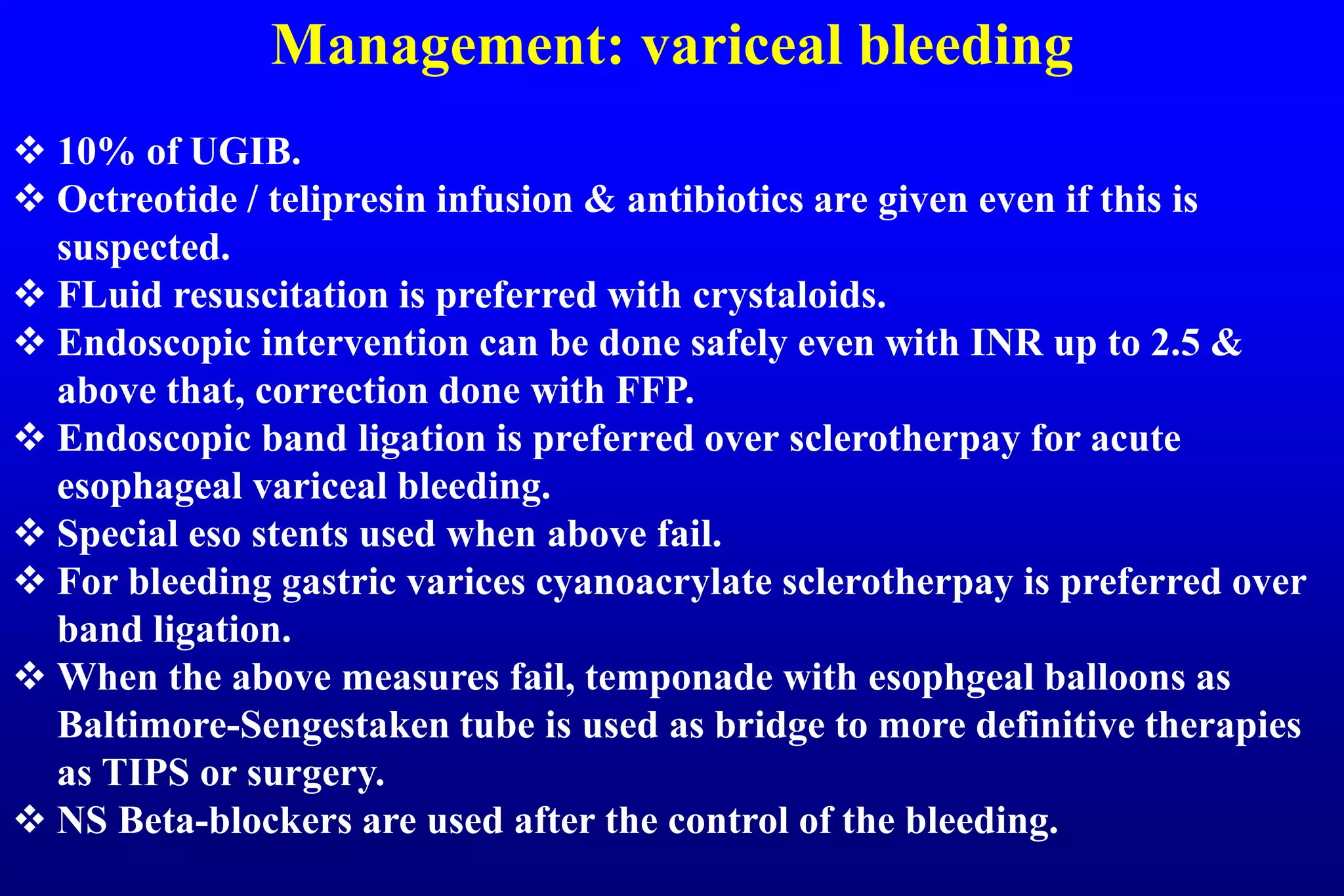
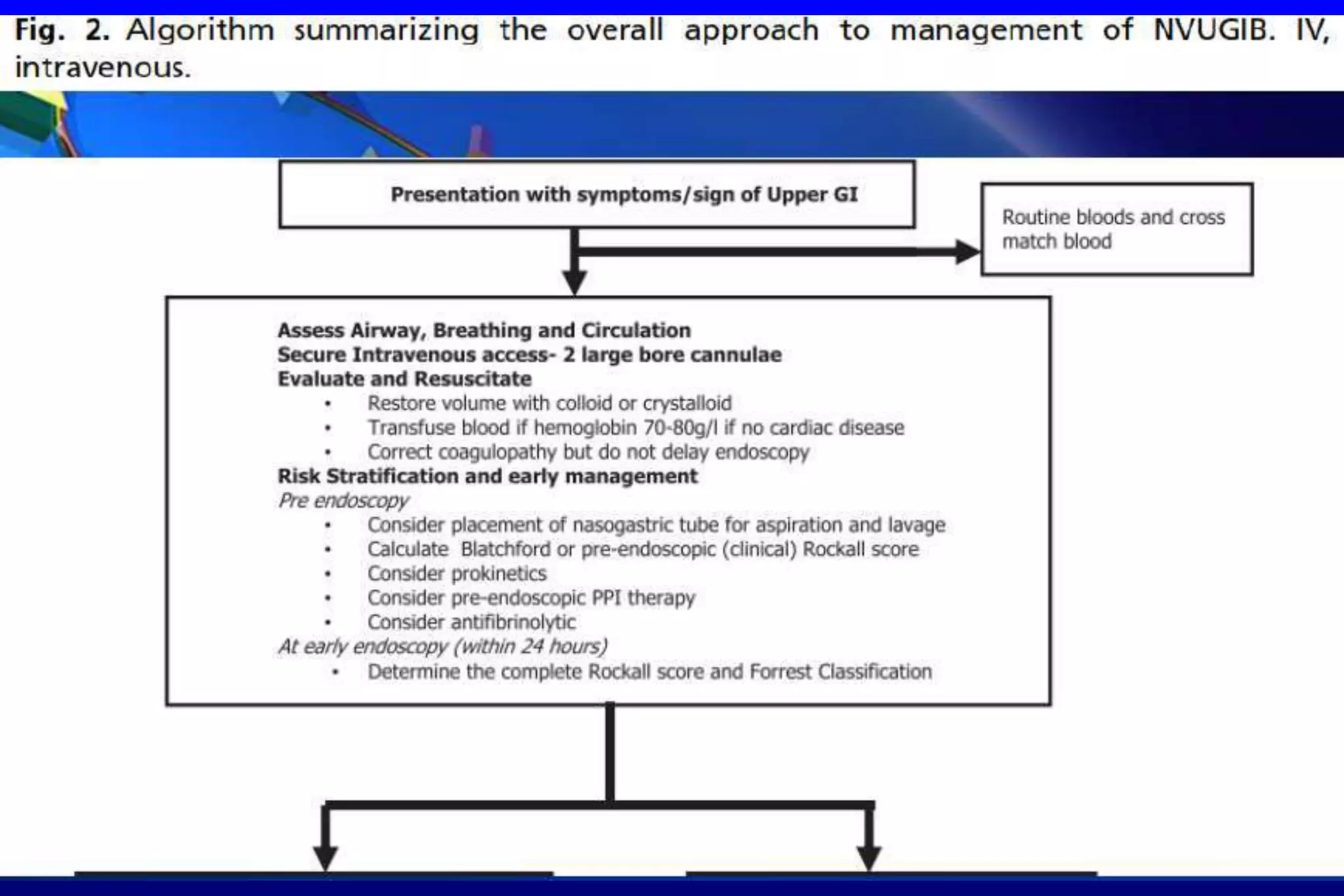
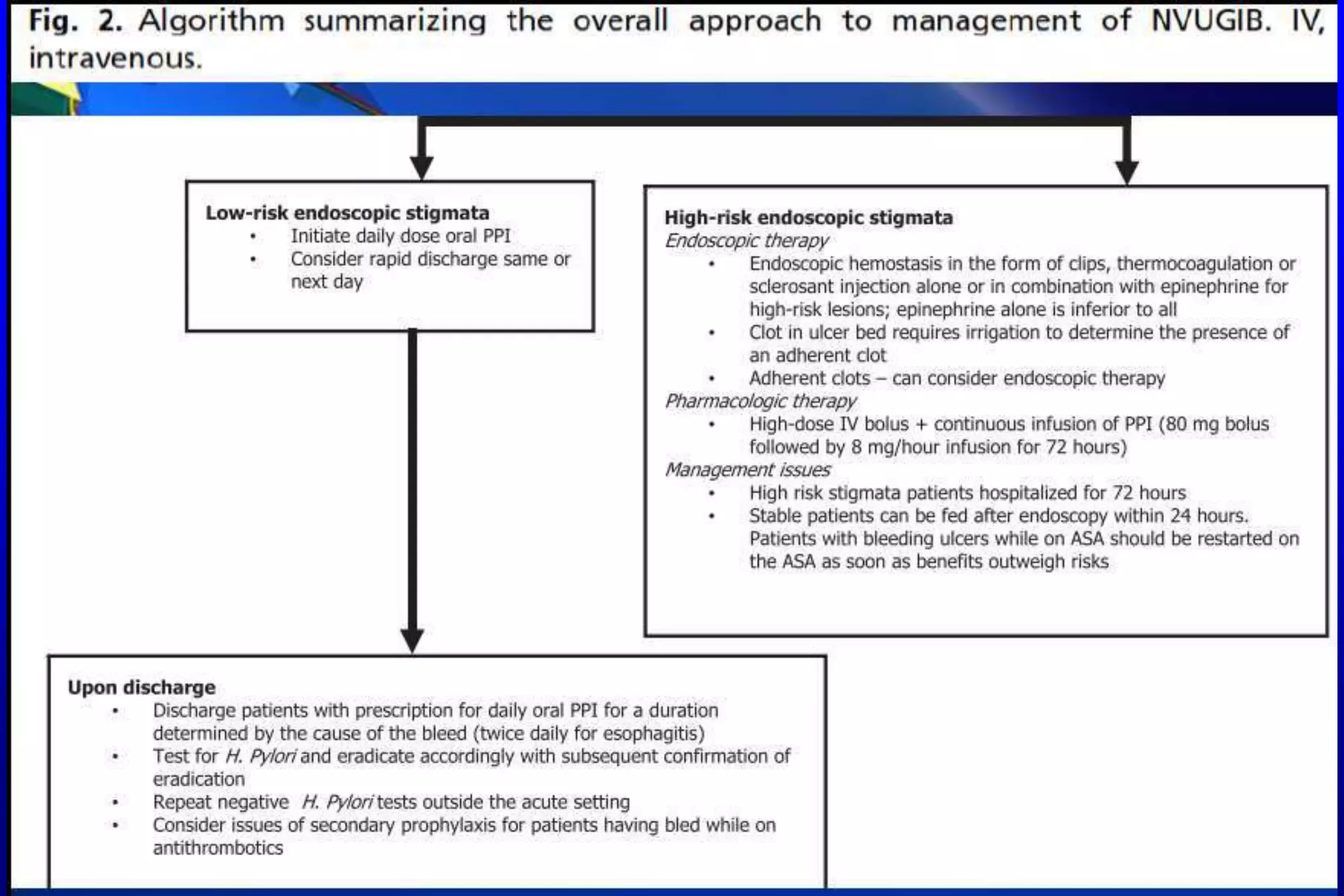
