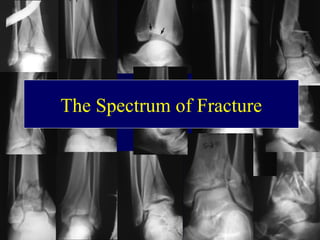
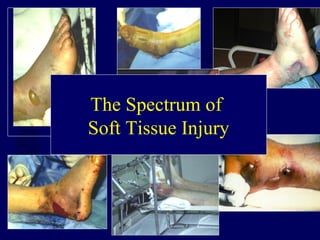
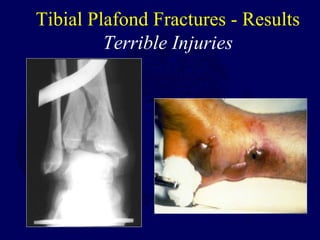
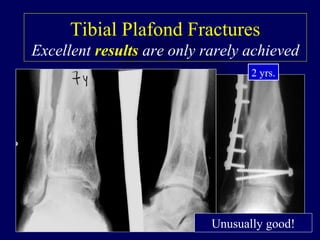
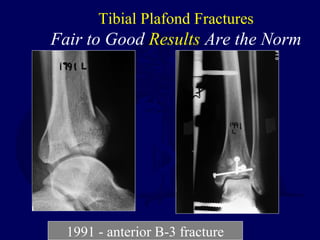
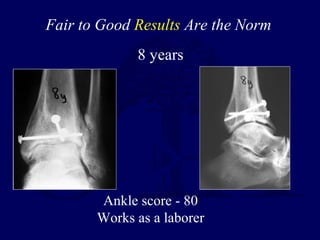
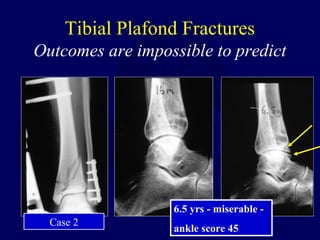
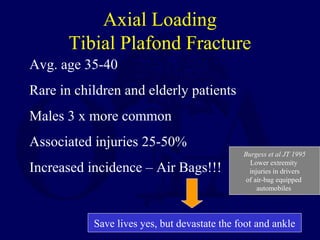
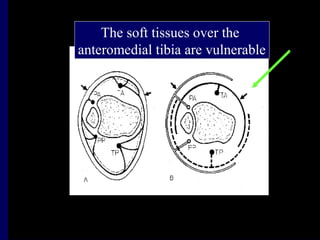
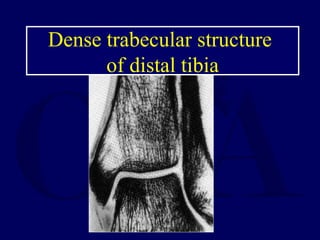
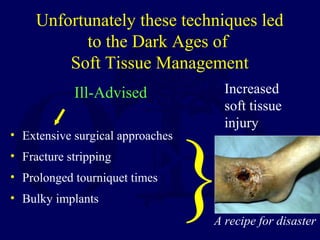
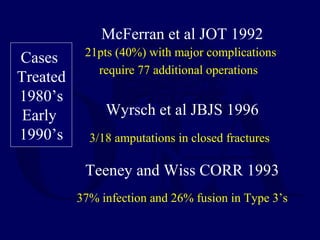
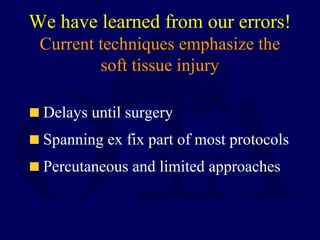
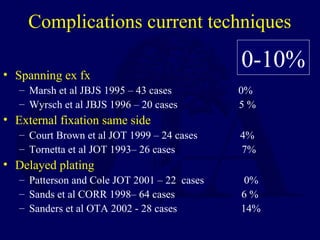
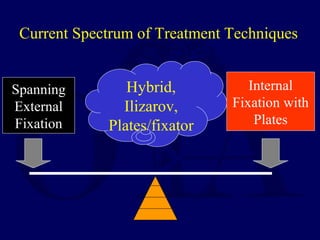
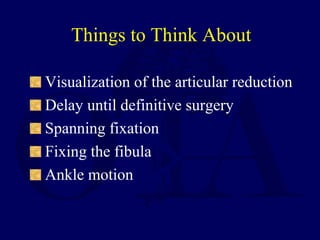
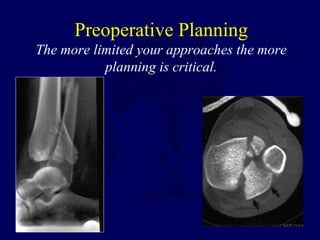
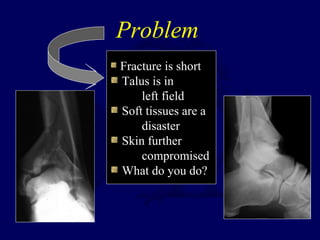
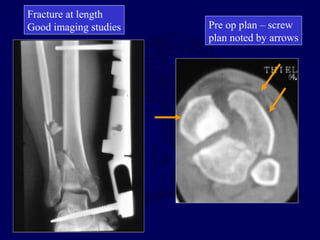
