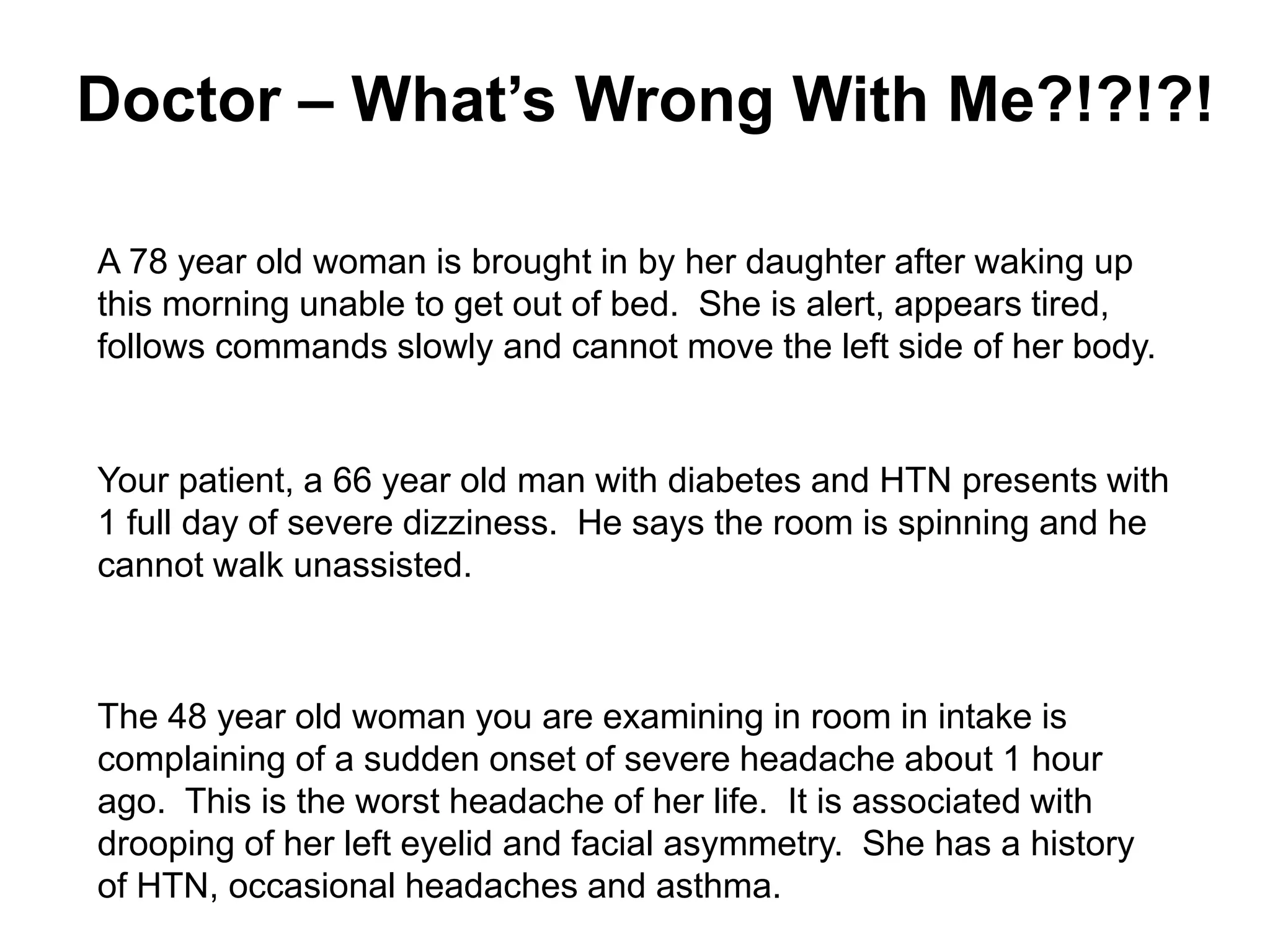
