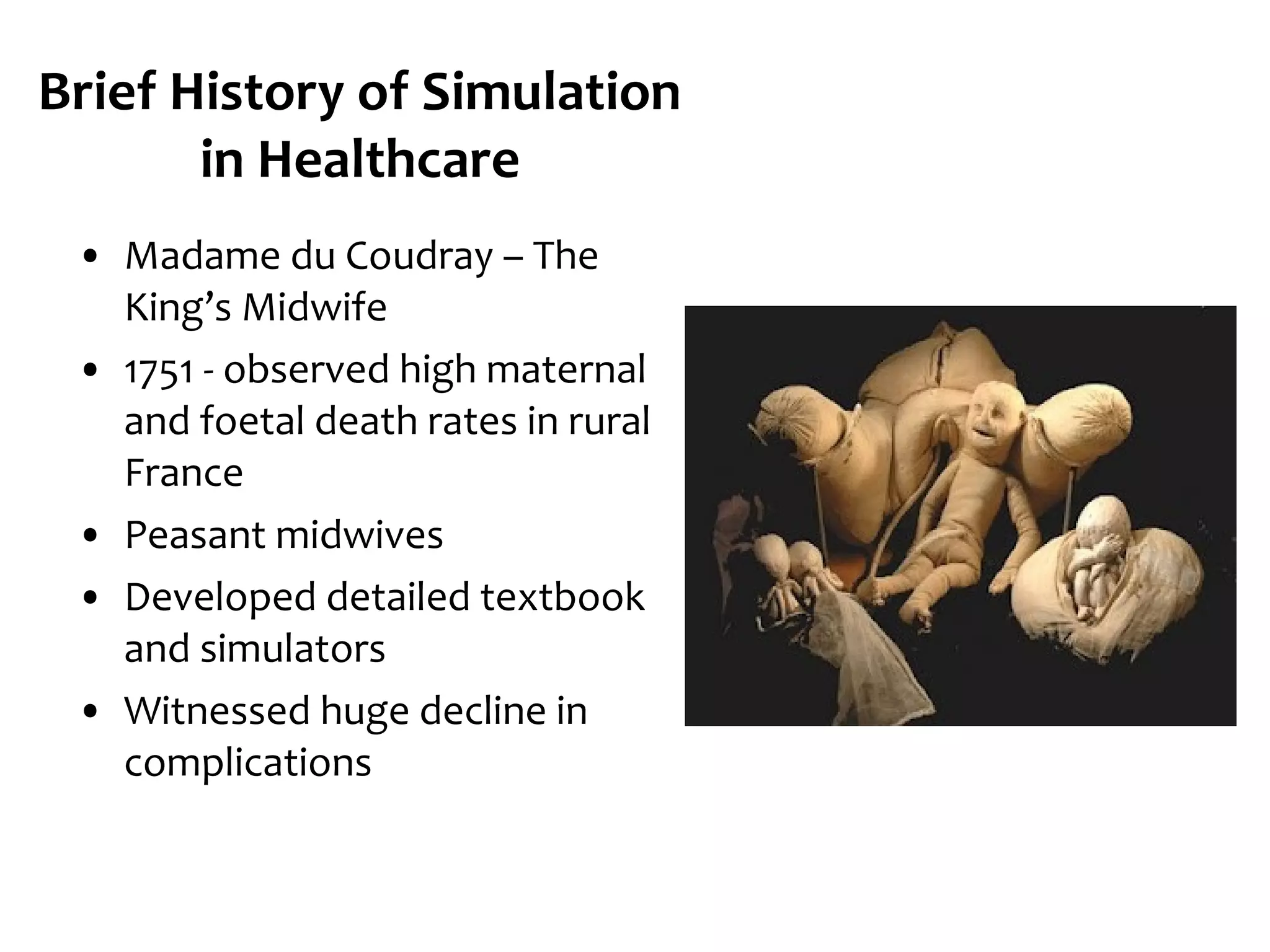
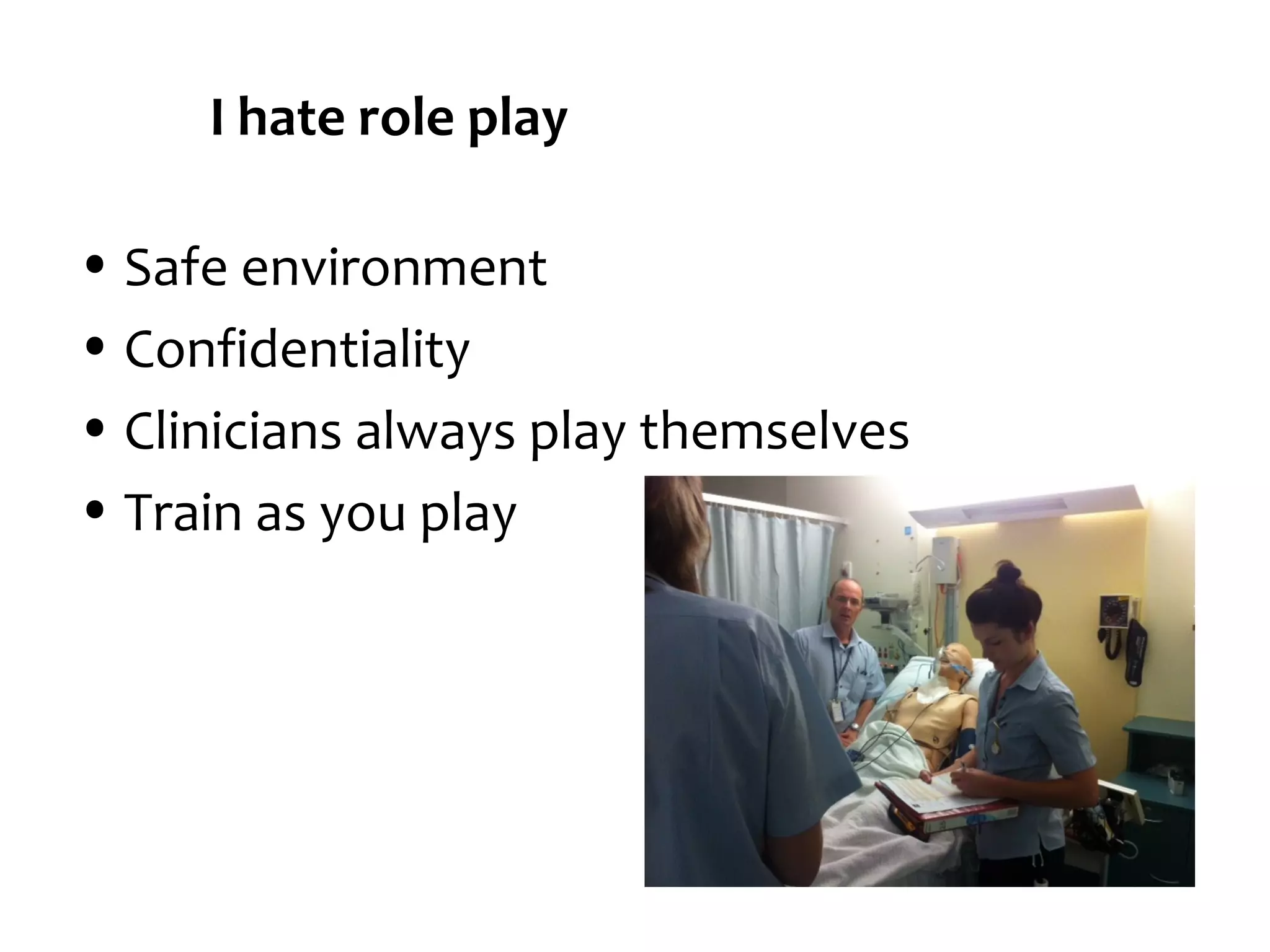
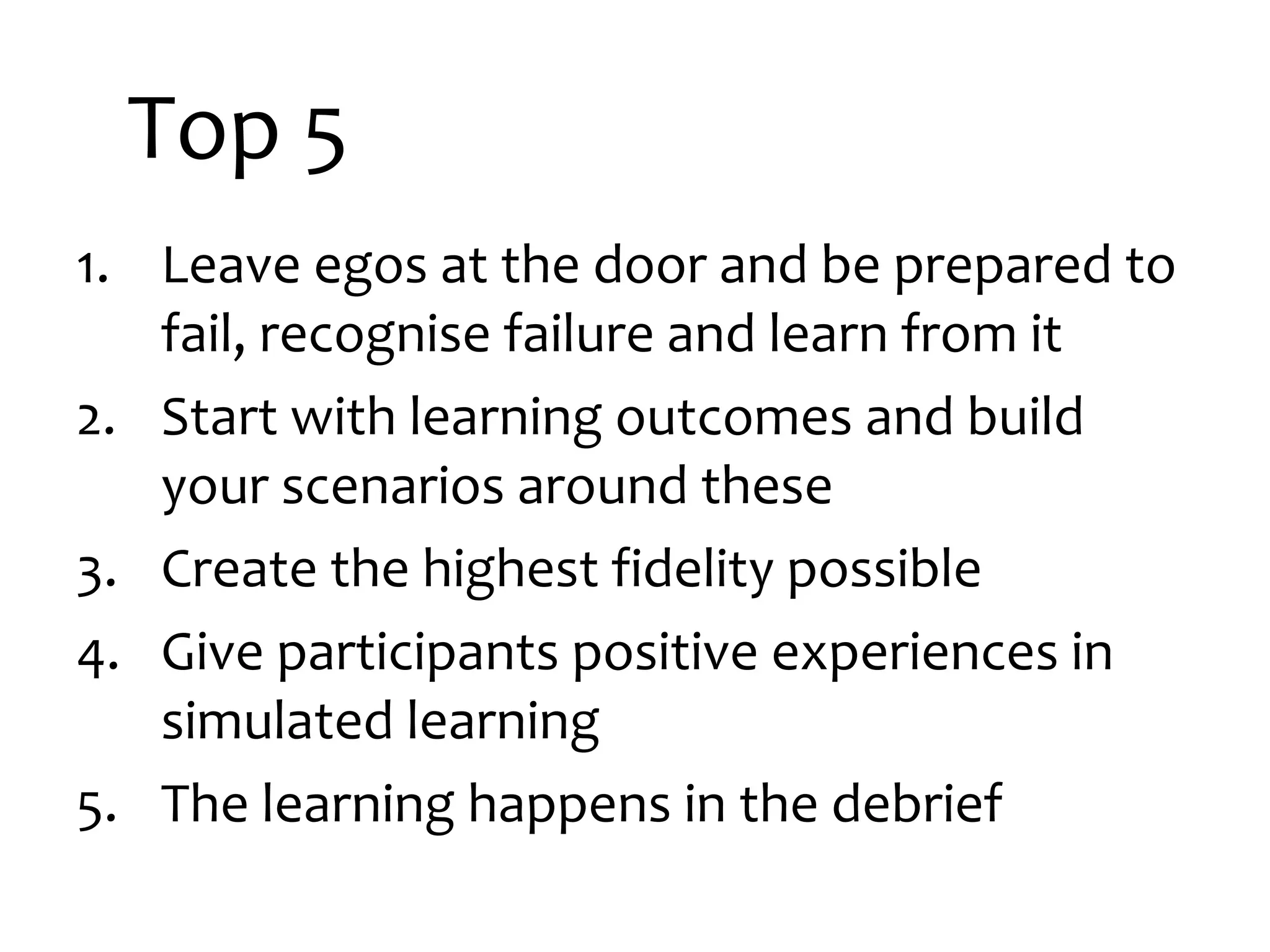
The document discusses the integration of simulation into healthcare education, detailing historical context, challenges faced, and strategies for improvement. It highlights issues such as participant resistance, management buy-in, and the need for realistic scenarios, while suggesting solutions like creating a supportive community and utilizing high-fidelity simulation techniques. Key takeaways emphasize the importance of learning outcomes, positive participant experiences, and effective debriefing for continuous improvement.