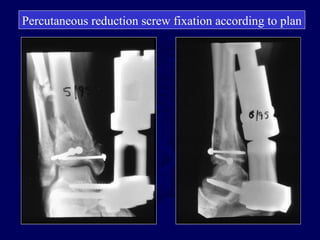
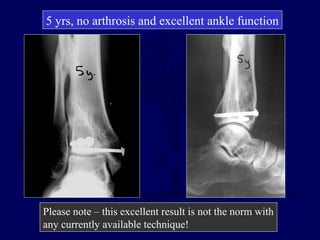
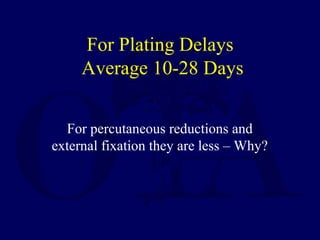
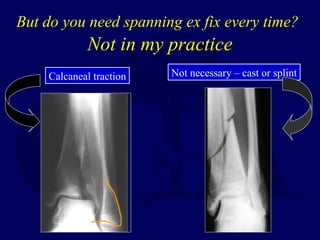
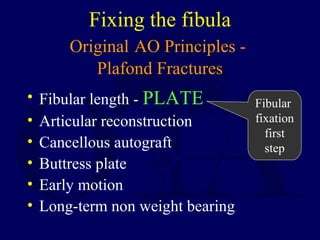
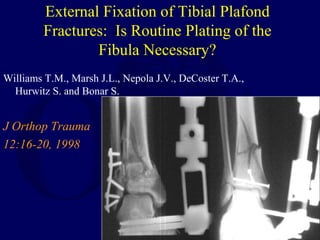
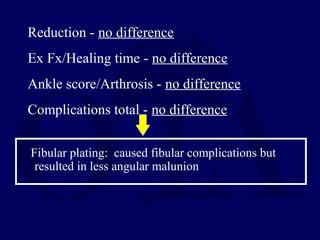
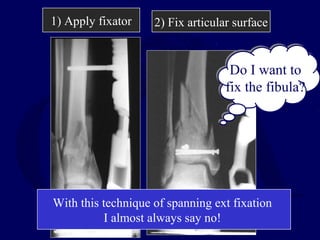
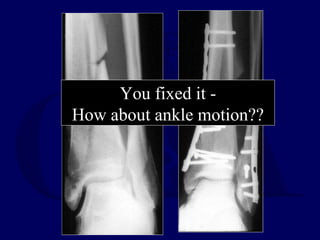
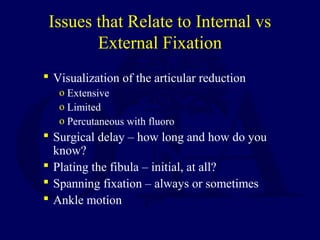
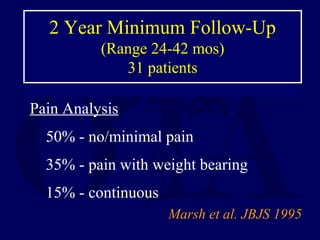
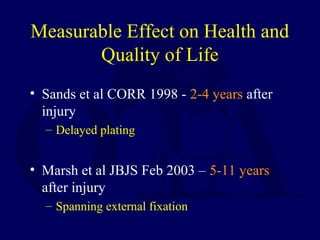
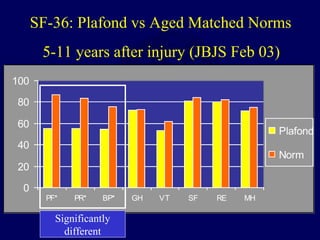
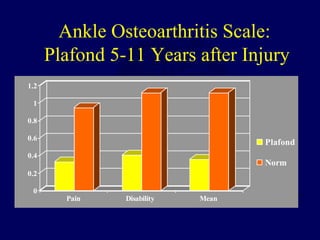
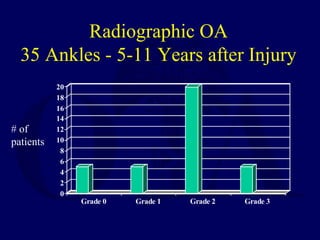
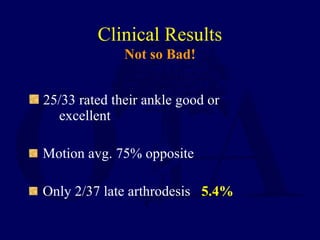
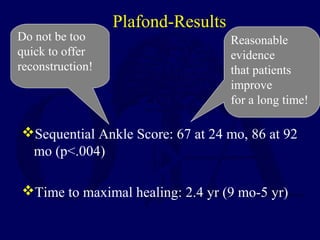
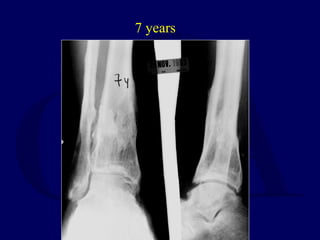
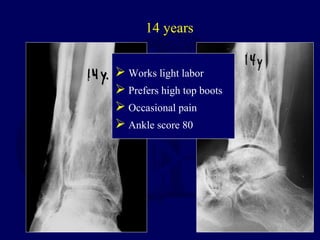
