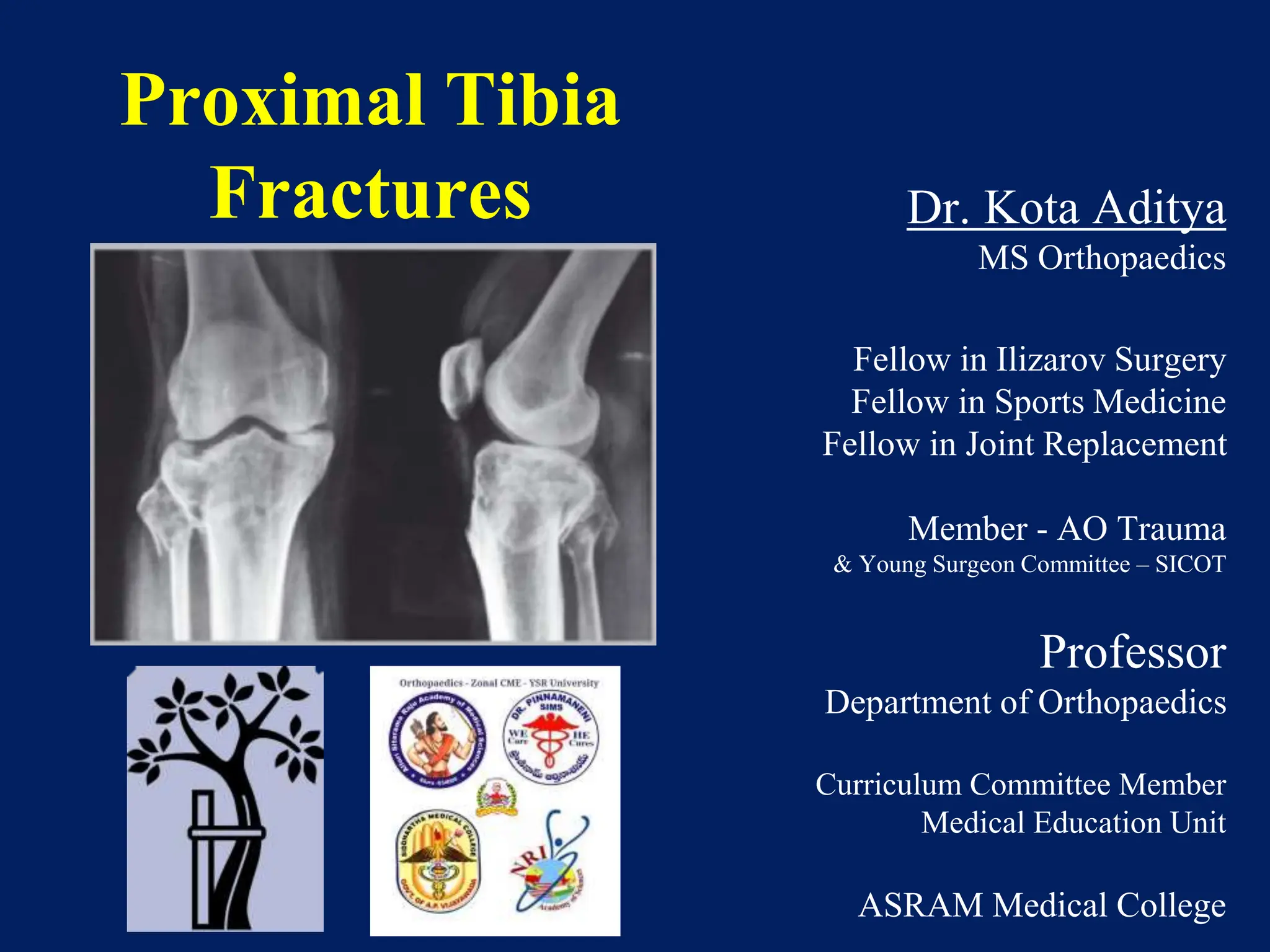
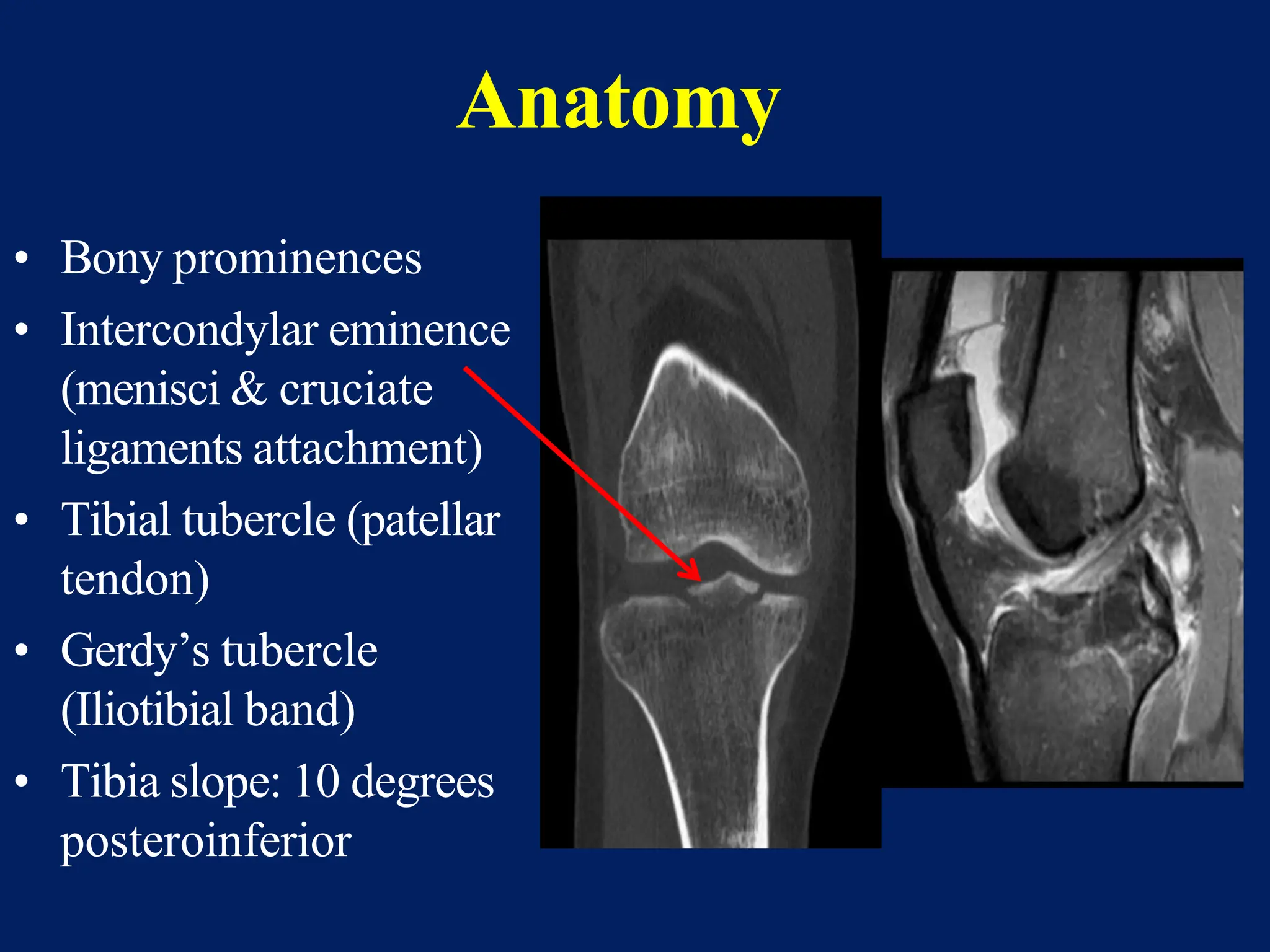
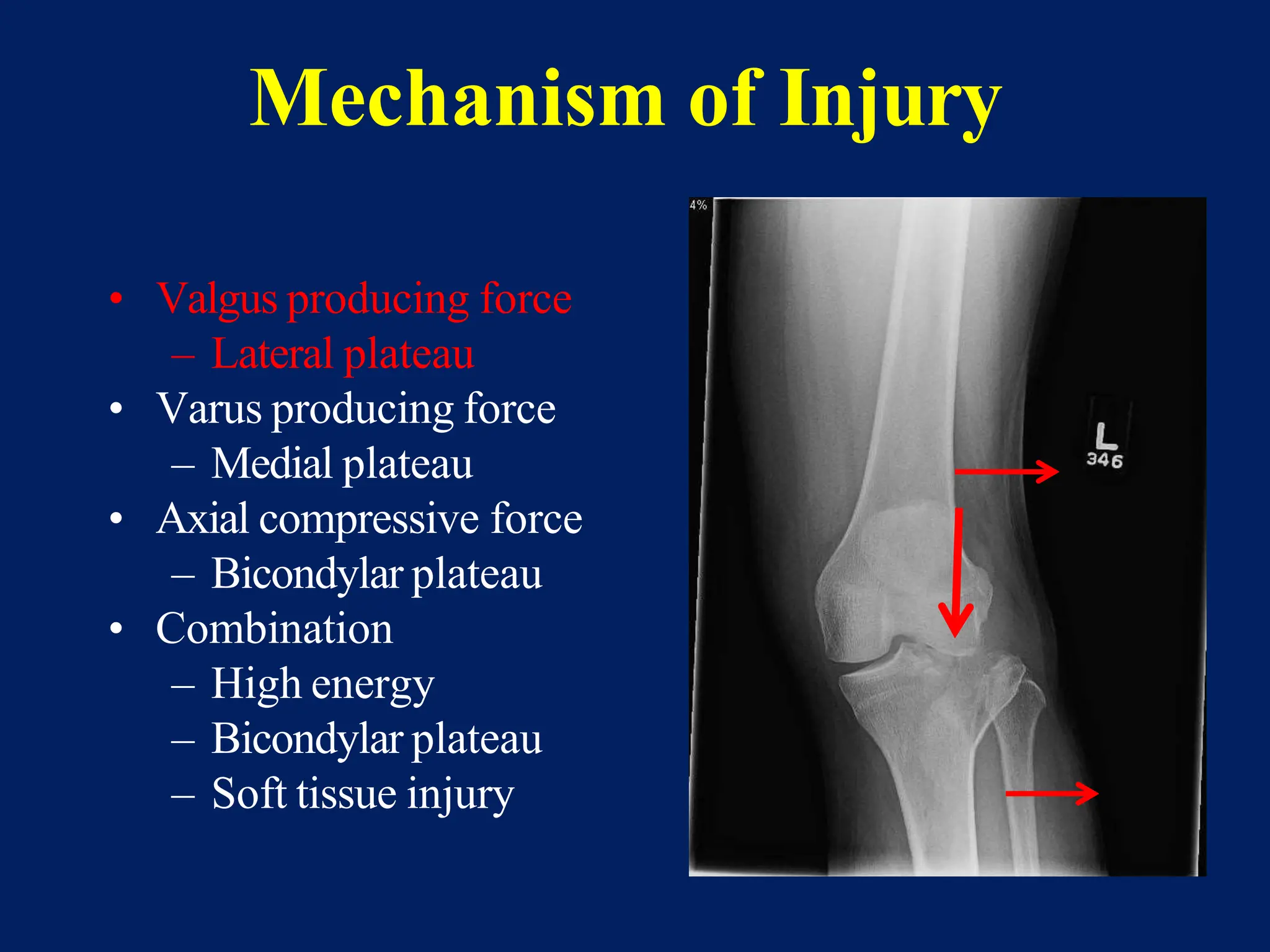
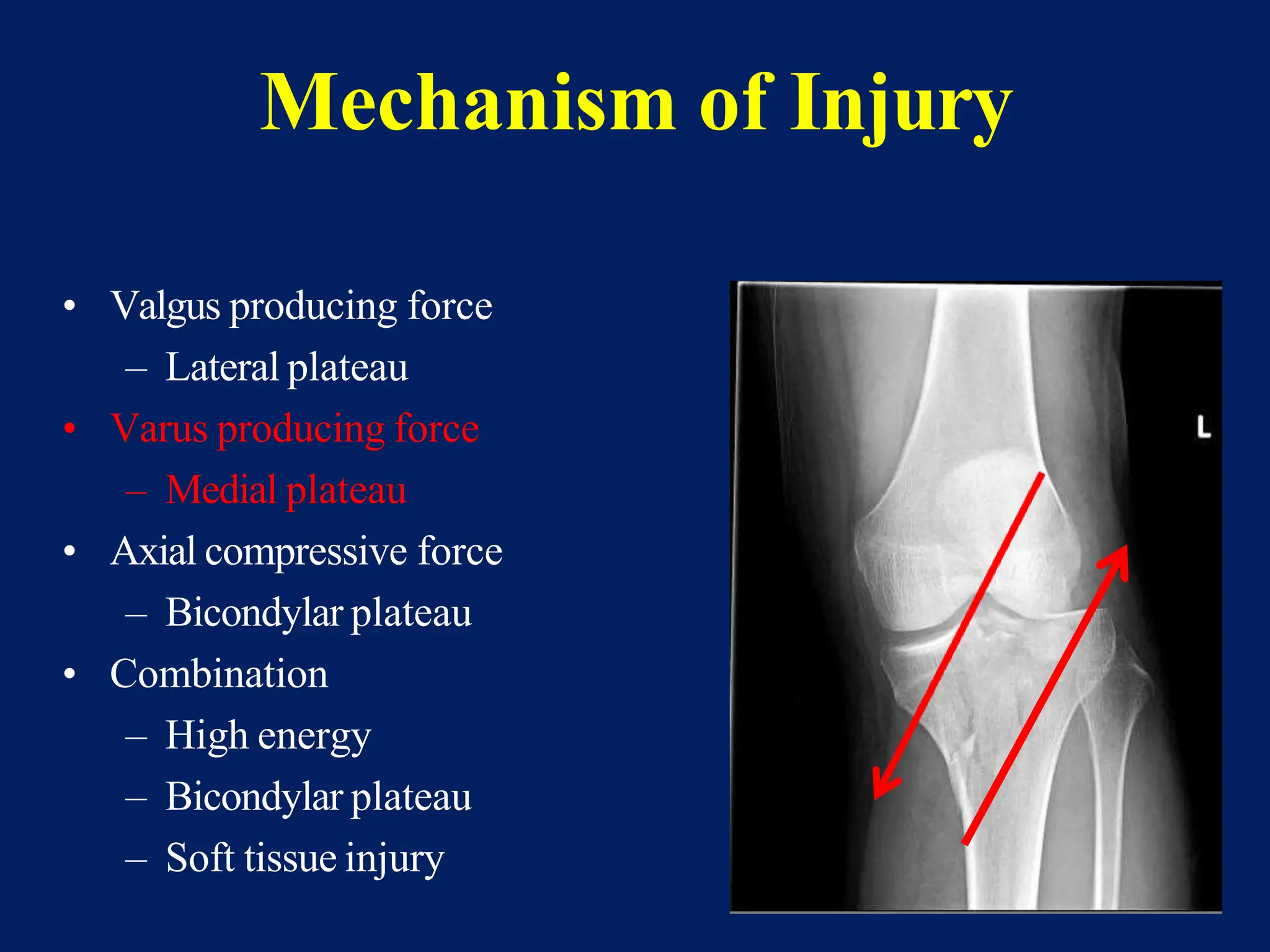
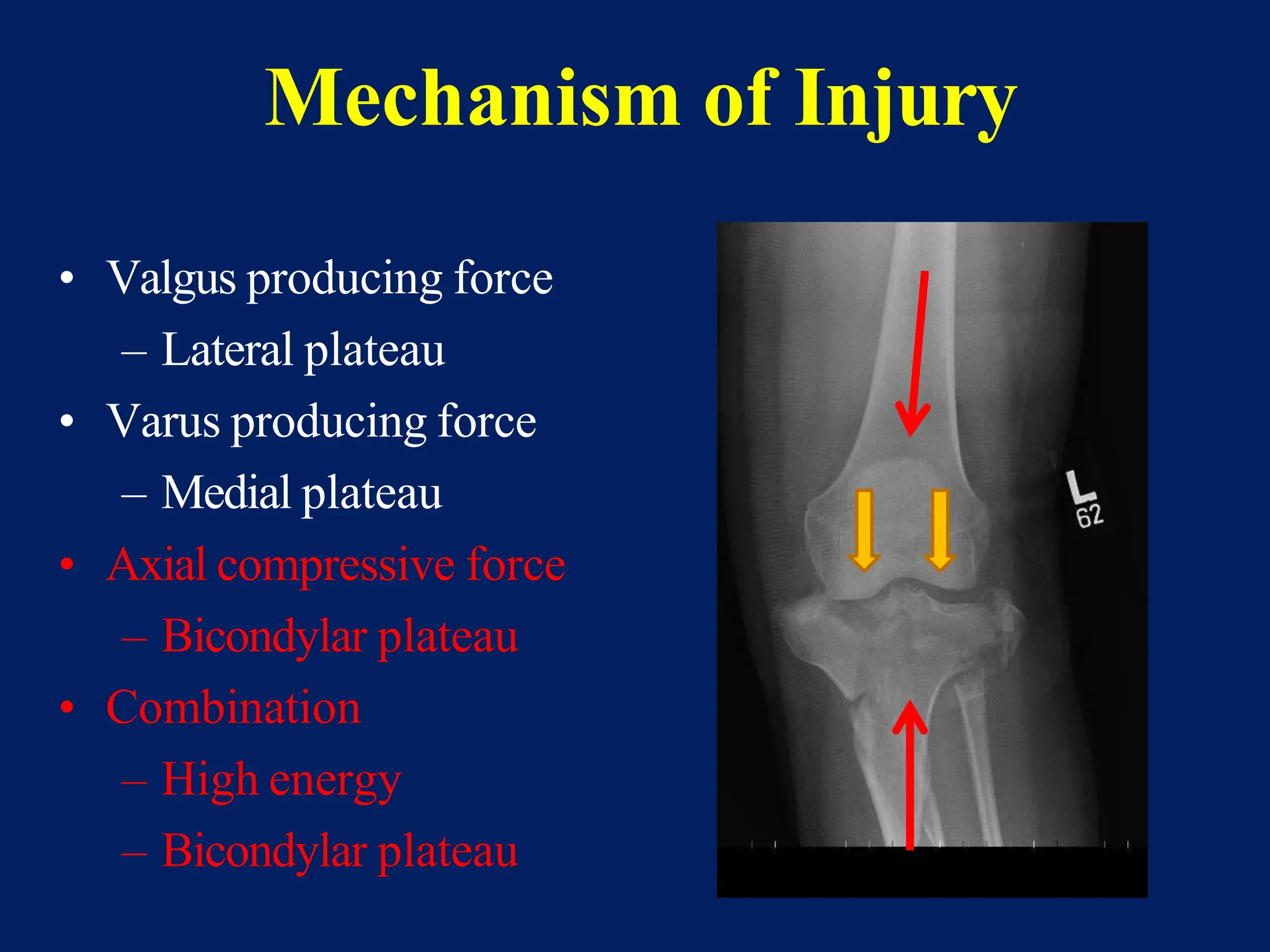
