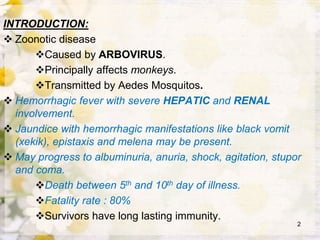
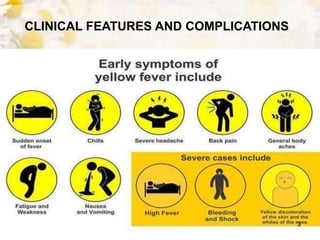
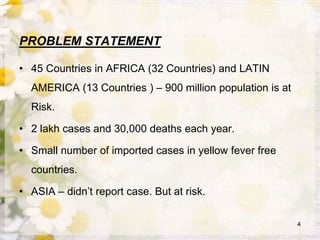
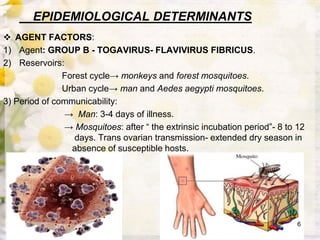
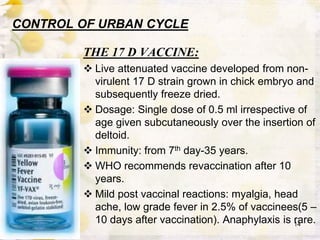
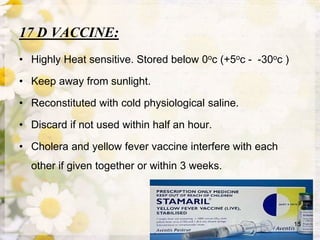
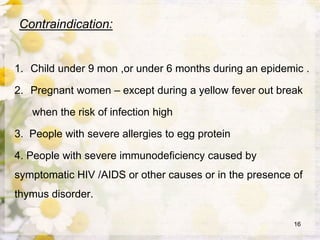
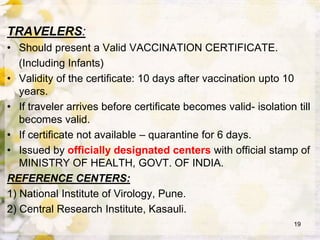
This document discusses yellow fever, a viral hemorrhagic disease transmitted by Aedes mosquitoes. It is caused by a flavivirus that primarily affects monkeys but can infect humans. The disease causes liver and kidney damage that can lead to jaundice, hemorrhaging, and death in 20-50% of cases. It is found in tropical areas of Africa and South America. Prevention relies on vaccination and controlling the Aedes aegypti mosquito vector through environmental management and insecticides.