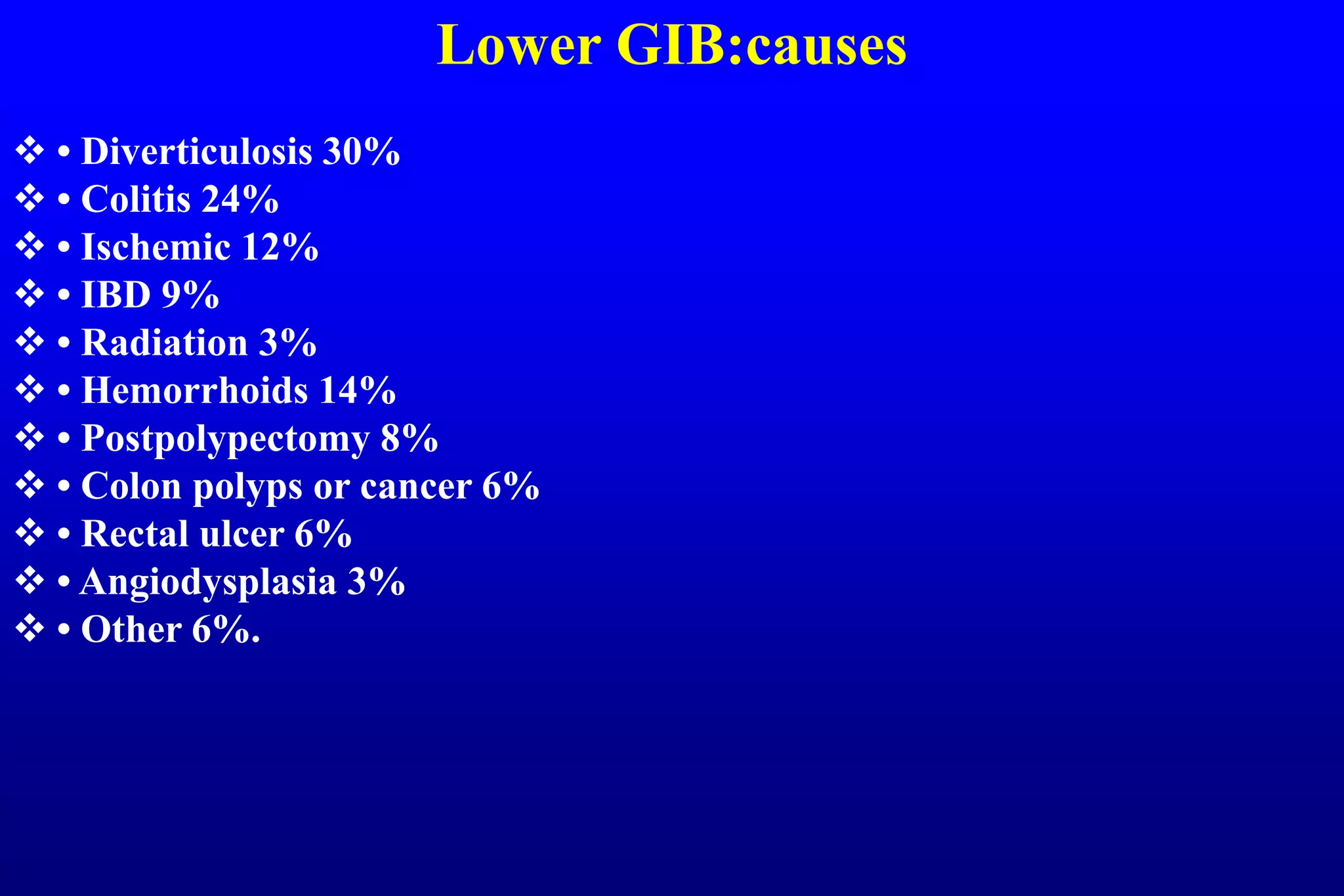
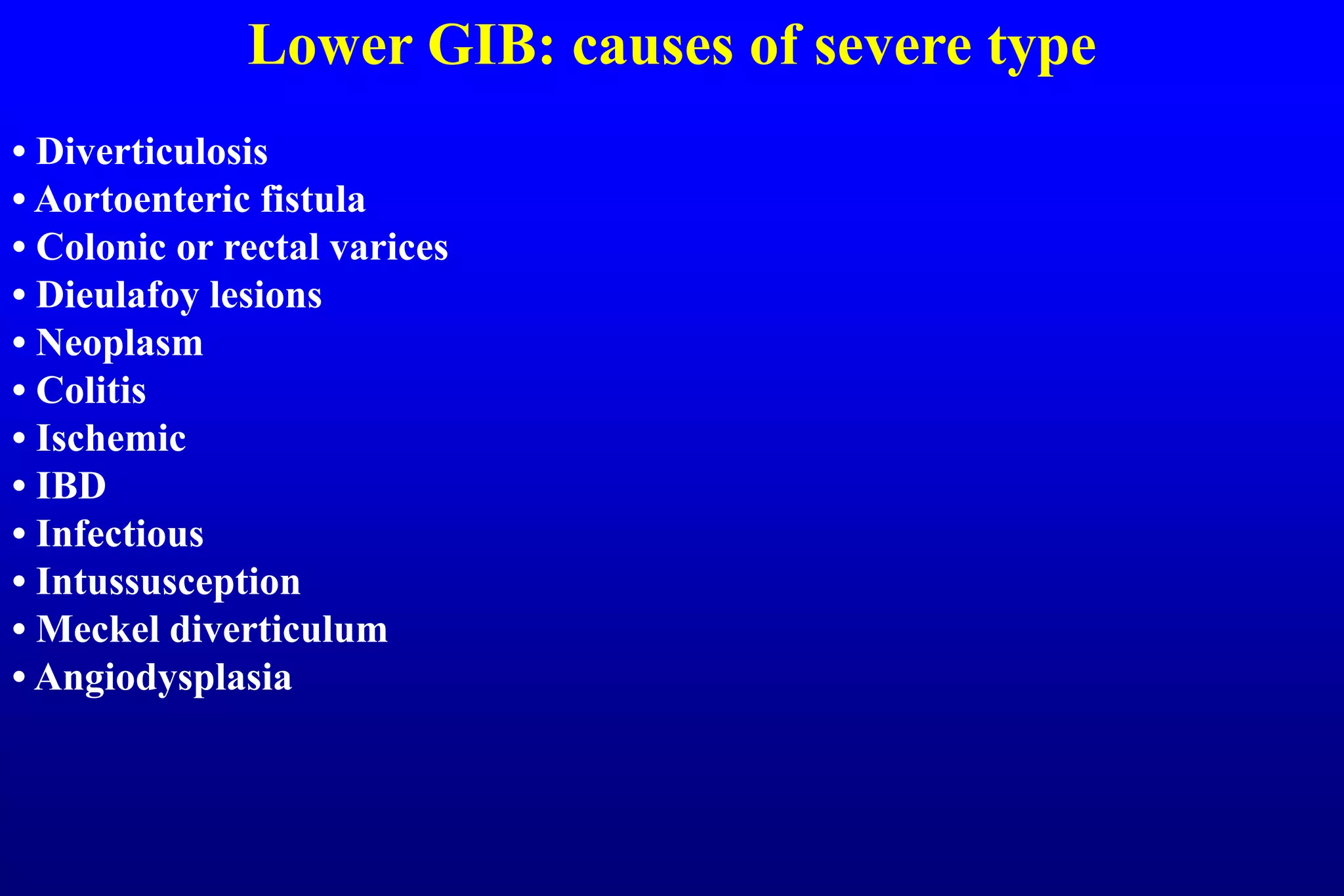
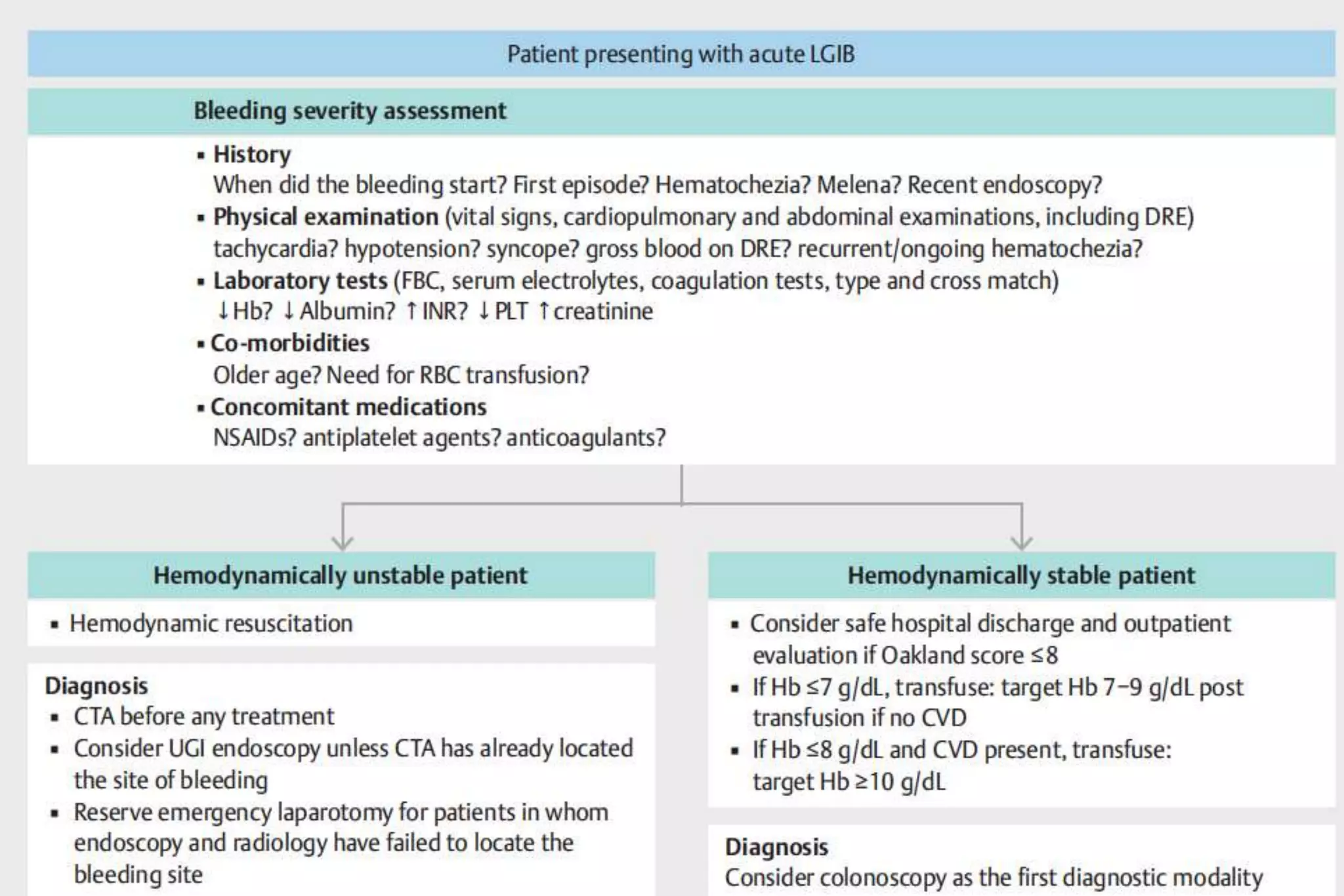