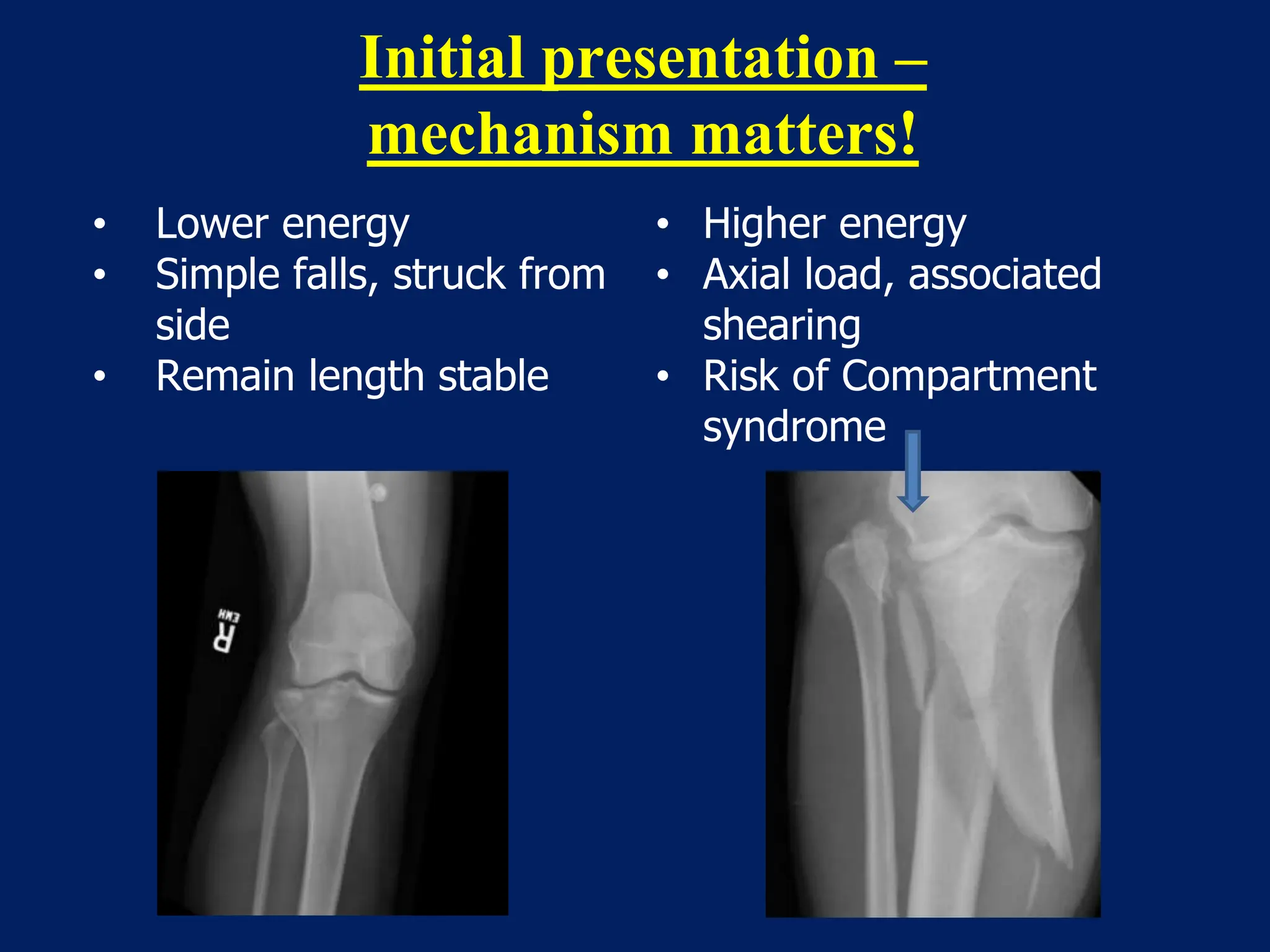
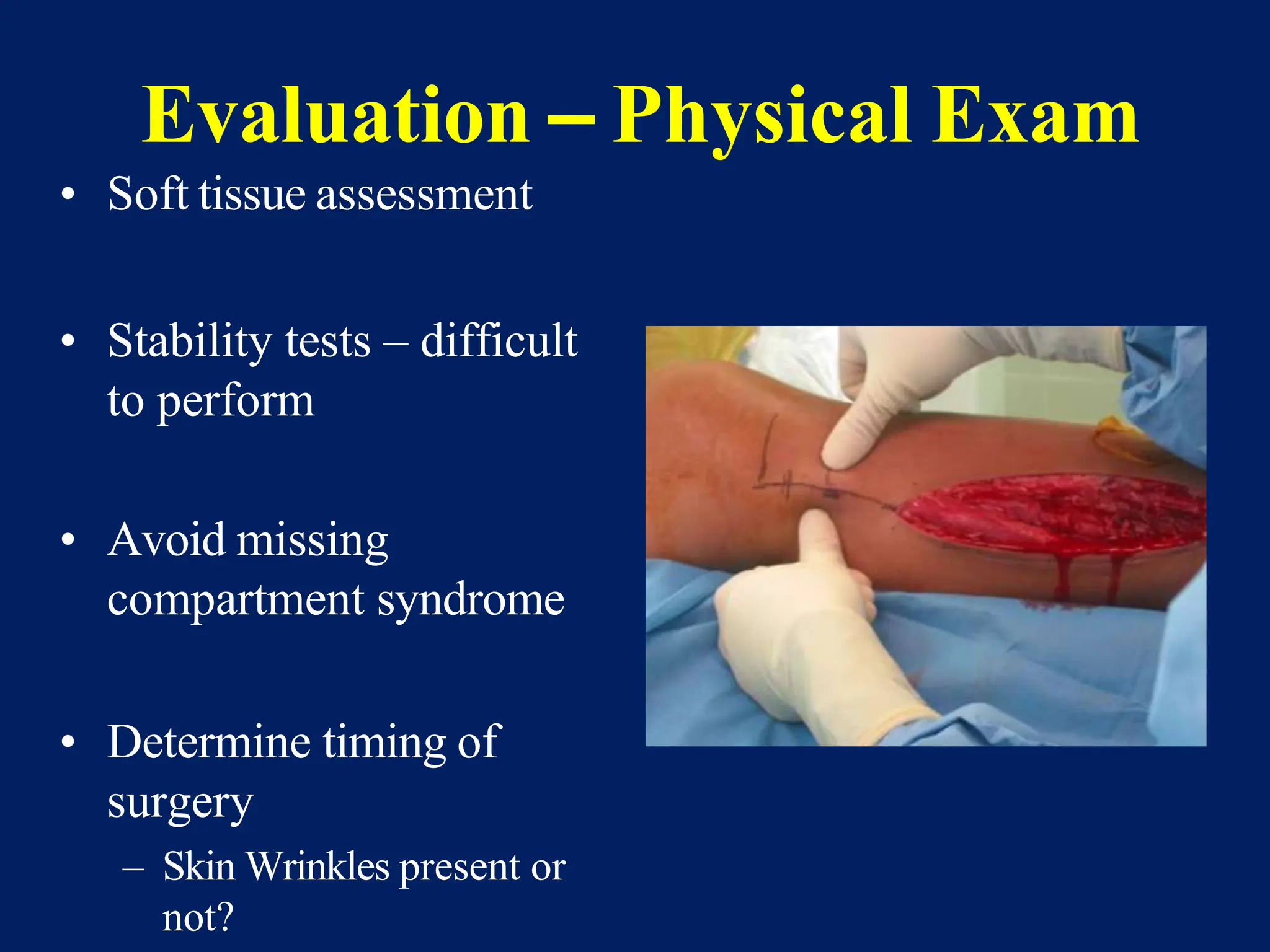
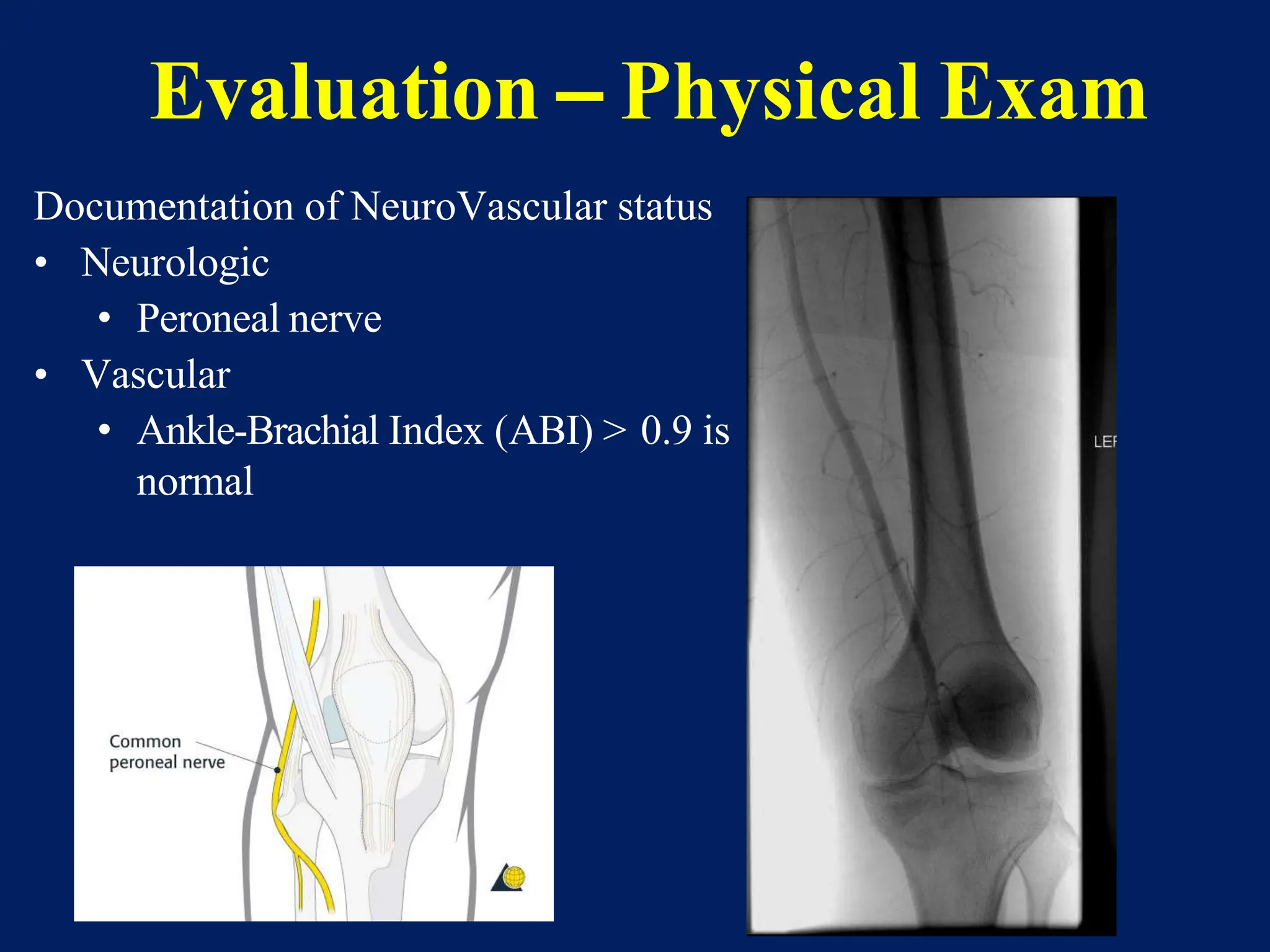
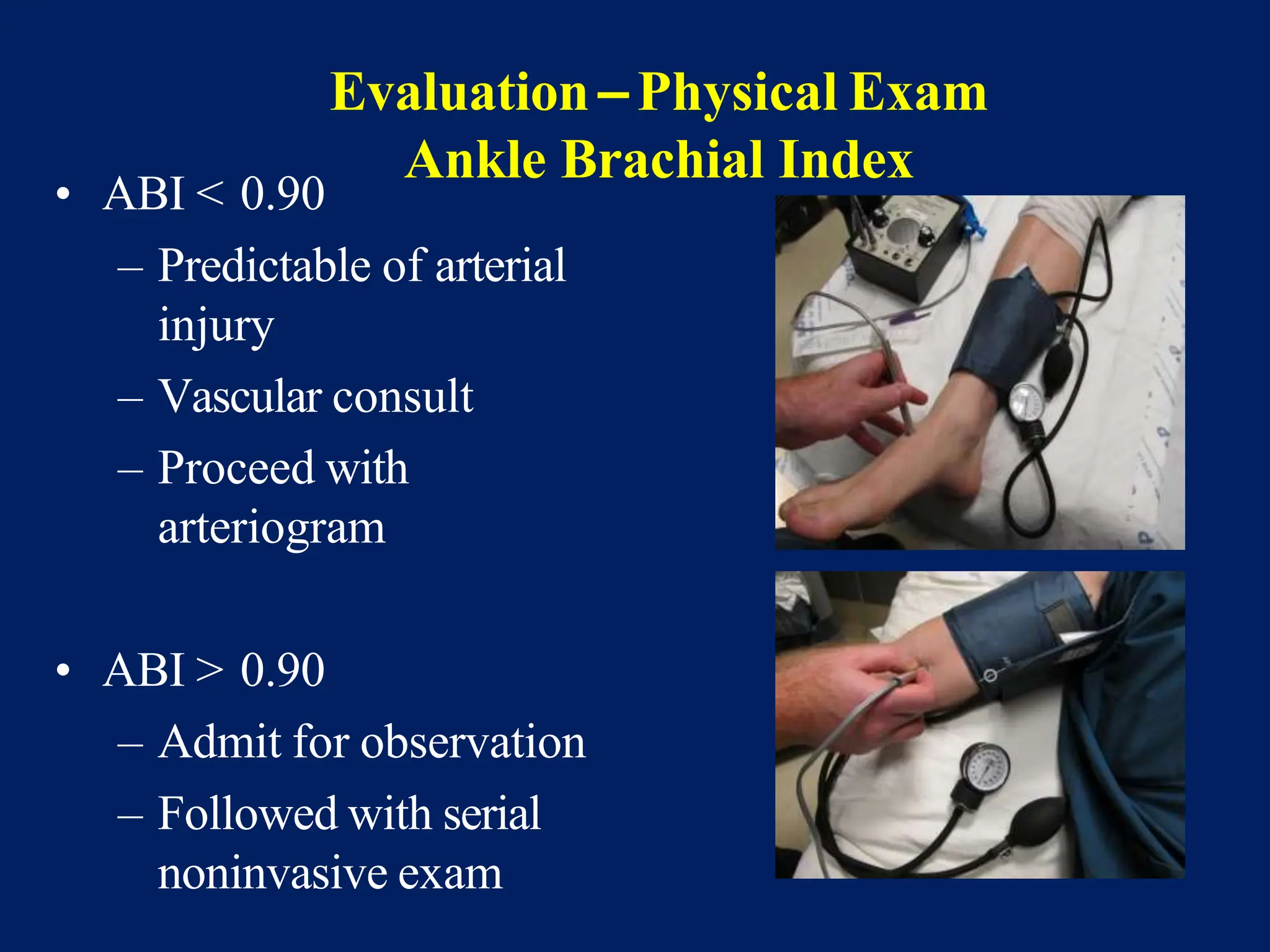
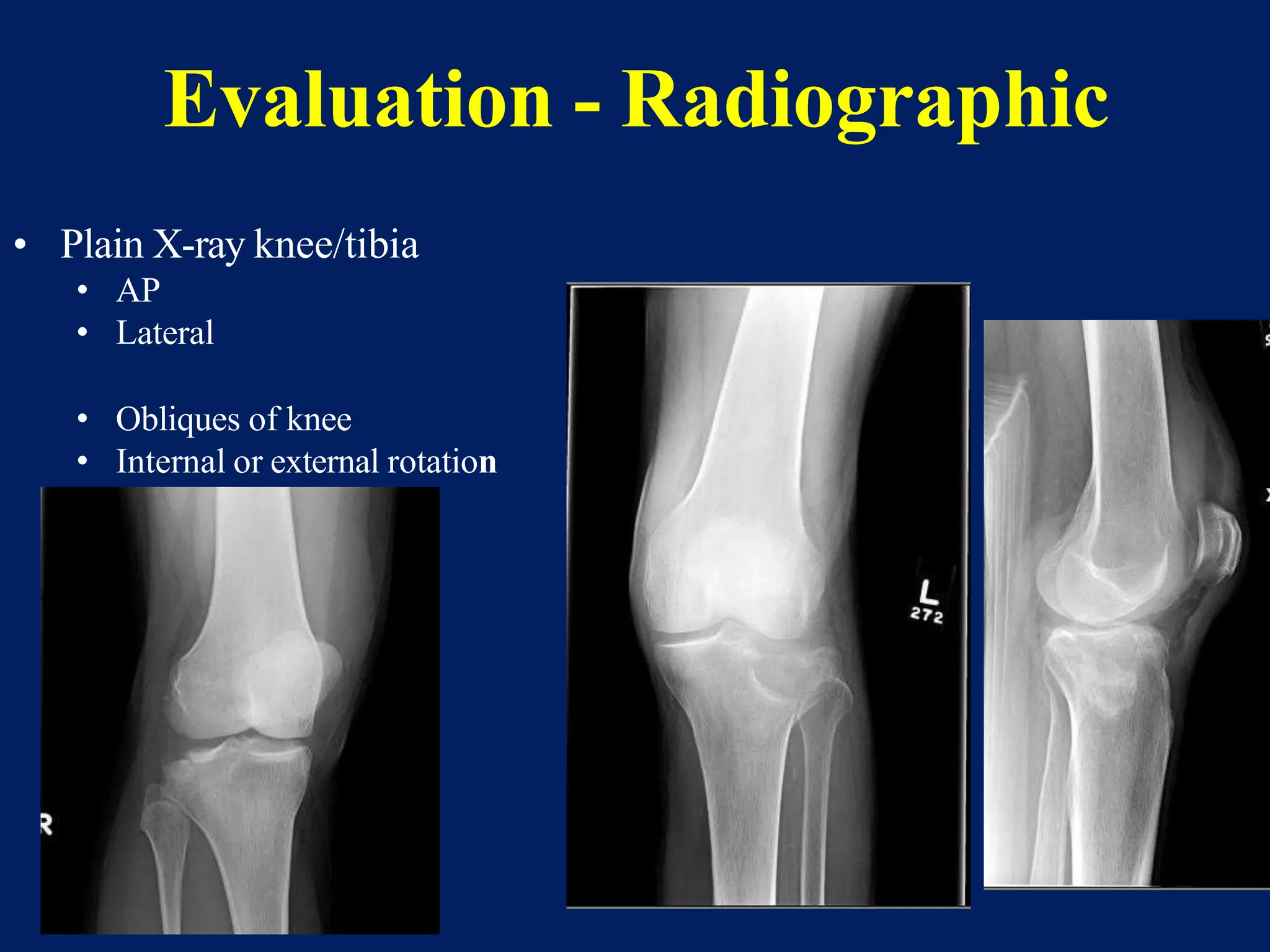