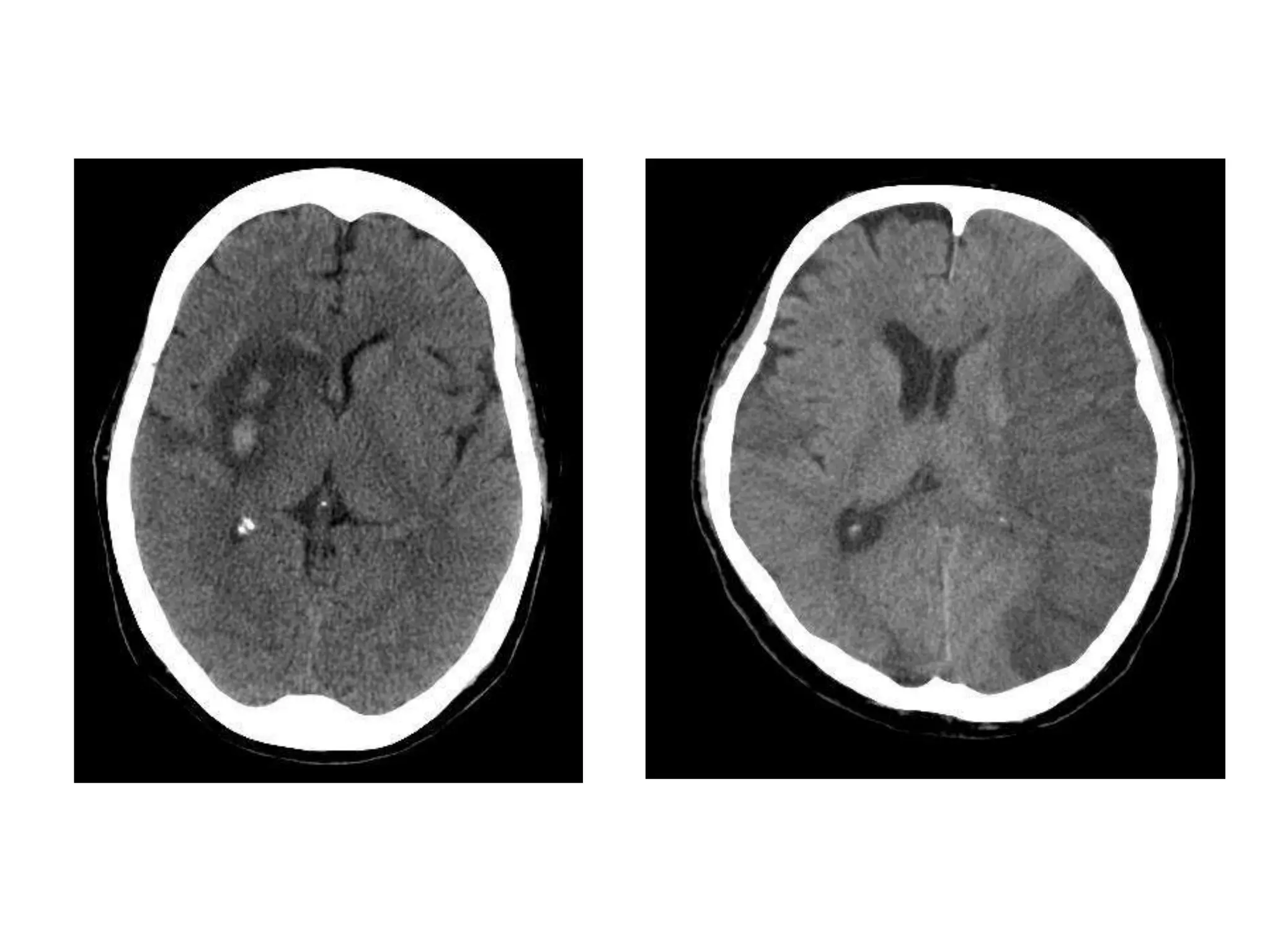
