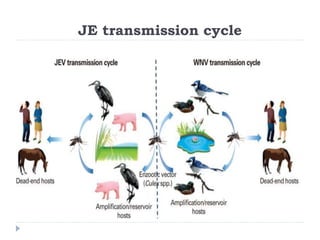
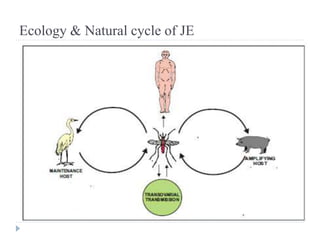
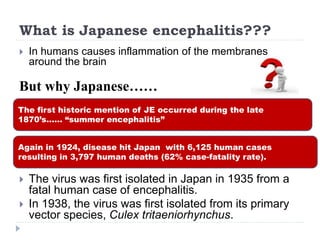
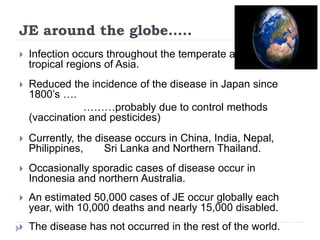
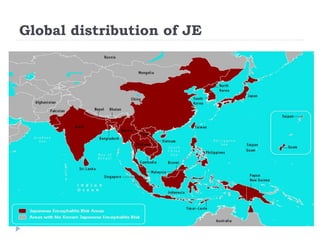
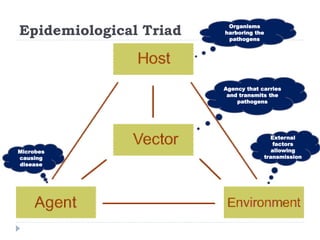
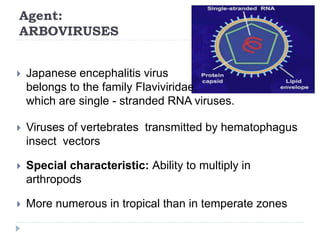
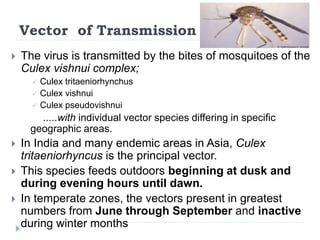
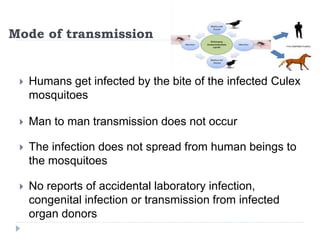
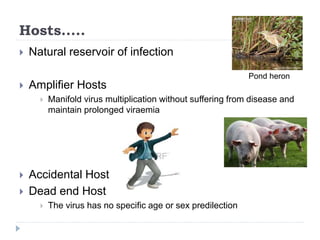
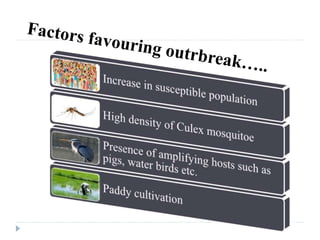
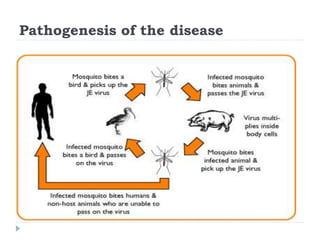
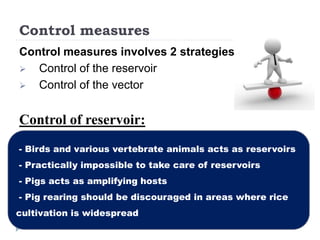
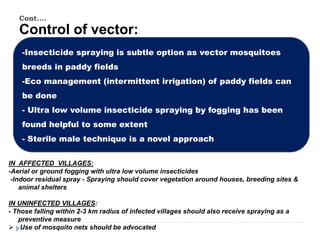
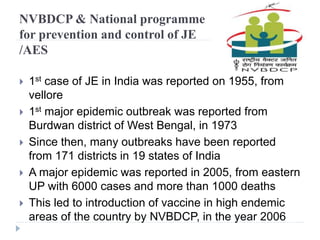
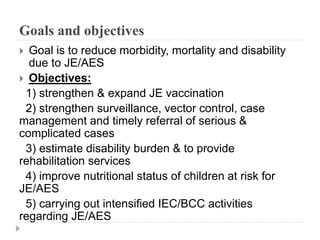
Japanese encephalitis is a mosquito-borne viral disease that infects humans and animals. The virus is maintained in a transmission cycle between mosquito vectors, such as Culex tritaeniorhynchus, and vertebrate hosts like birds and pigs. The disease is most common in Asia and causes brain inflammation that can lead to death or long-term neurological problems in about 20-30% of cases. Prevention strategies focus on controlling the mosquito vector population and vaccinating people in endemic areas.