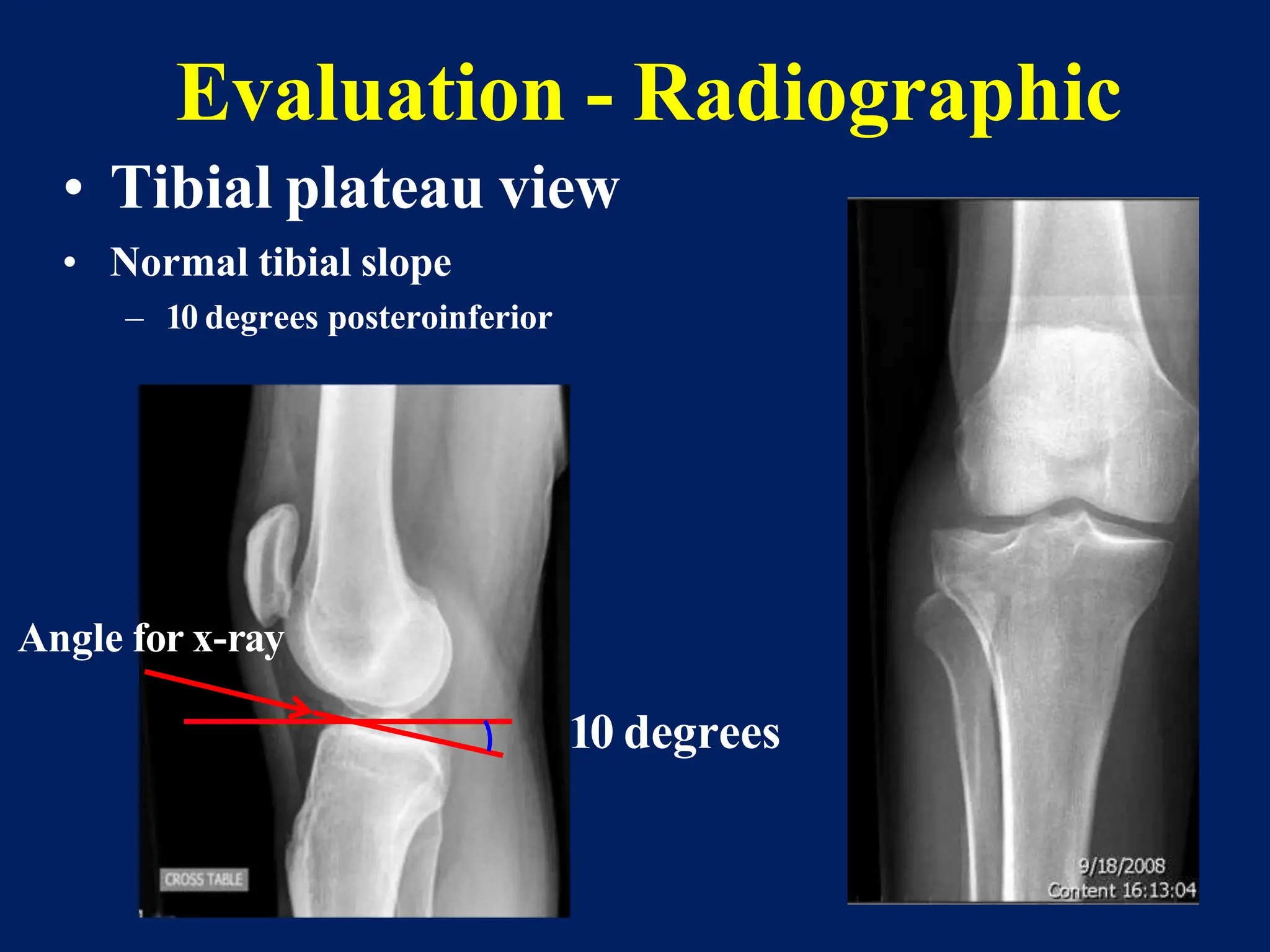
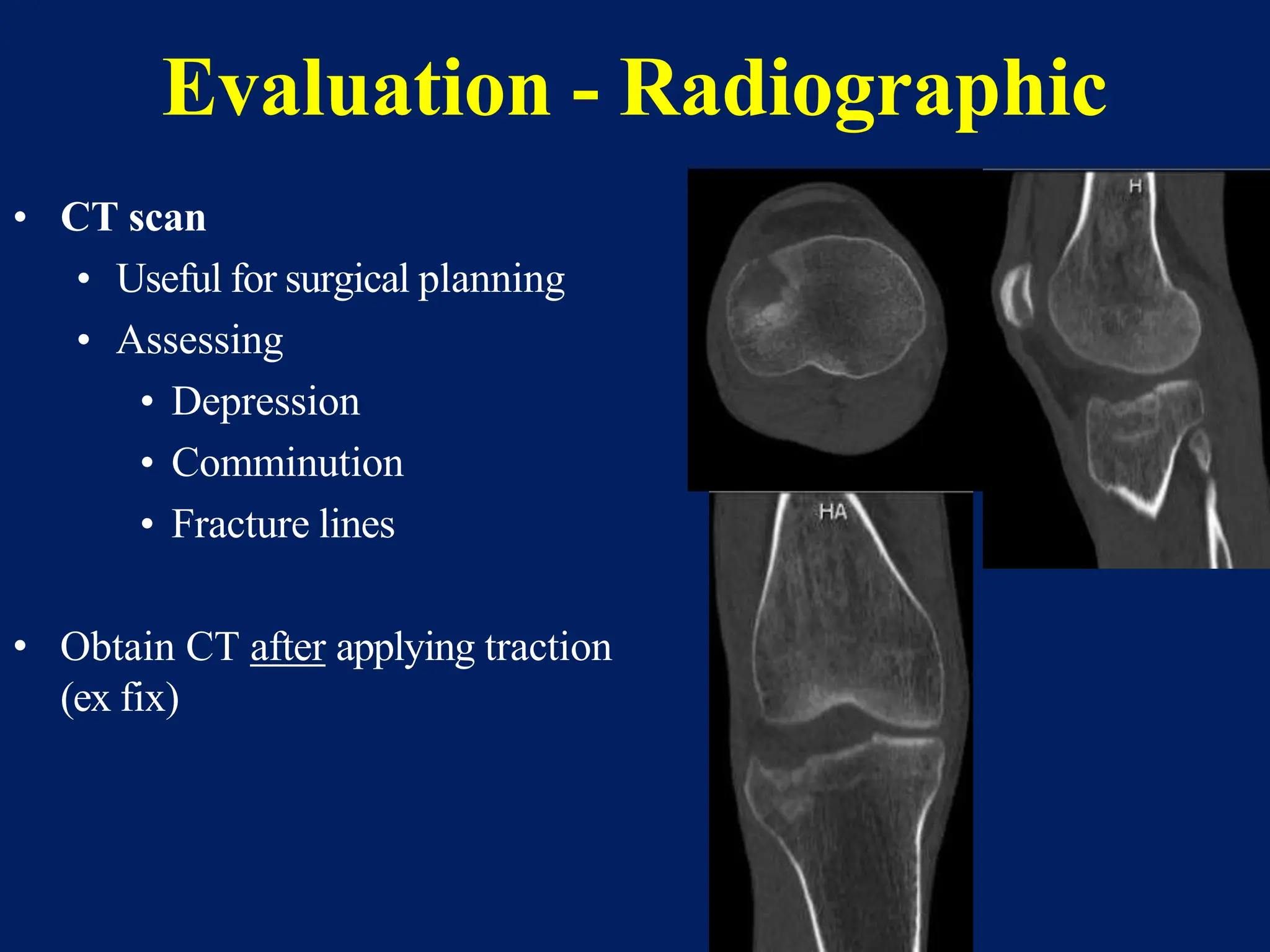
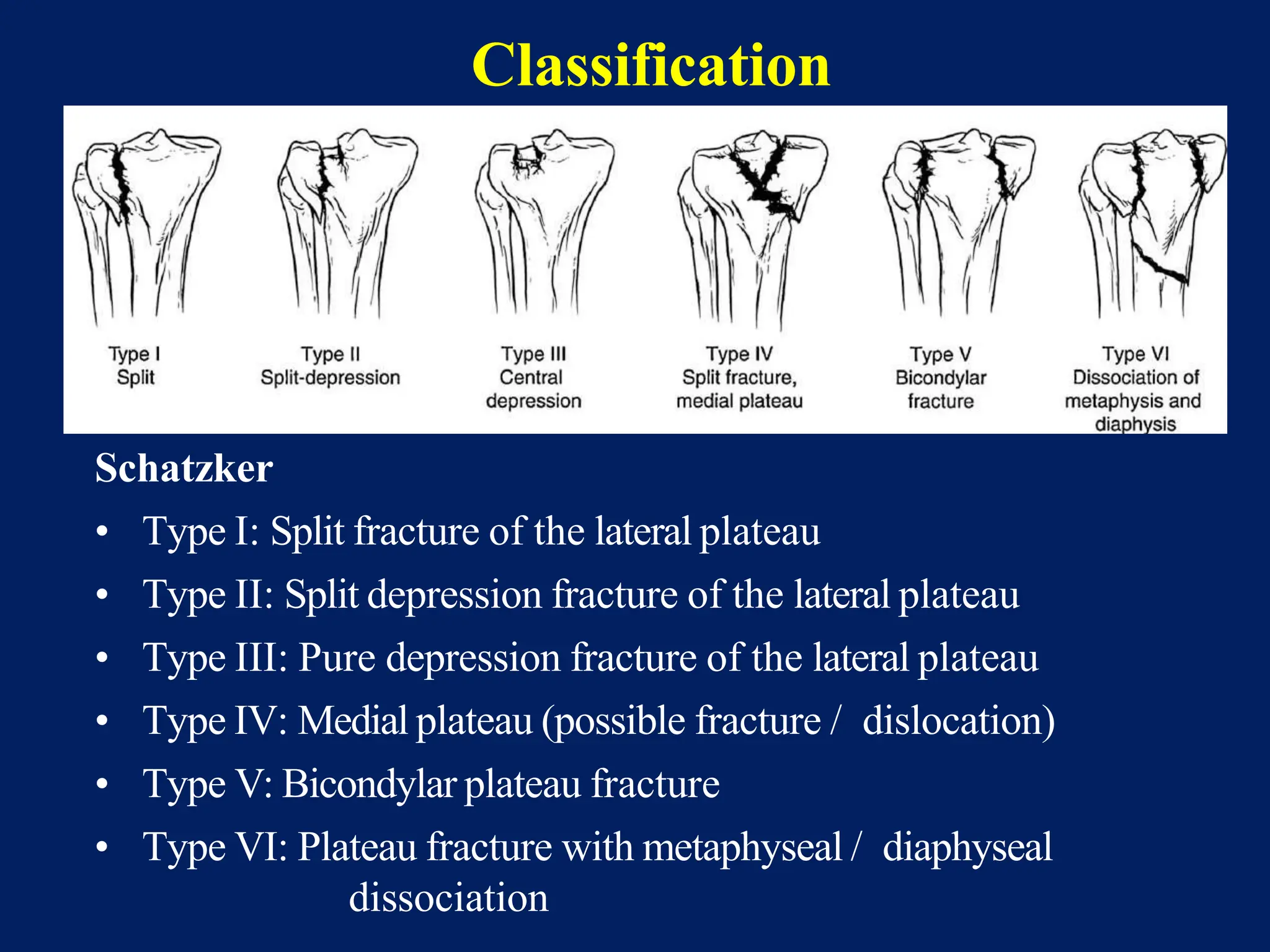
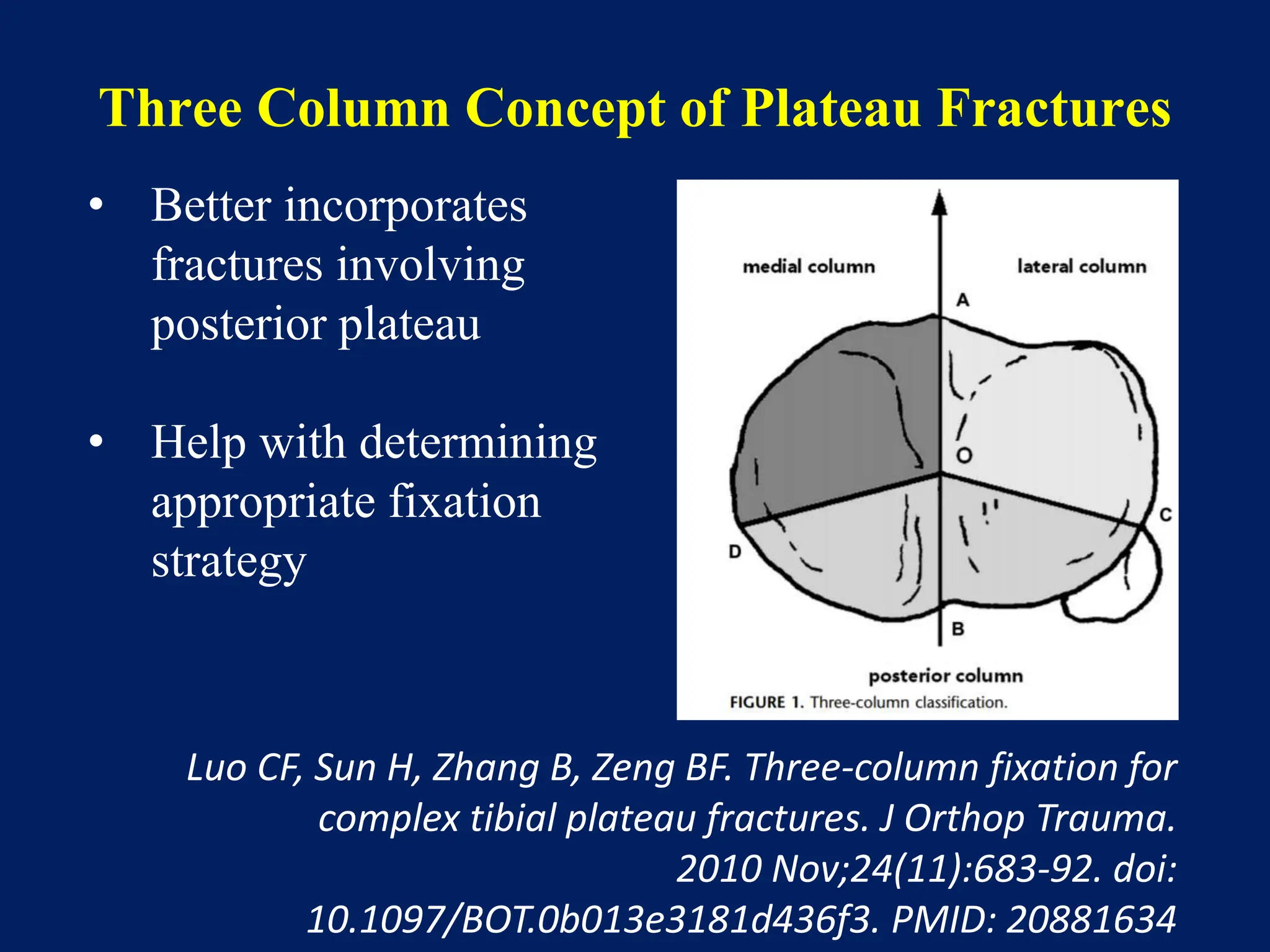
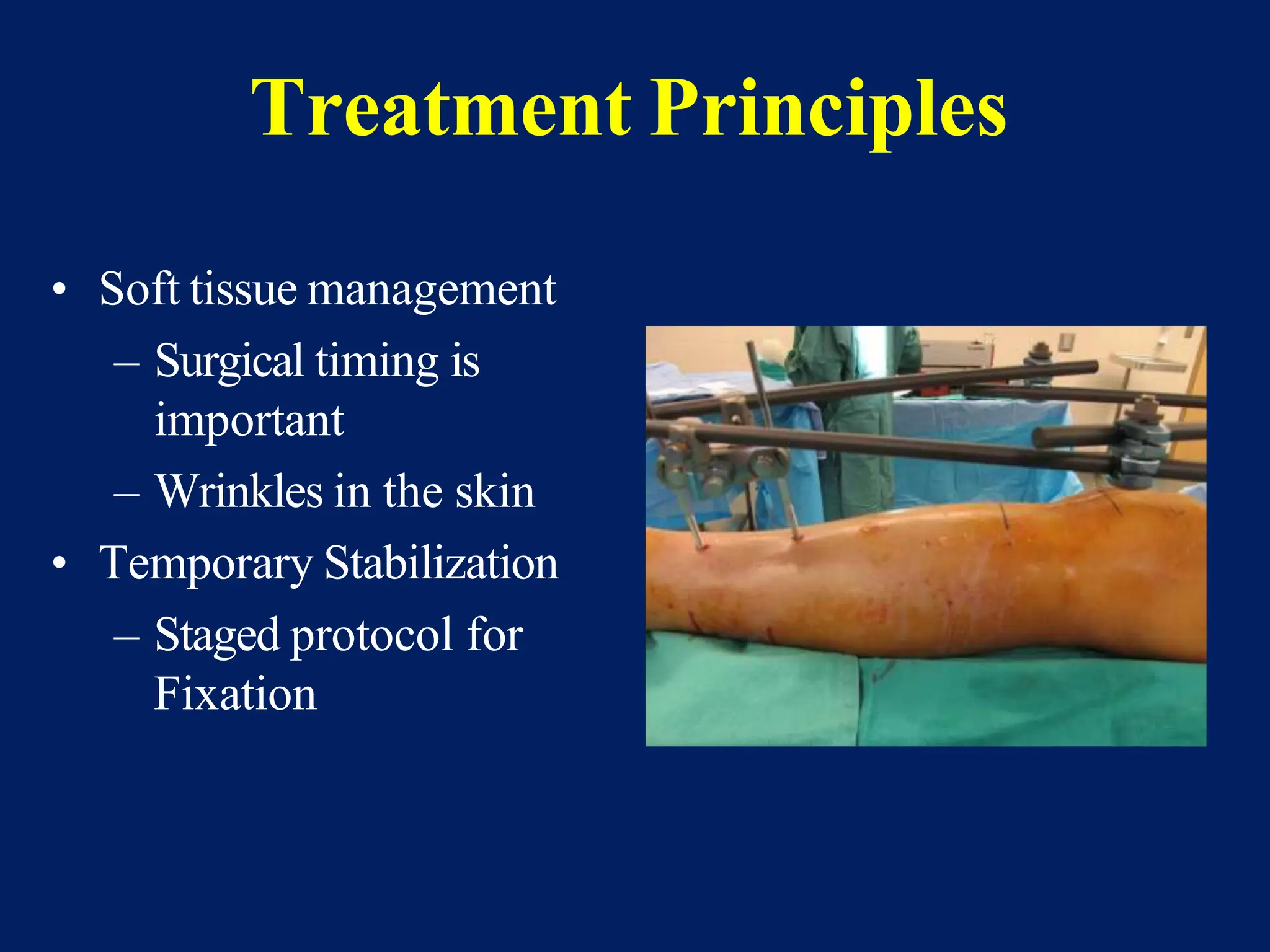