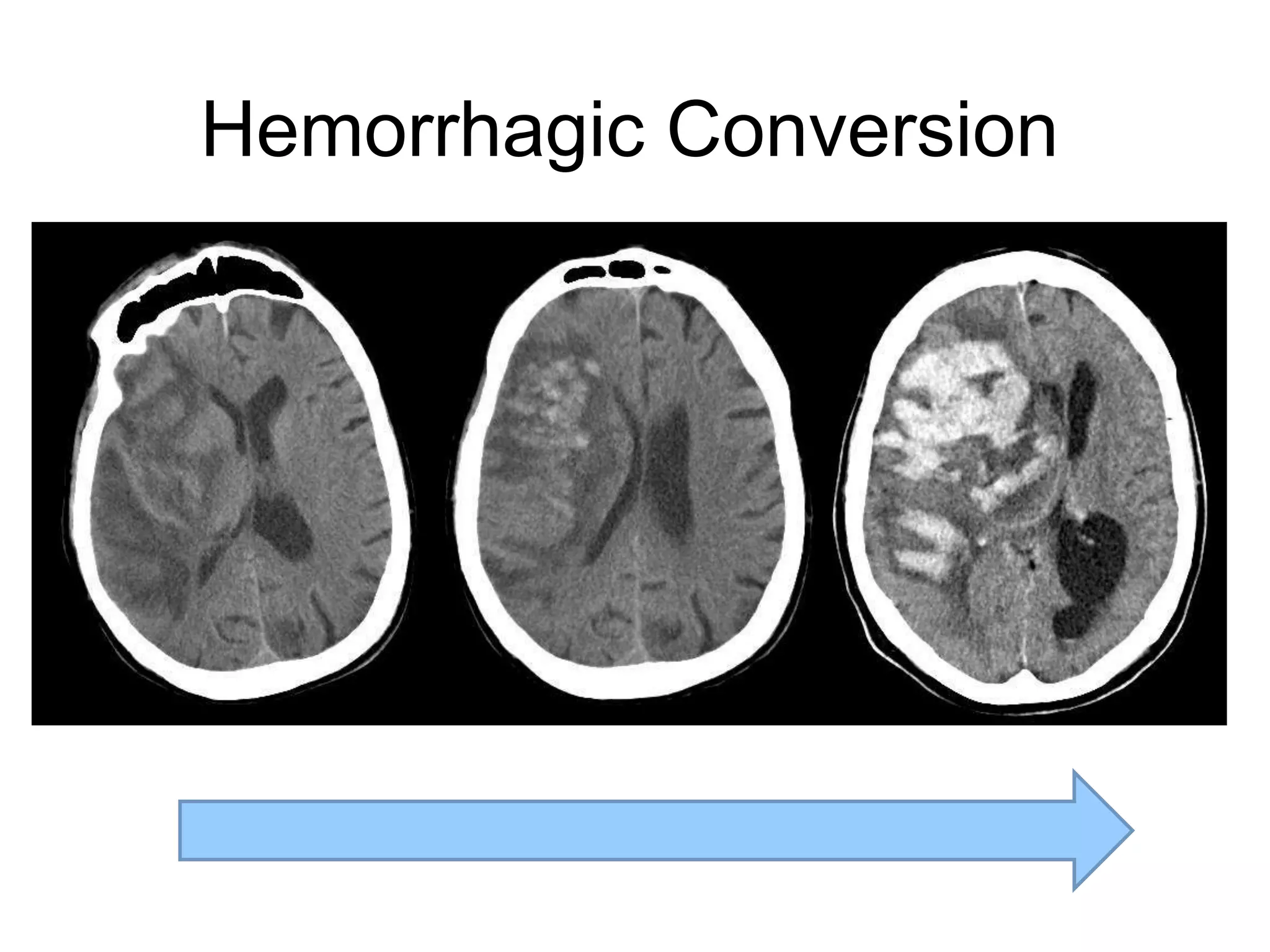
