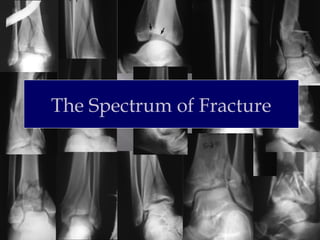
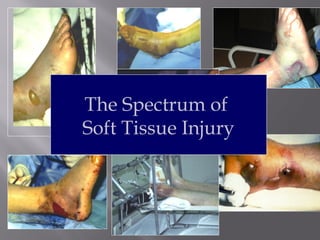
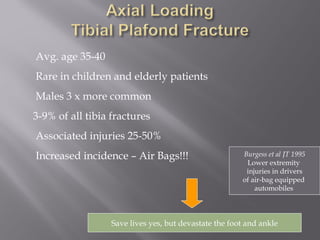
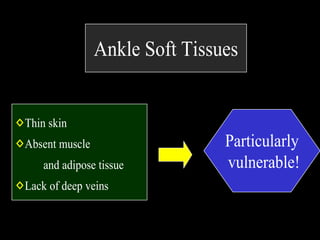
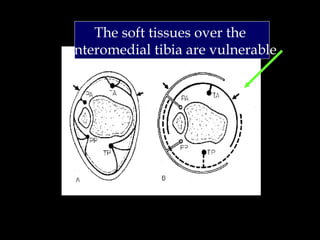
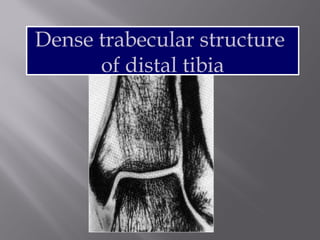
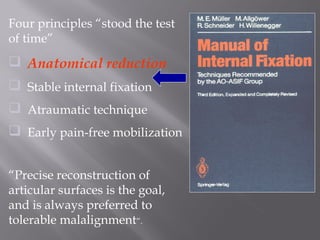
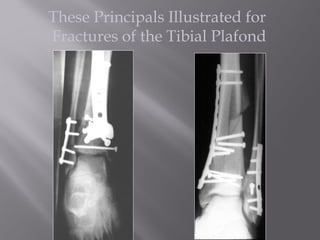
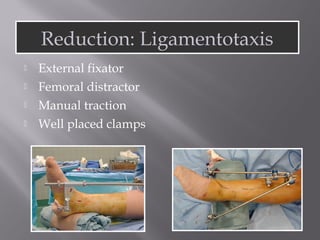
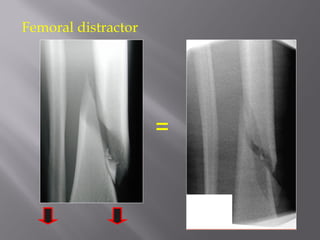
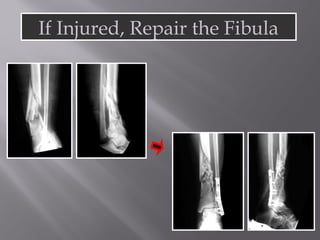
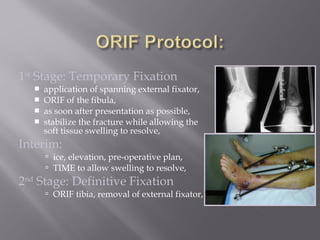
1) Tibial plafond fractures involve injuries to both the bone and soft tissues of the distal tibia. They require anatomical reduction, stable fixation, and early mobilization to achieve the best outcomes.