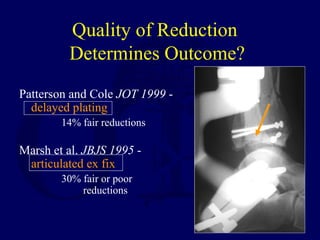
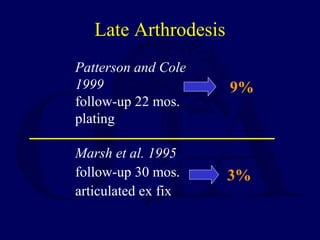
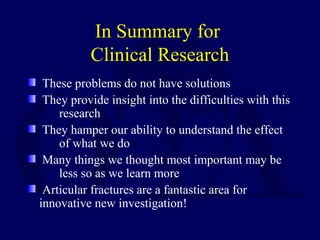
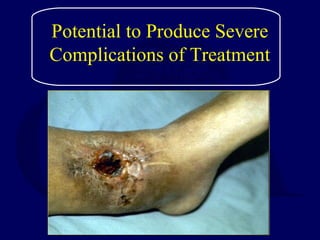
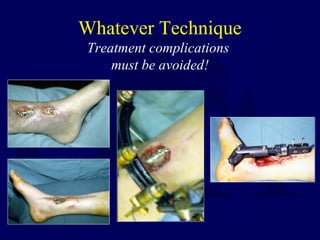
Tibial plafond fractures are severe injuries that often result in fair to good outcomes rather than excellent outcomes. Soft tissue management is crucial, and treatment concepts have shifted from extensive surgical approaches to emphasize soft tissue recovery through techniques like spanning external fixation and delayed surgery. While long-term follow up shows many patients experience pain and arthrosis, most rate their ankle as good or excellent, demonstrating the ability to improve over many years. Excellent results remain difficult to achieve for these injuries.