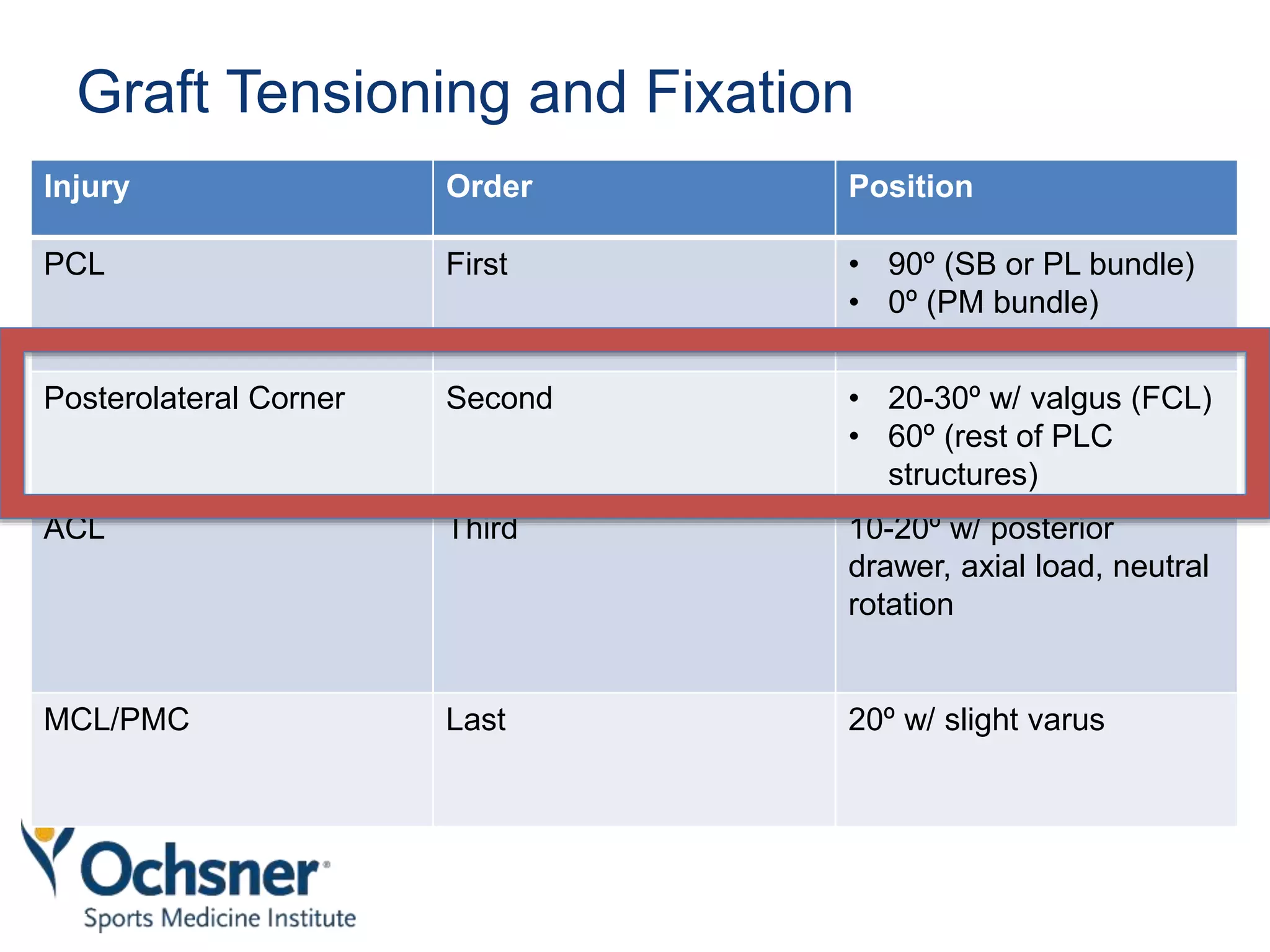
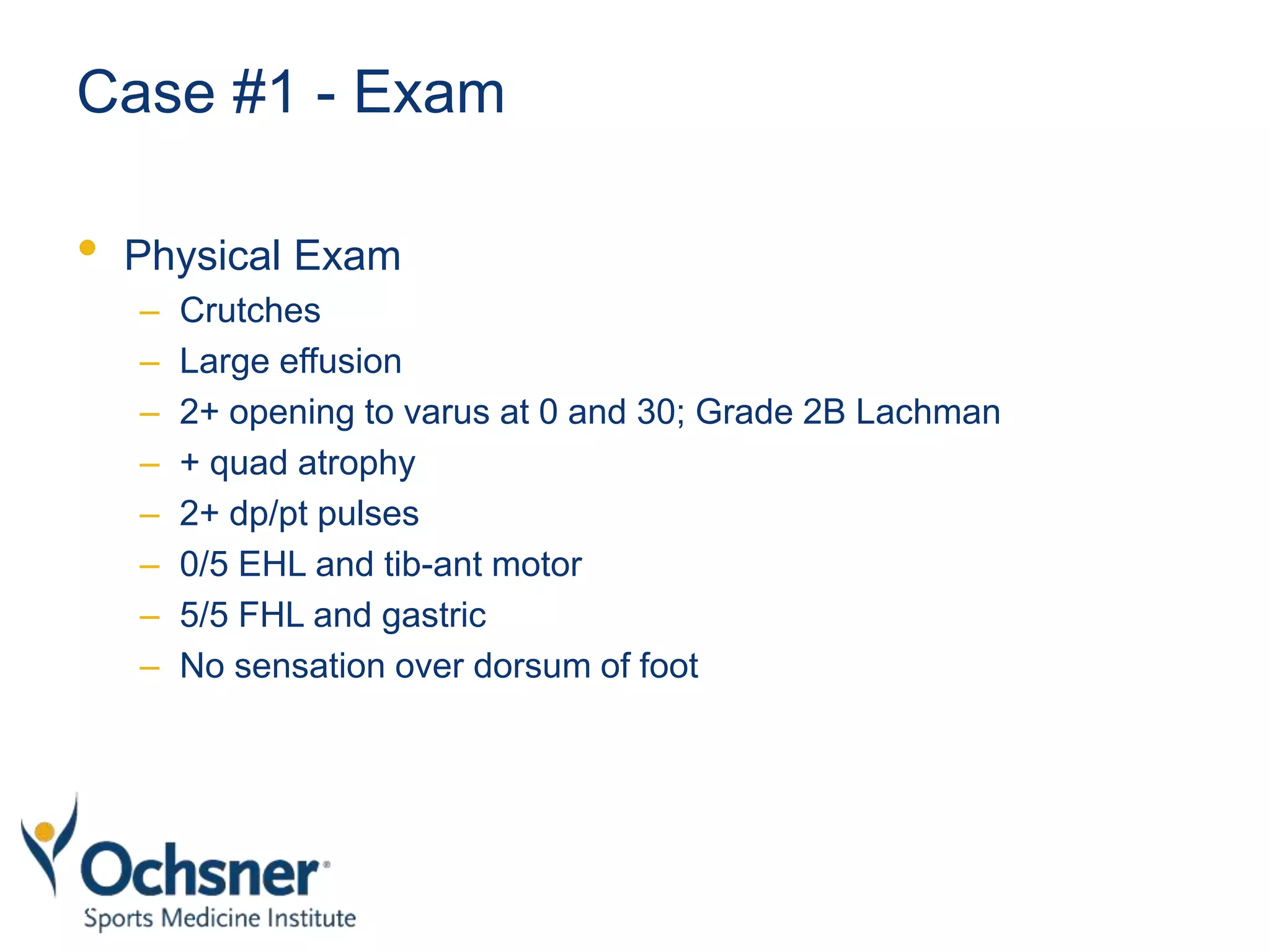
The document discusses a case study of a 17-year-old male football player who suffered a knee injury and highlights the evaluation and treatment of multiple ligament knee injuries, particularly focusing on posterolateral corner reconstruction. It outlines treatment options, surgical timing, and rehabilitation protocols, emphasizing the advantages of operative treatment over non-operative methods. The document also includes specific graft types and techniques utilized in surgical interventions and rehabilitation timelines for recovery.