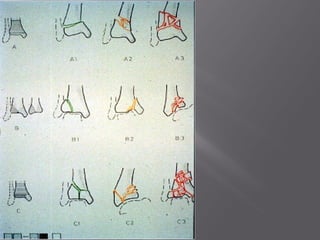
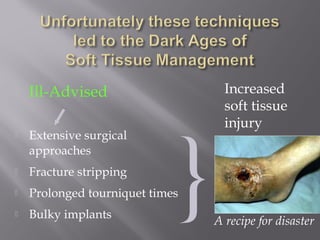
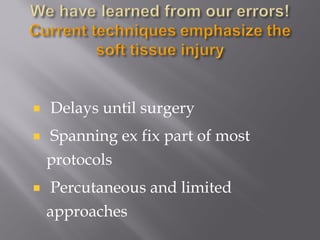
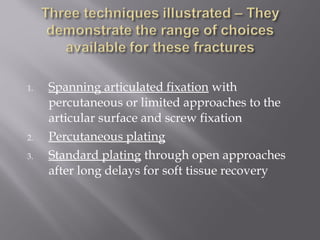
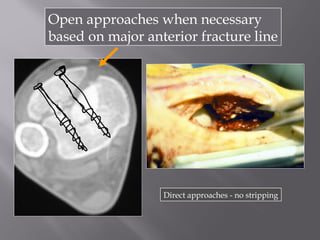
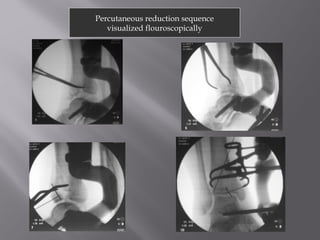
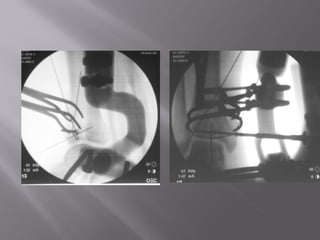
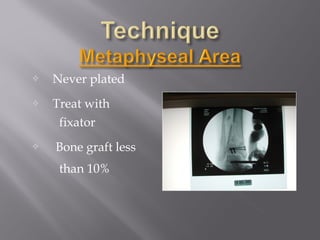
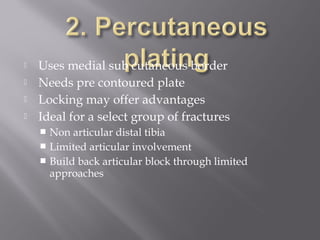
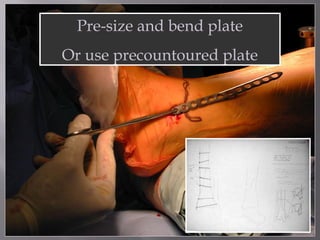
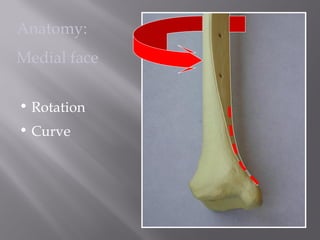
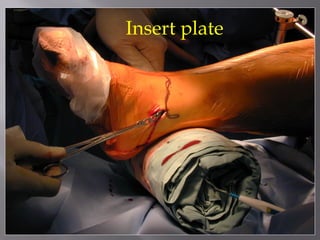
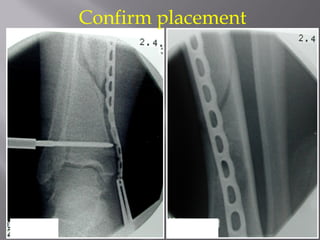
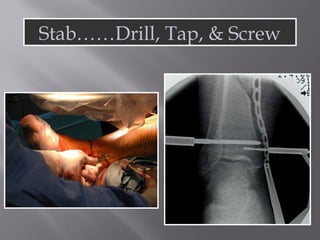
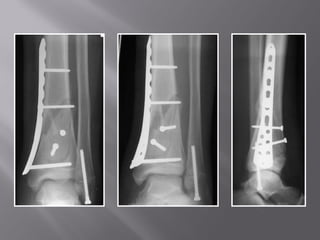
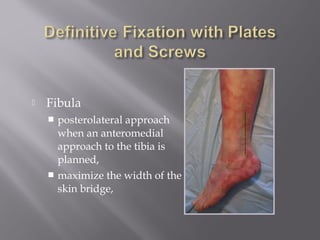
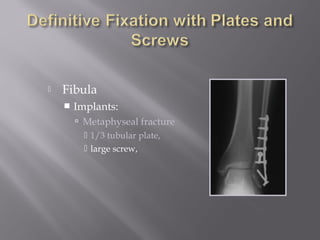
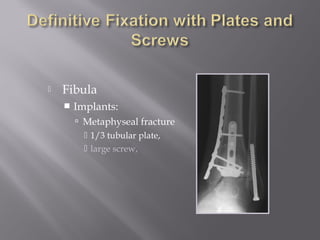
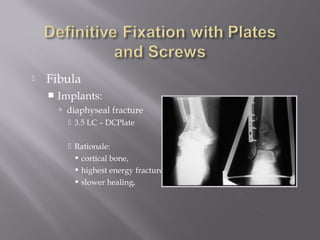