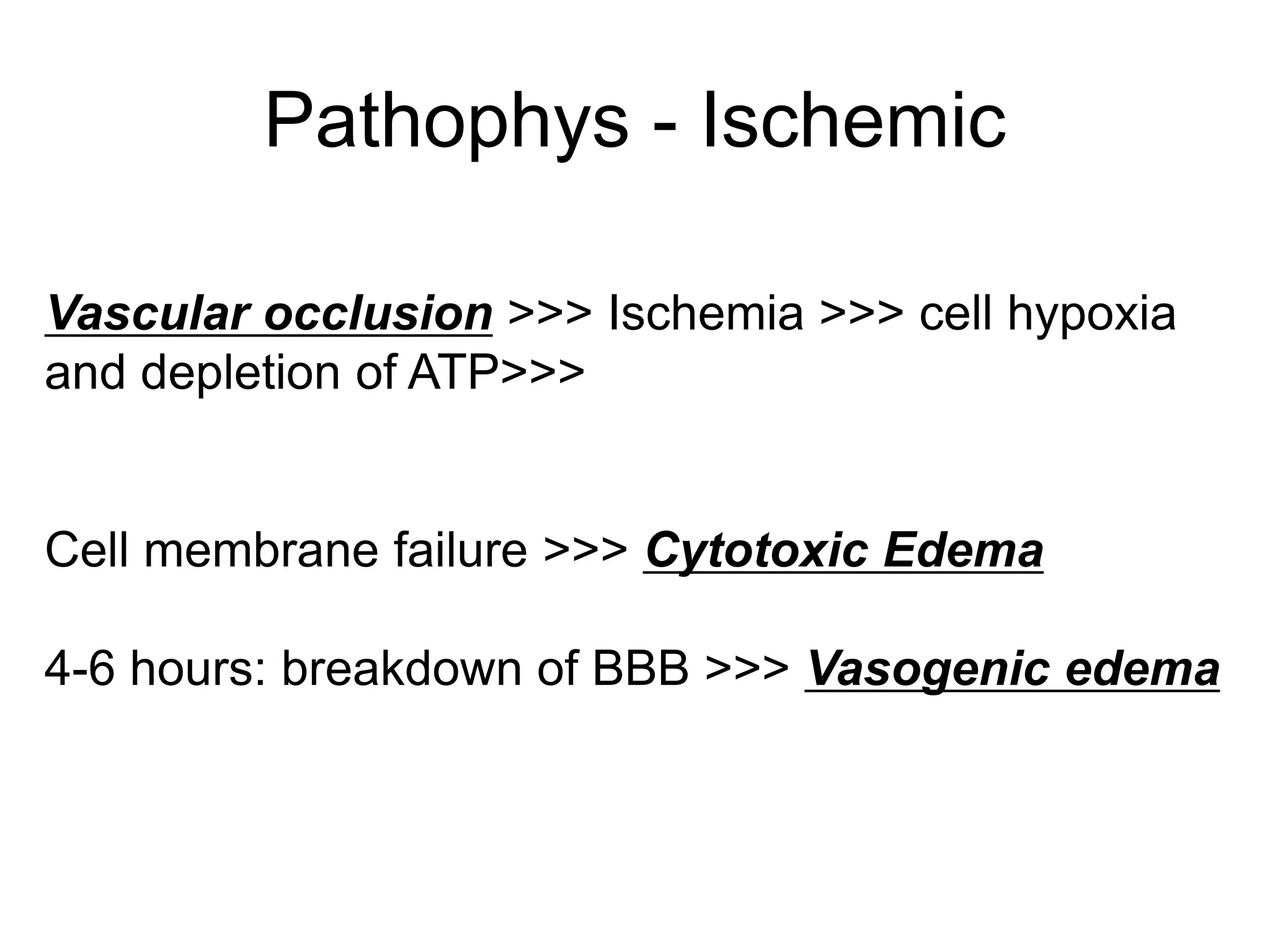