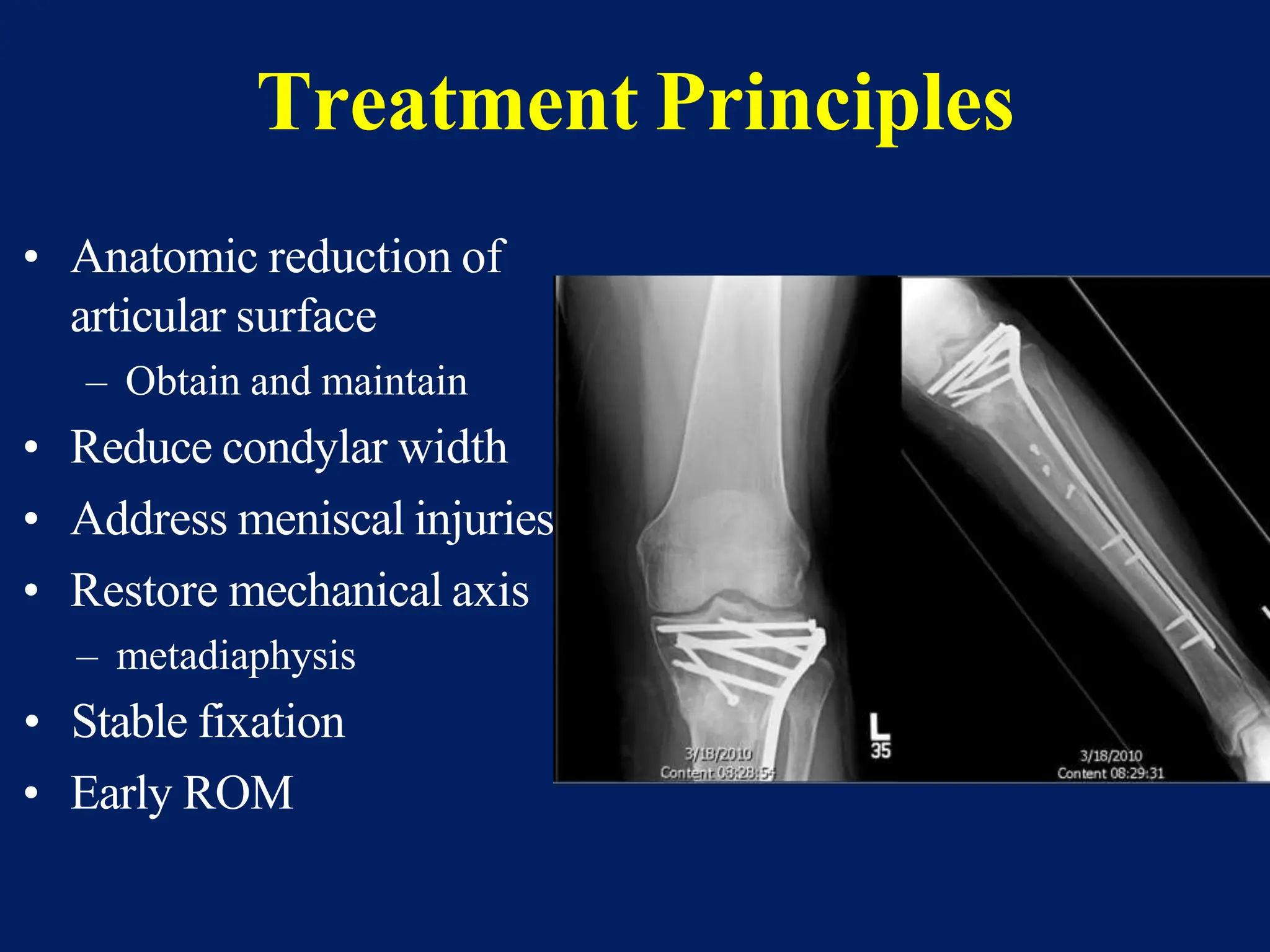
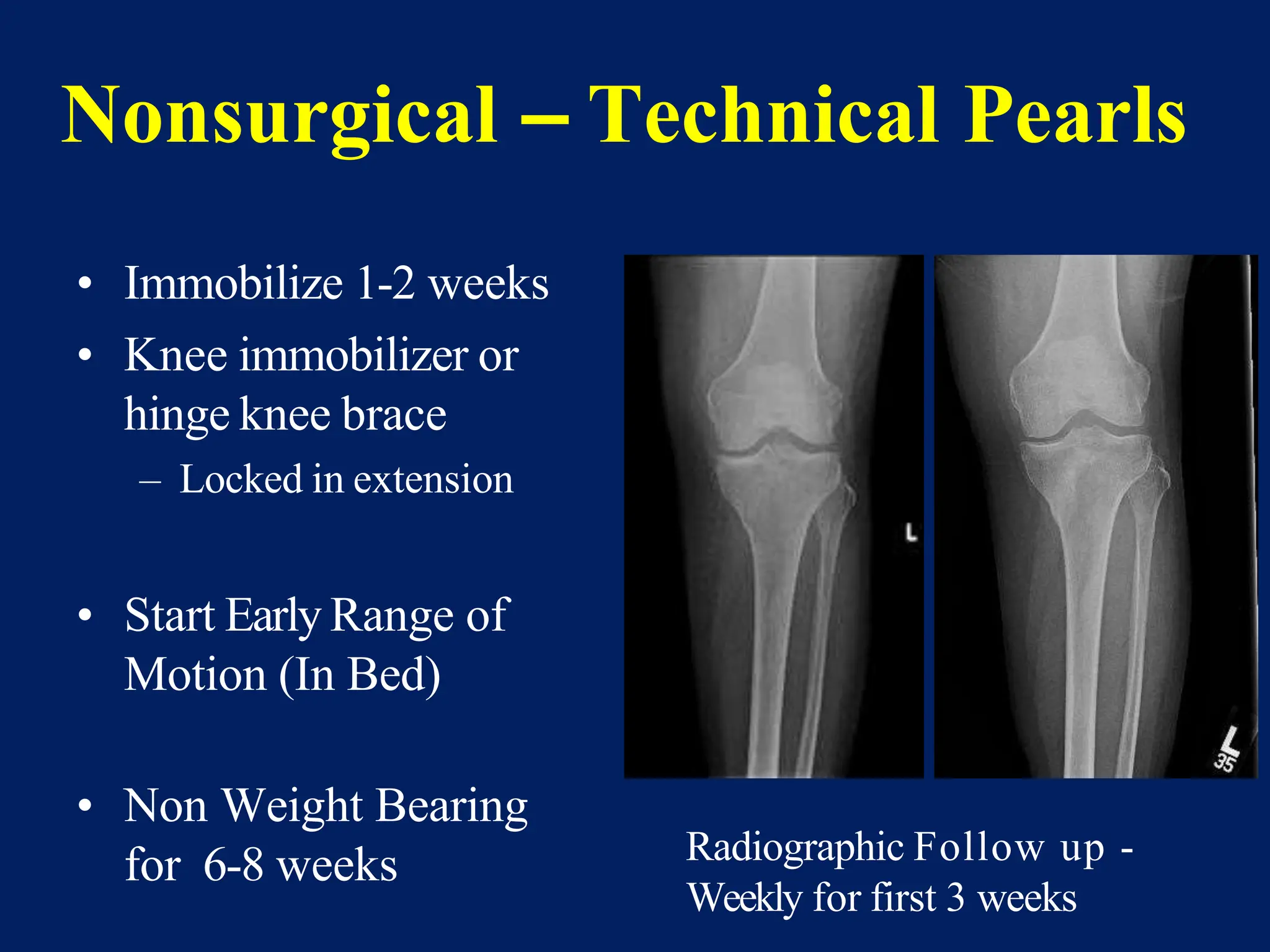
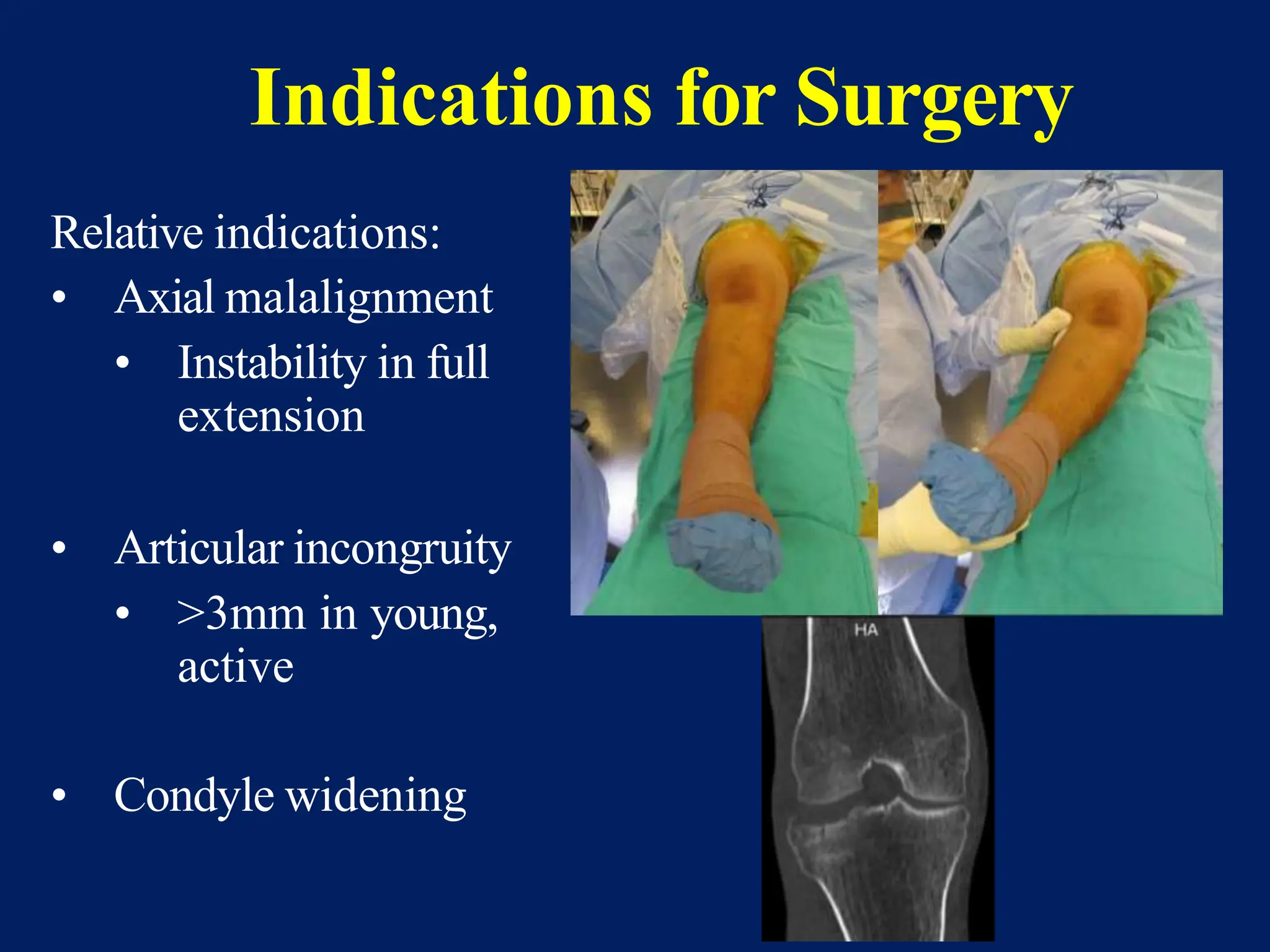
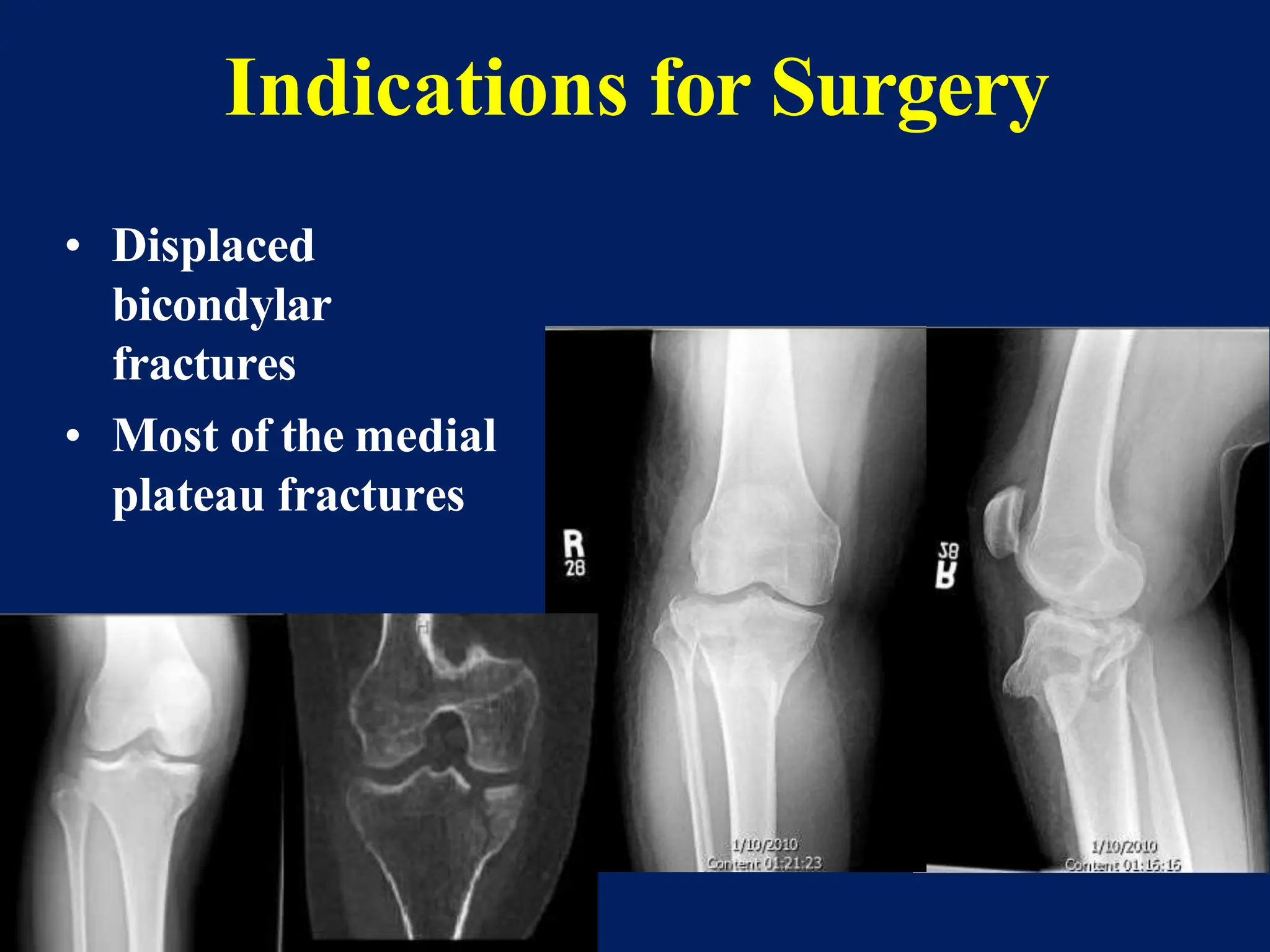