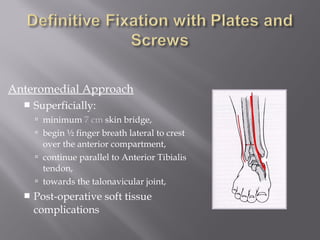
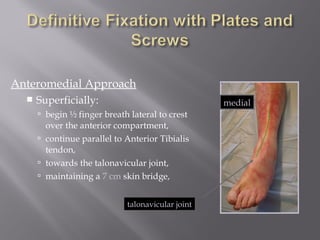
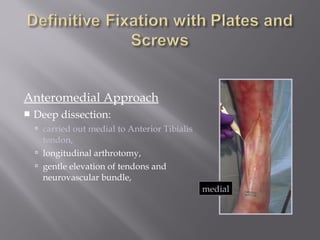
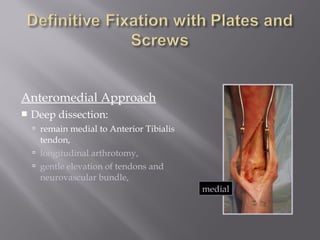
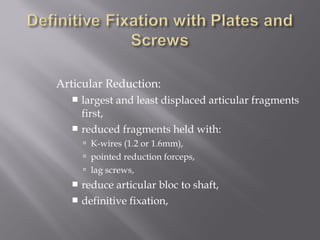
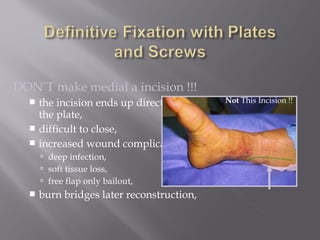
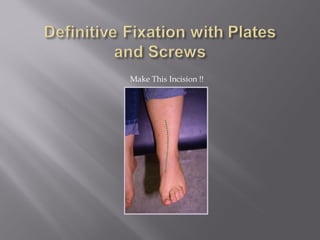
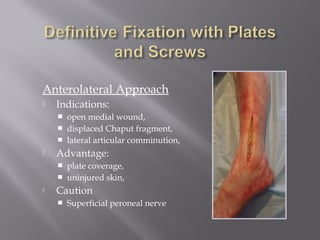
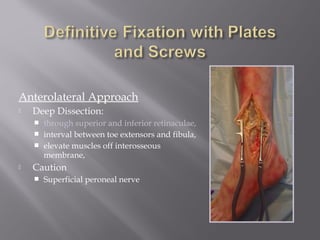
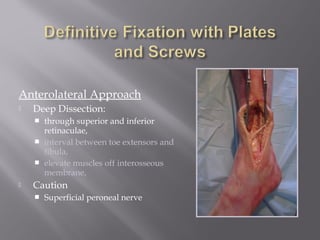
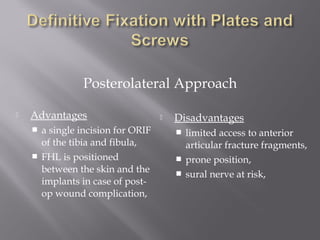
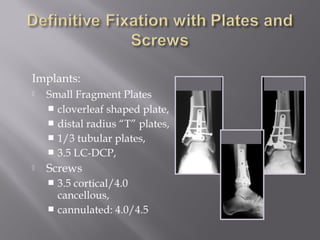
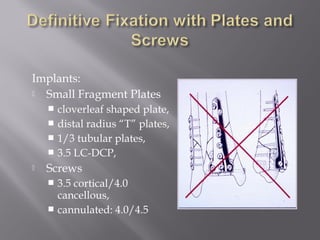
2) Several surgical approaches can be used including anteromedial, anterolateral, and posterolateral. Small fragment plates and screws are typically used for internal fixation. Meticulous soft tissue management and wound closure are important.