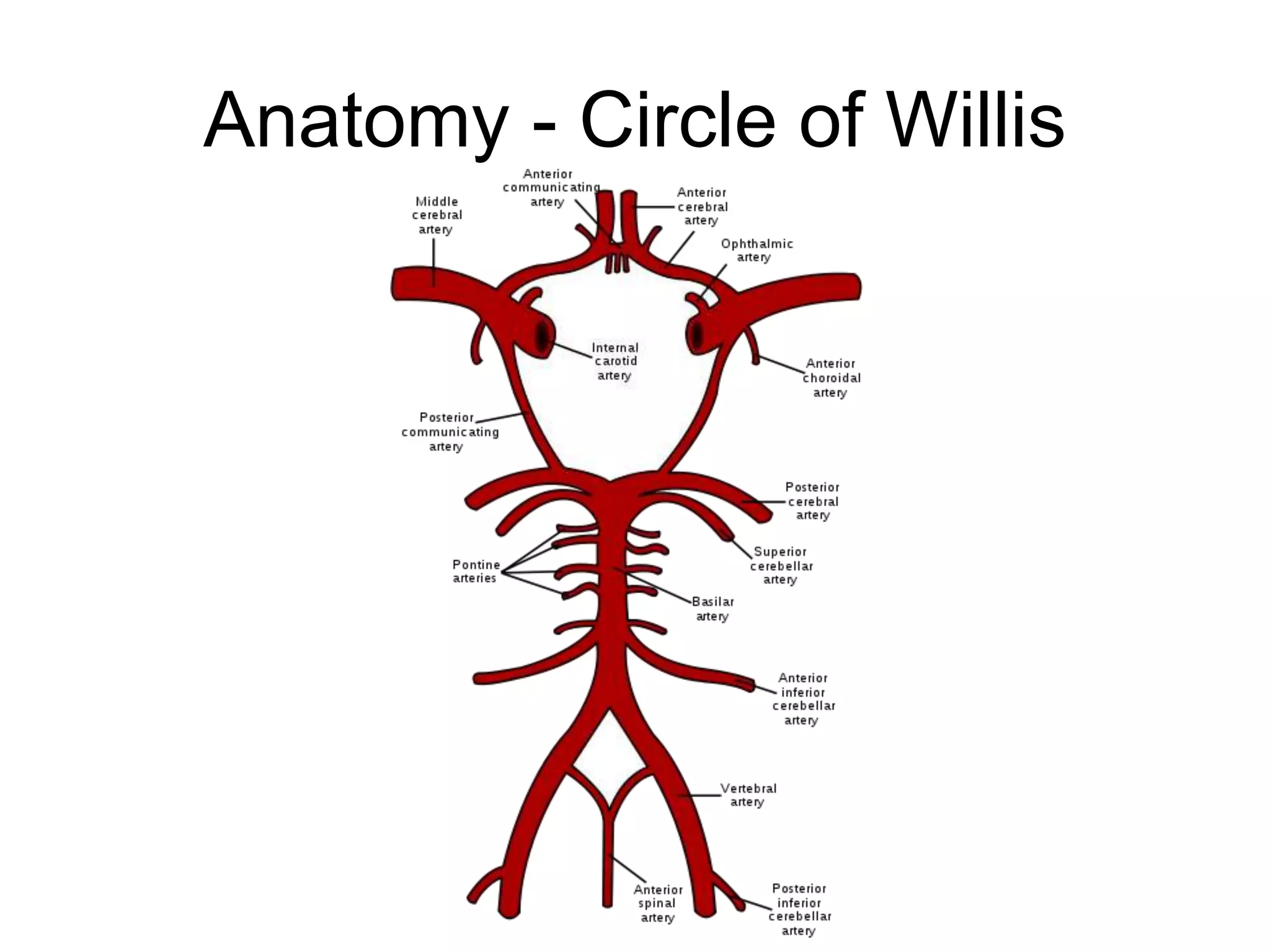