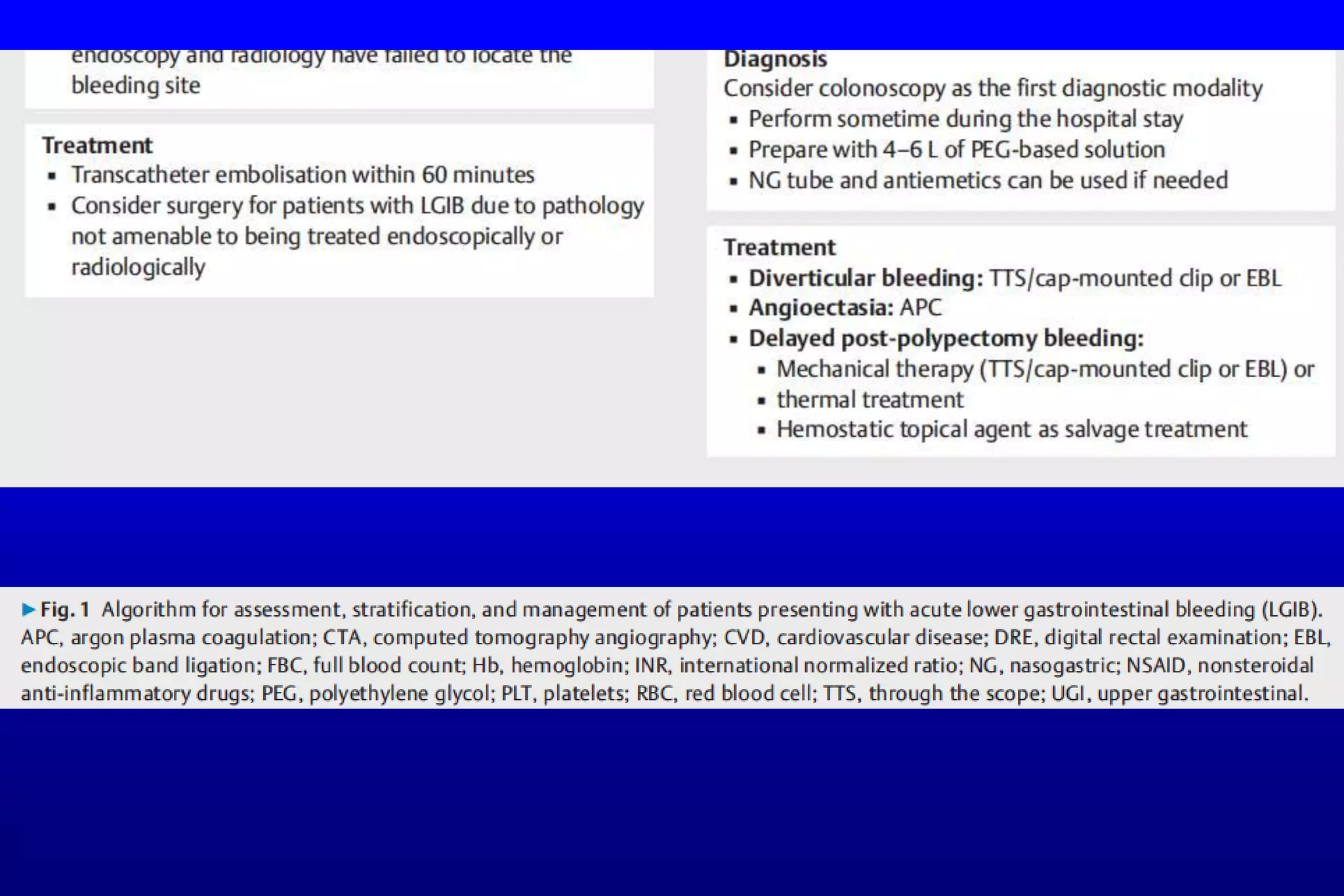
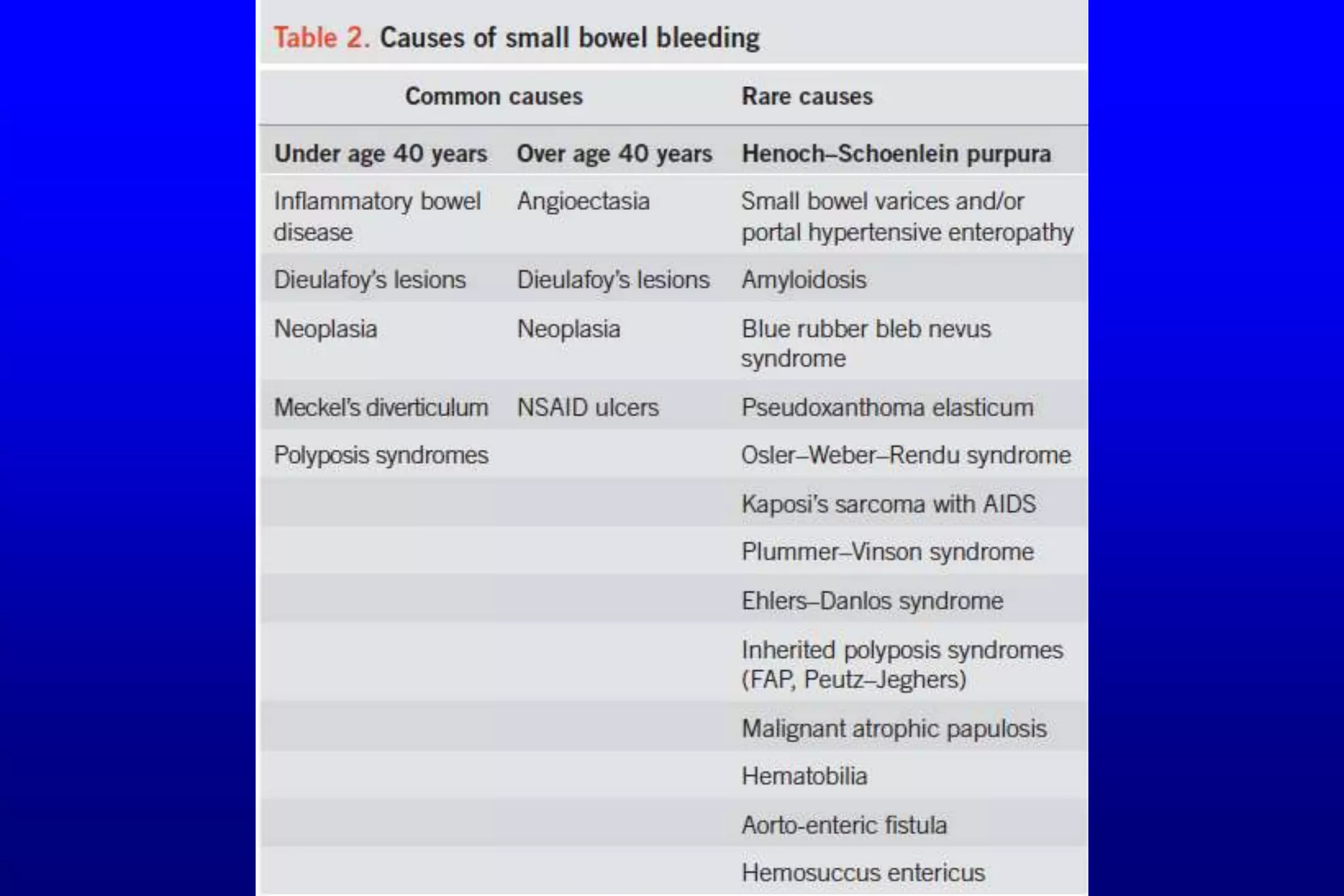
This document discusses gastrointestinal bleeding (GIB), summarizing its main causes and approaches to management. It notes that upper GIB accounts for 80% of cases, with the most common causes being peptic ulcer disease, esophageal varices, esophagitis, and Mallory-Weiss tears. Lower GIB is more common in the elderly and can be caused by conditions like diverticulosis, colitis, ischemia, and hemorrhoids. Small intestinal bleeding is relatively uncommon but can now be identified in most patients using video capsule endoscopy, deep enteroscopy, or radiological imaging. The document provides guidance on assessing severity, differentiating upper from lower sources, initial resuscitation measures, the role of endoscopy,