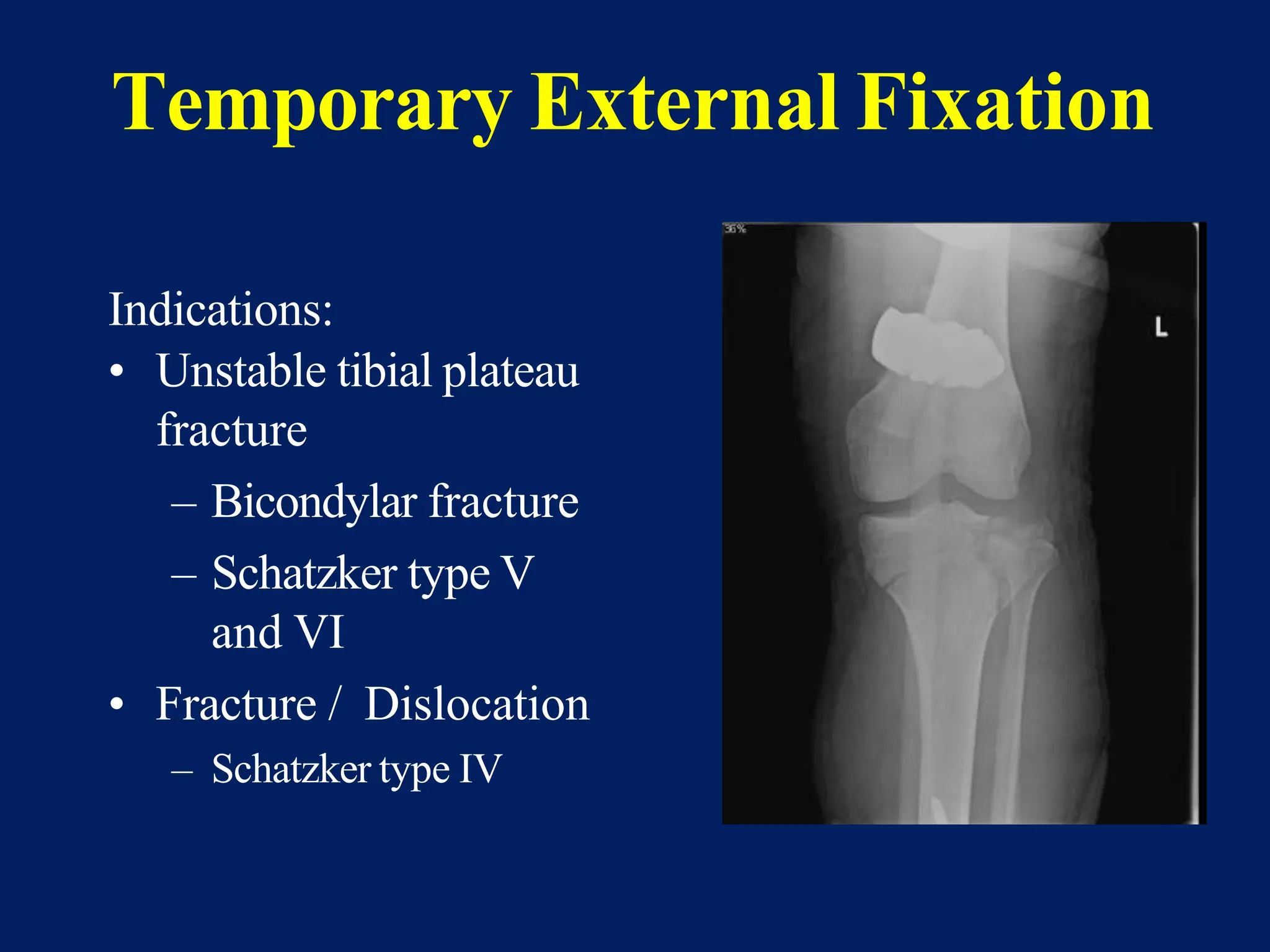
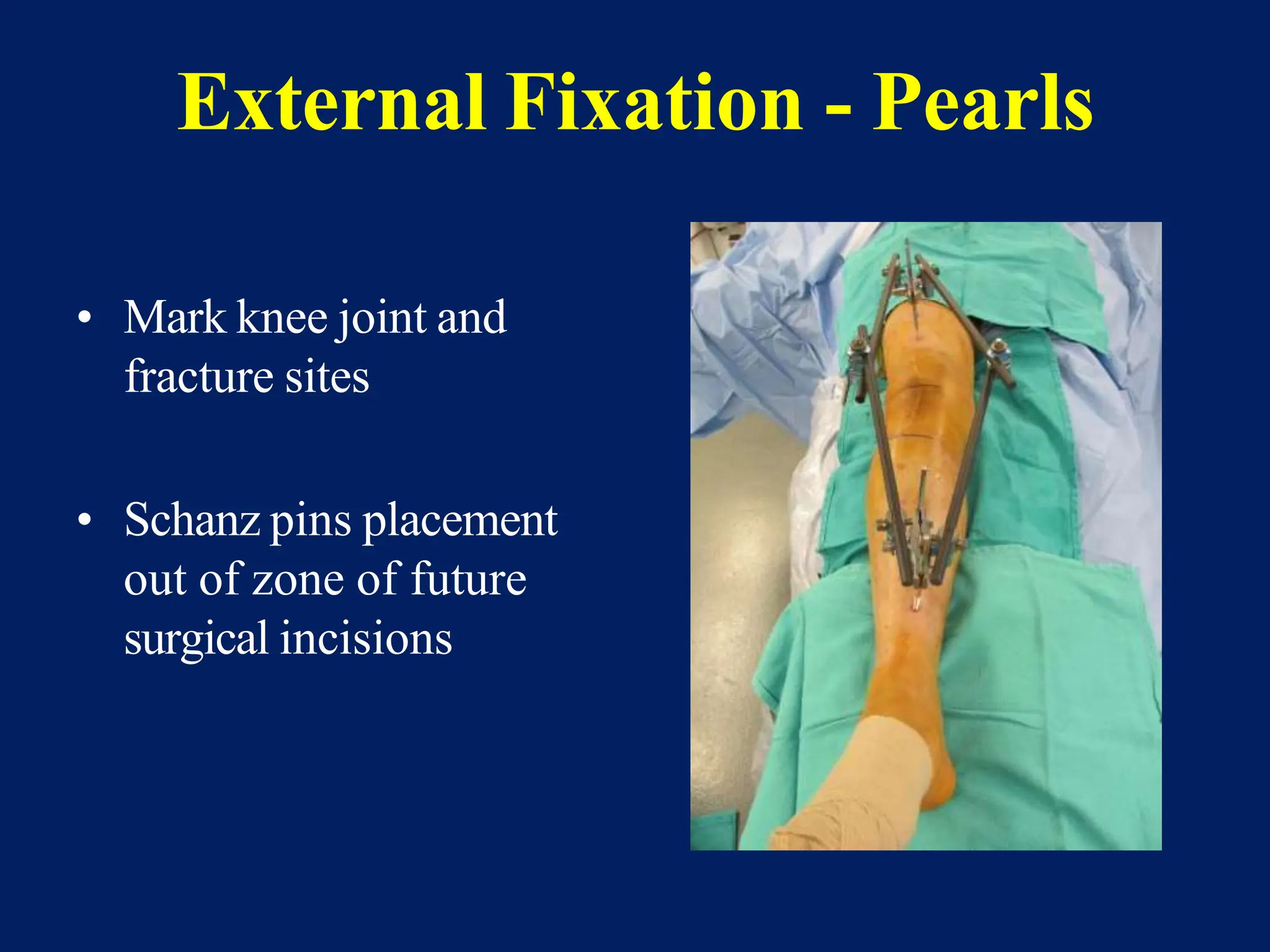
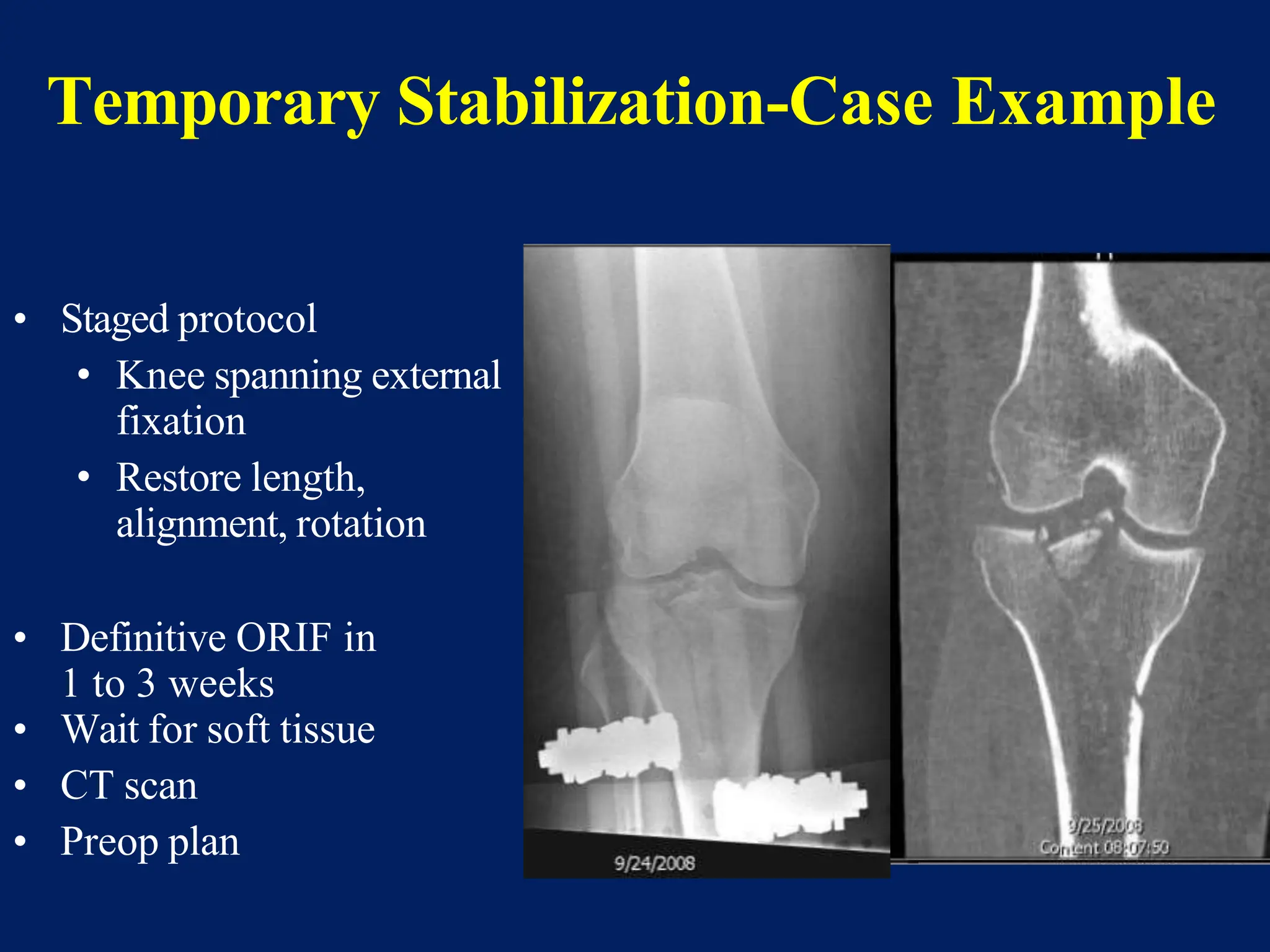
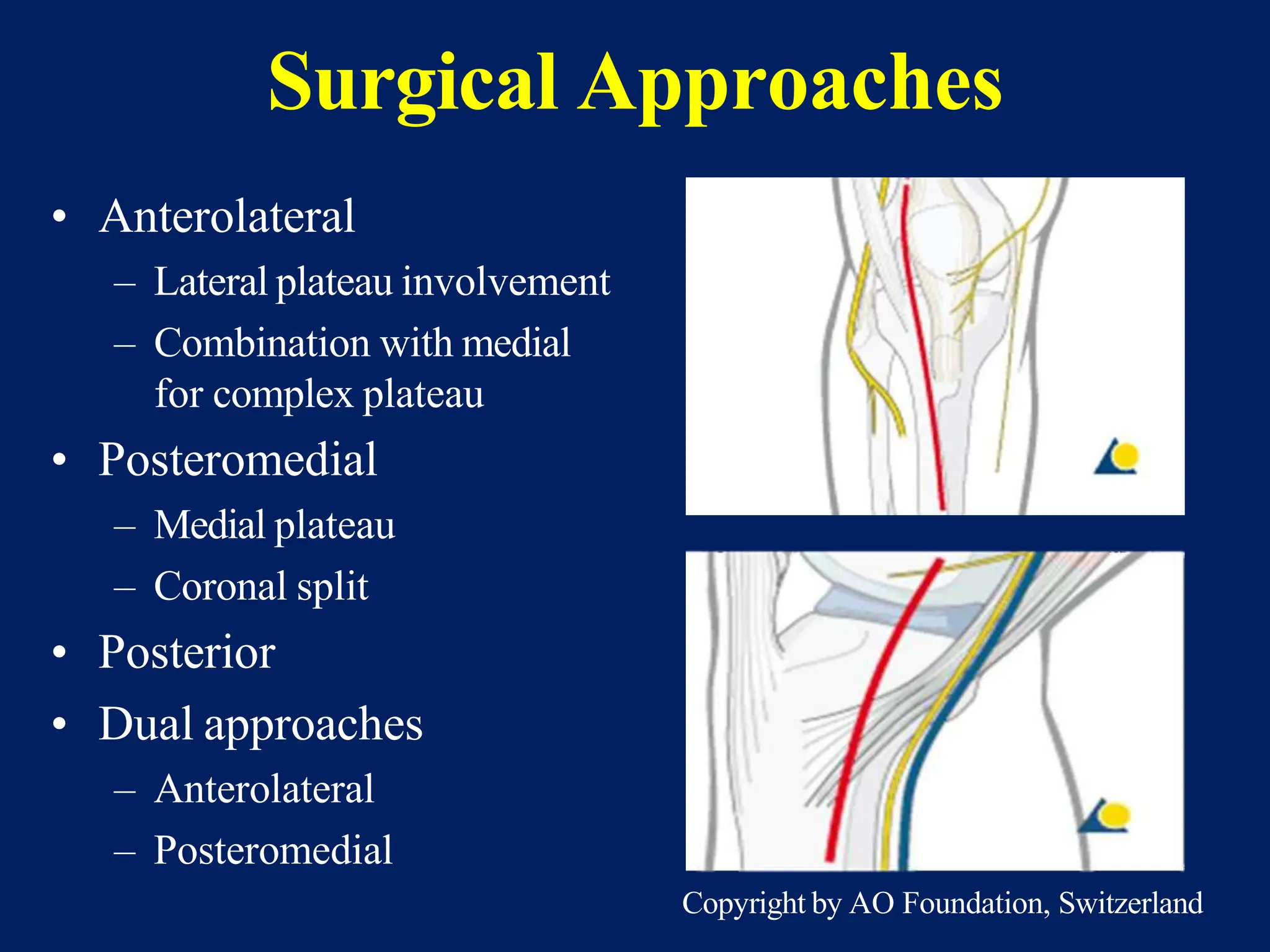
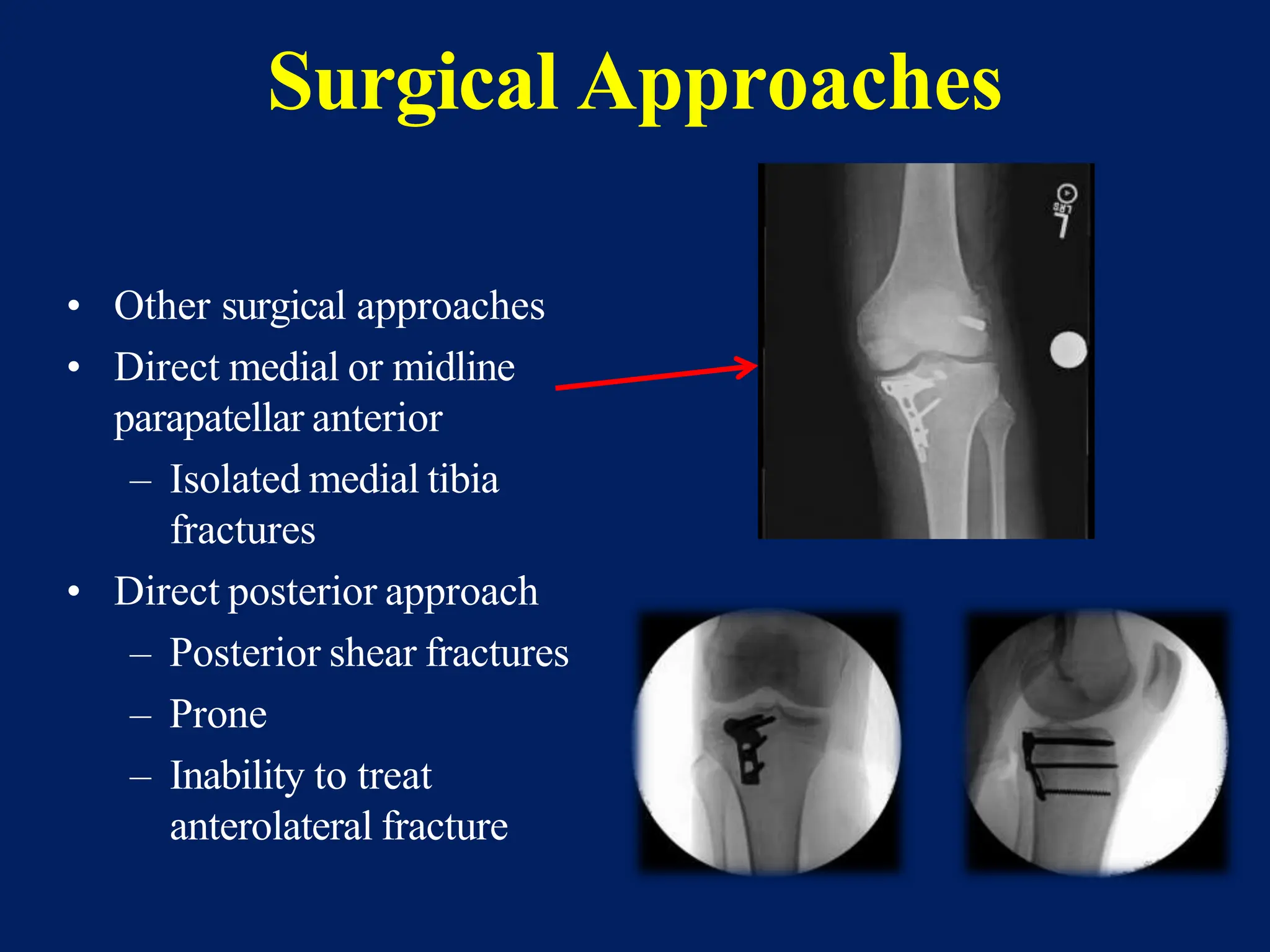