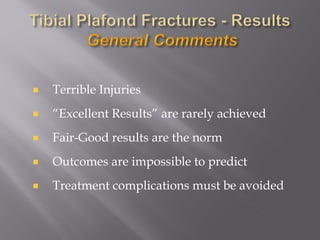
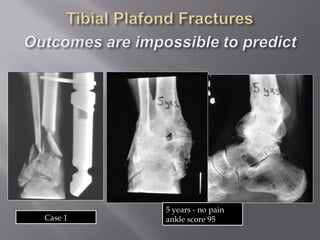
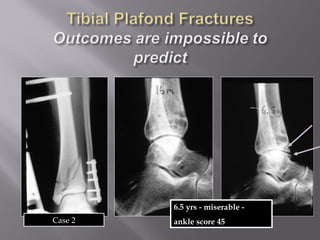
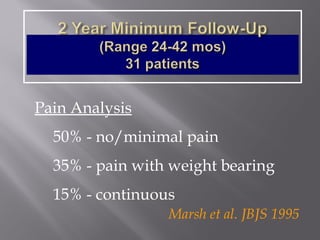
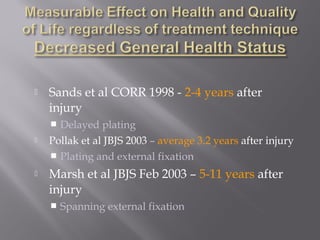
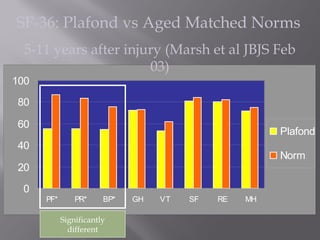
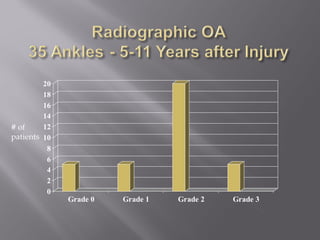
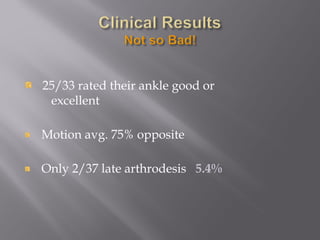
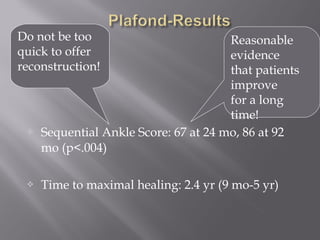
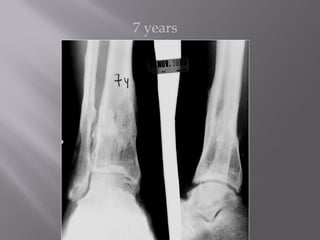
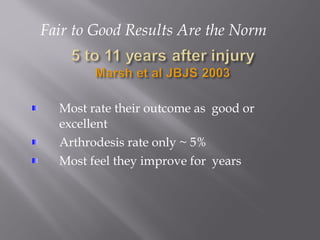
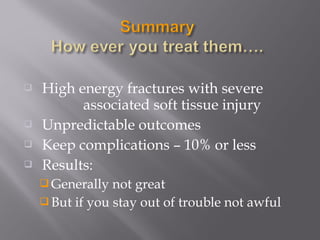
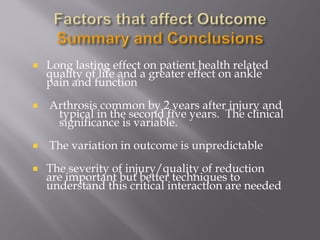
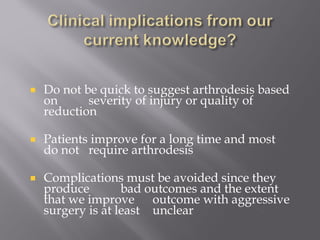
3) While most patients experience some pain, many are able to return to work. Arthrosis is detected in about 50% of cases, but arthrodesis is rare. Outcomes improve over time, and patients should not be rushed into reconstruction without allowing for further