This presentation provides information about ventilators including:
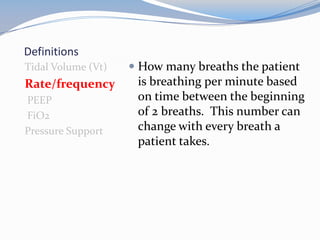
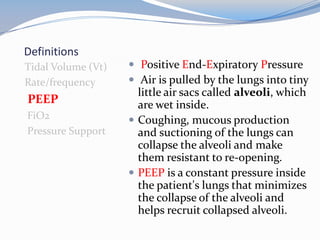
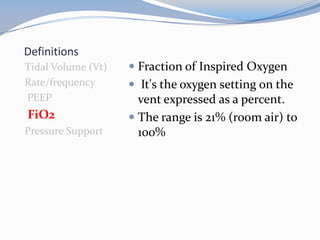
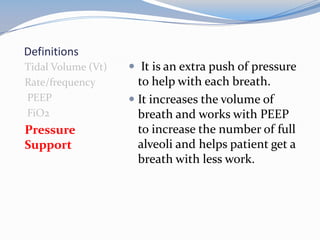
- Definitions of key terms like tidal volume, PEEP, and pressure support.
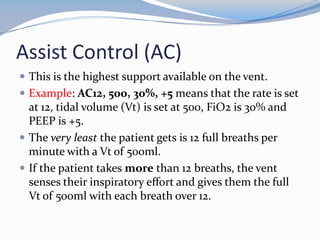
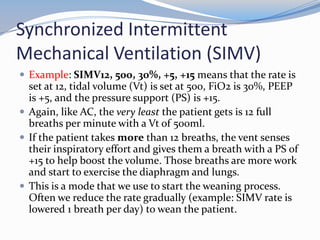
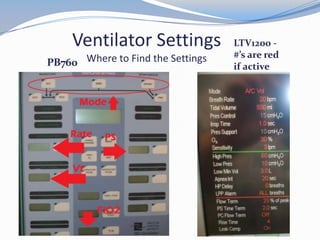
- The most common ventilator modes of Assist Control, SIMV, and Pressure Support and example settings.
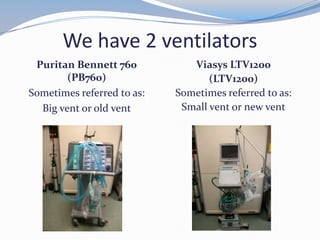
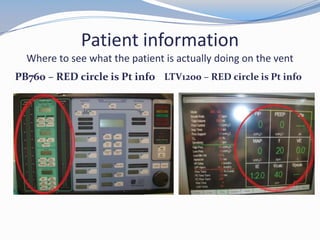
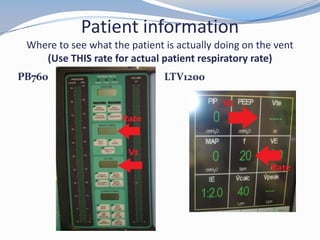
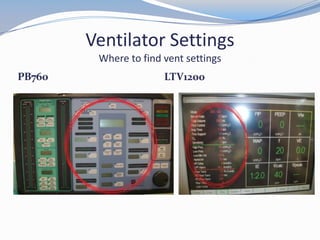
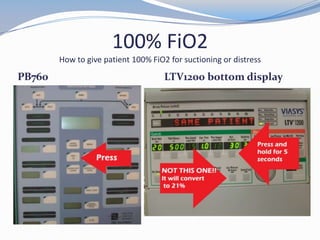
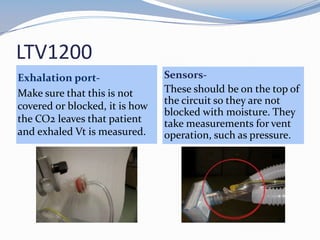
- Identifying patient data and settings on the two ventilators used - the Puritan Bennett 760 and Viasys LTV1200.
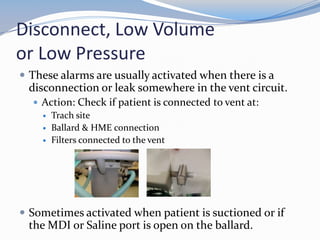
- Common ventilator alarms like high pressure and disconnect and appropriate troubleshooting actions.
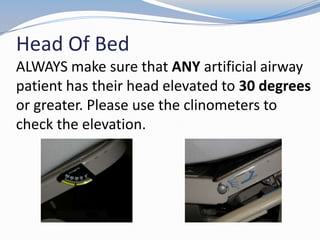
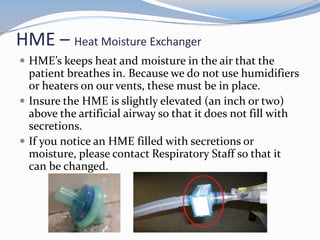
- Other important aspects like using a clinometer to check head of bed elevation and maintaining heat and moisture with an HME.