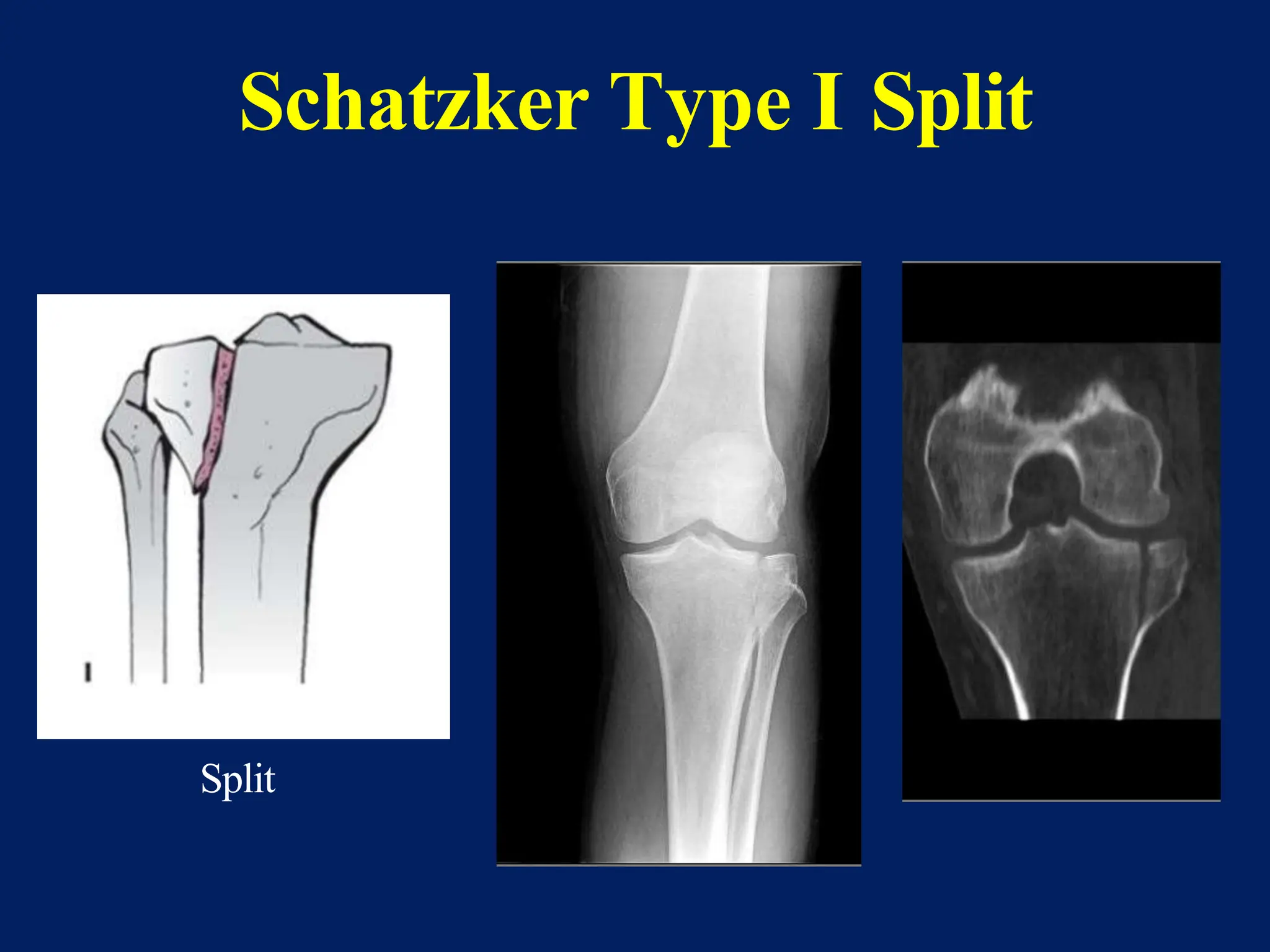
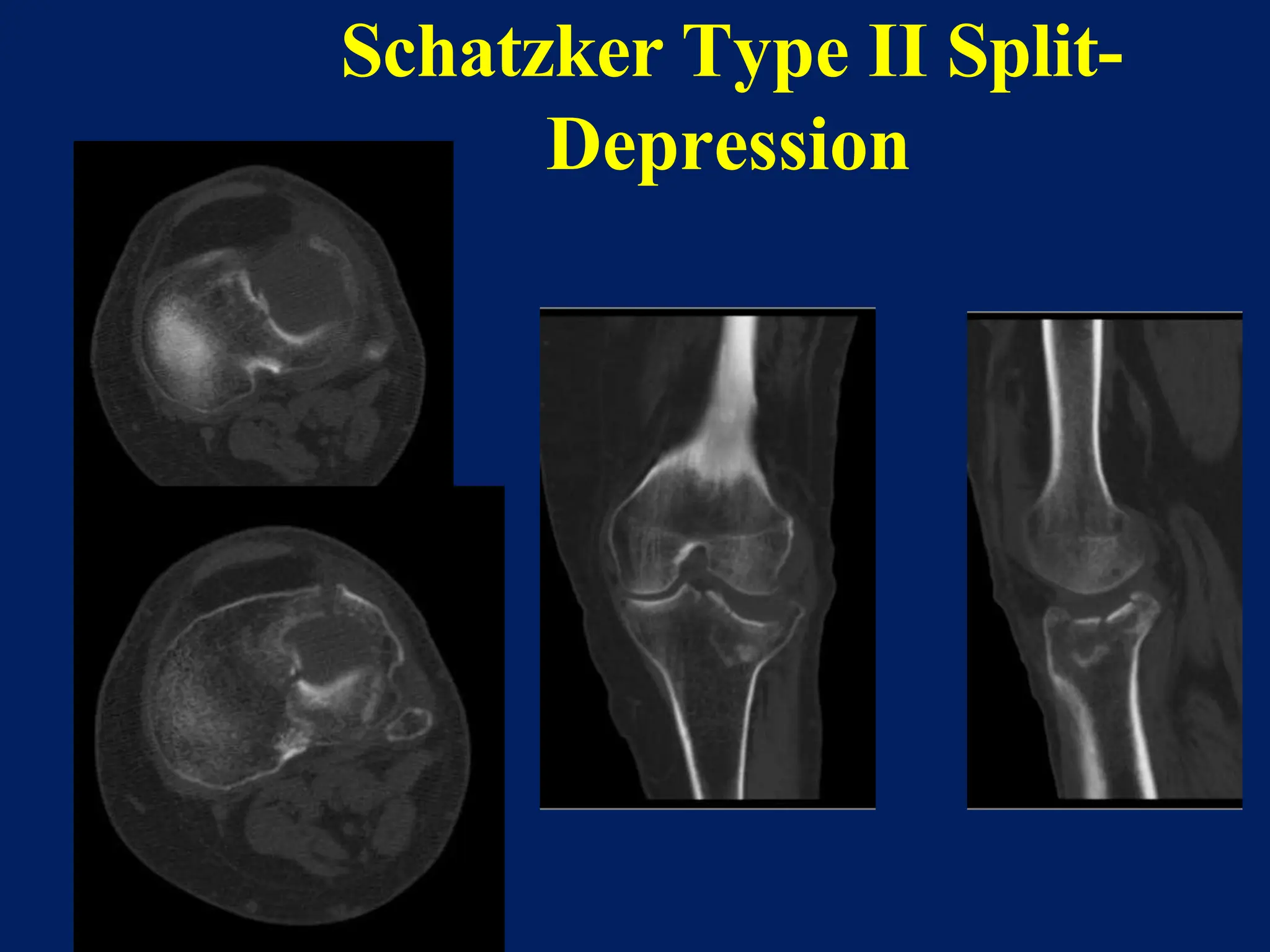
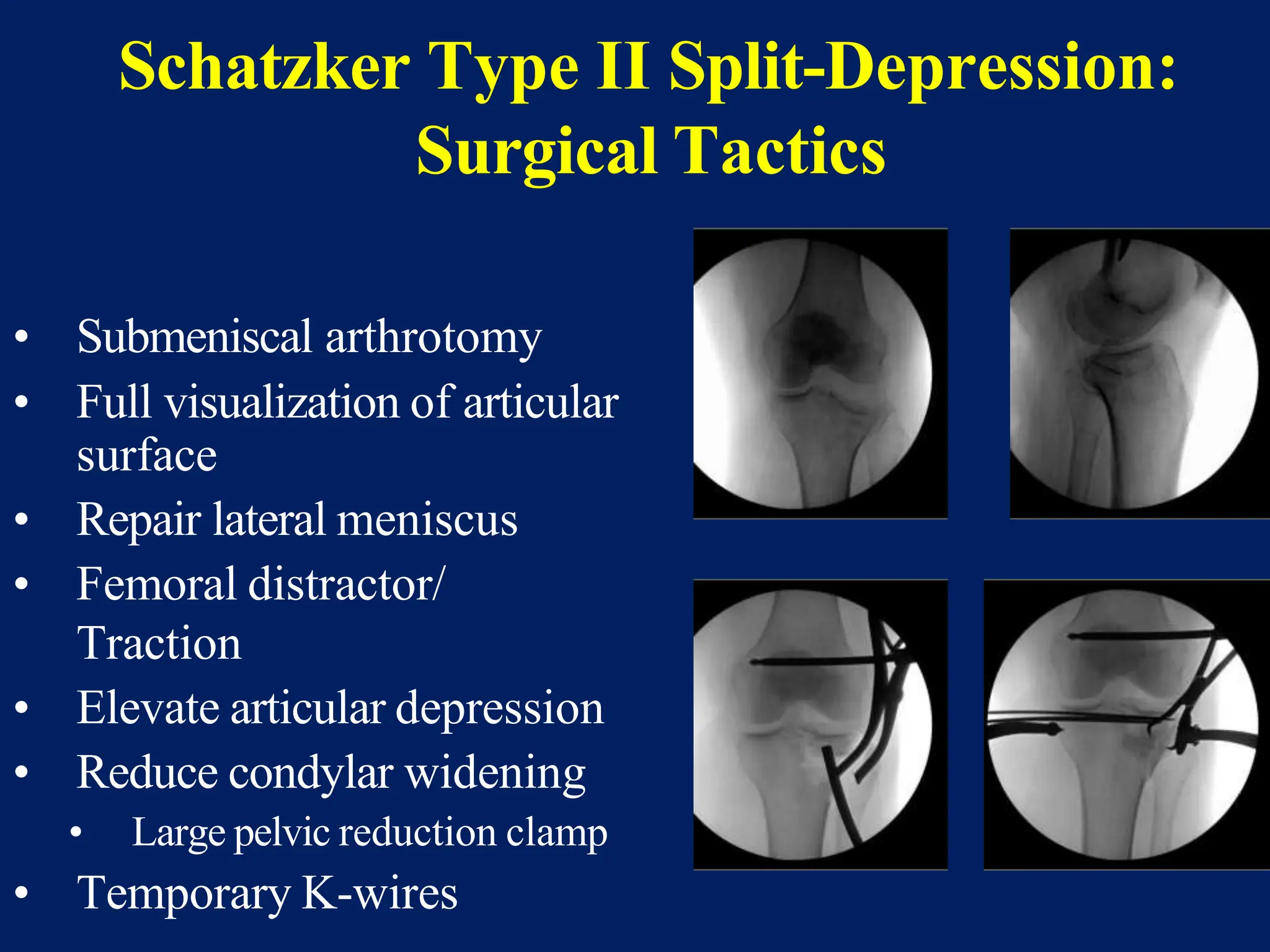
The document discusses proximal tibia fractures, covering their anatomy, mechanisms of injury, evaluation methods, and treatment principles. It emphasizes the importance of recognizing fracture patterns like partial and complete articular fractures and outlines surgical approaches, including external fixation and open reduction internal fixation techniques. The document also highlights rehabilitation, potential complications, and includes case studies for practical understanding.