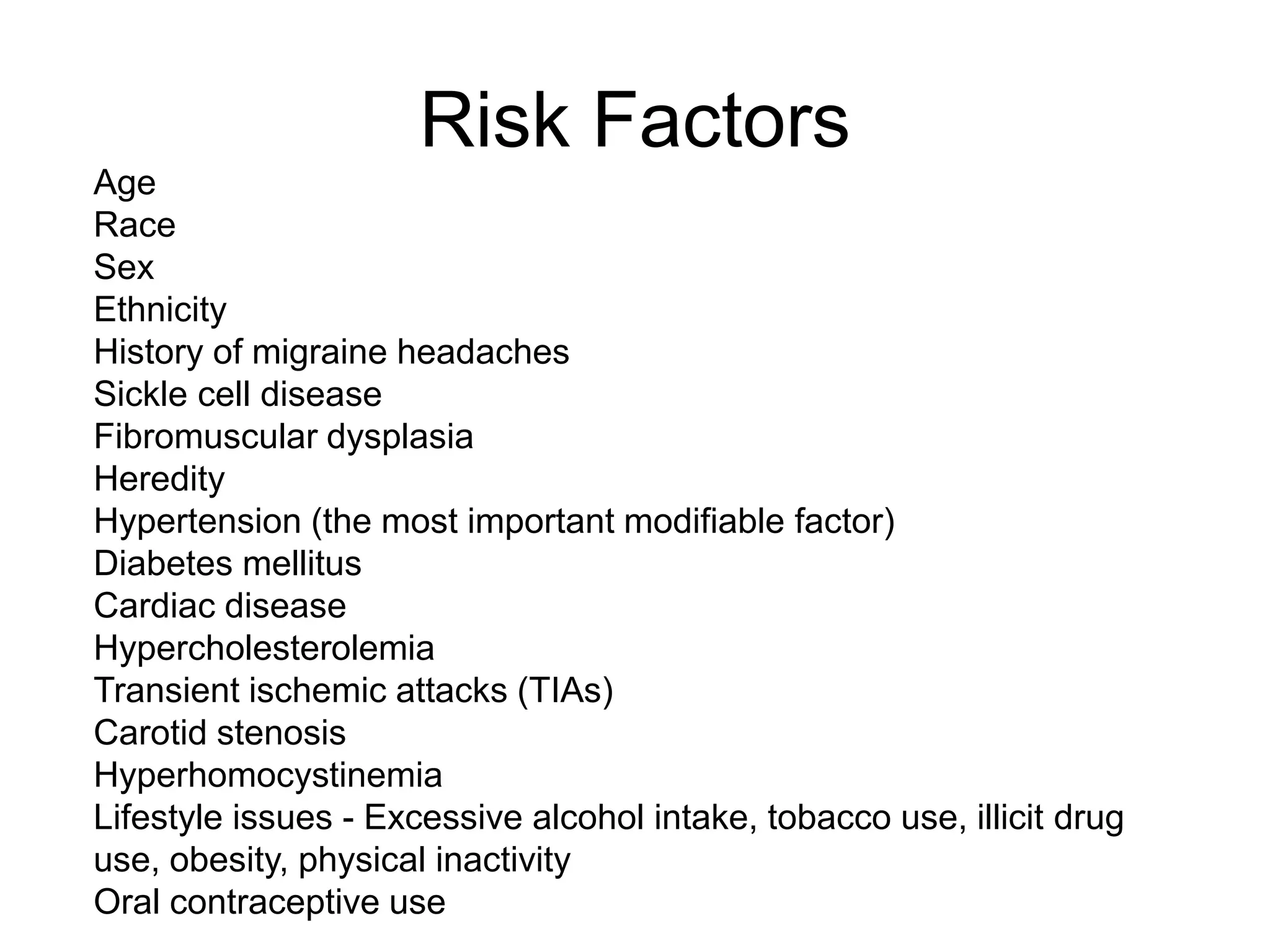
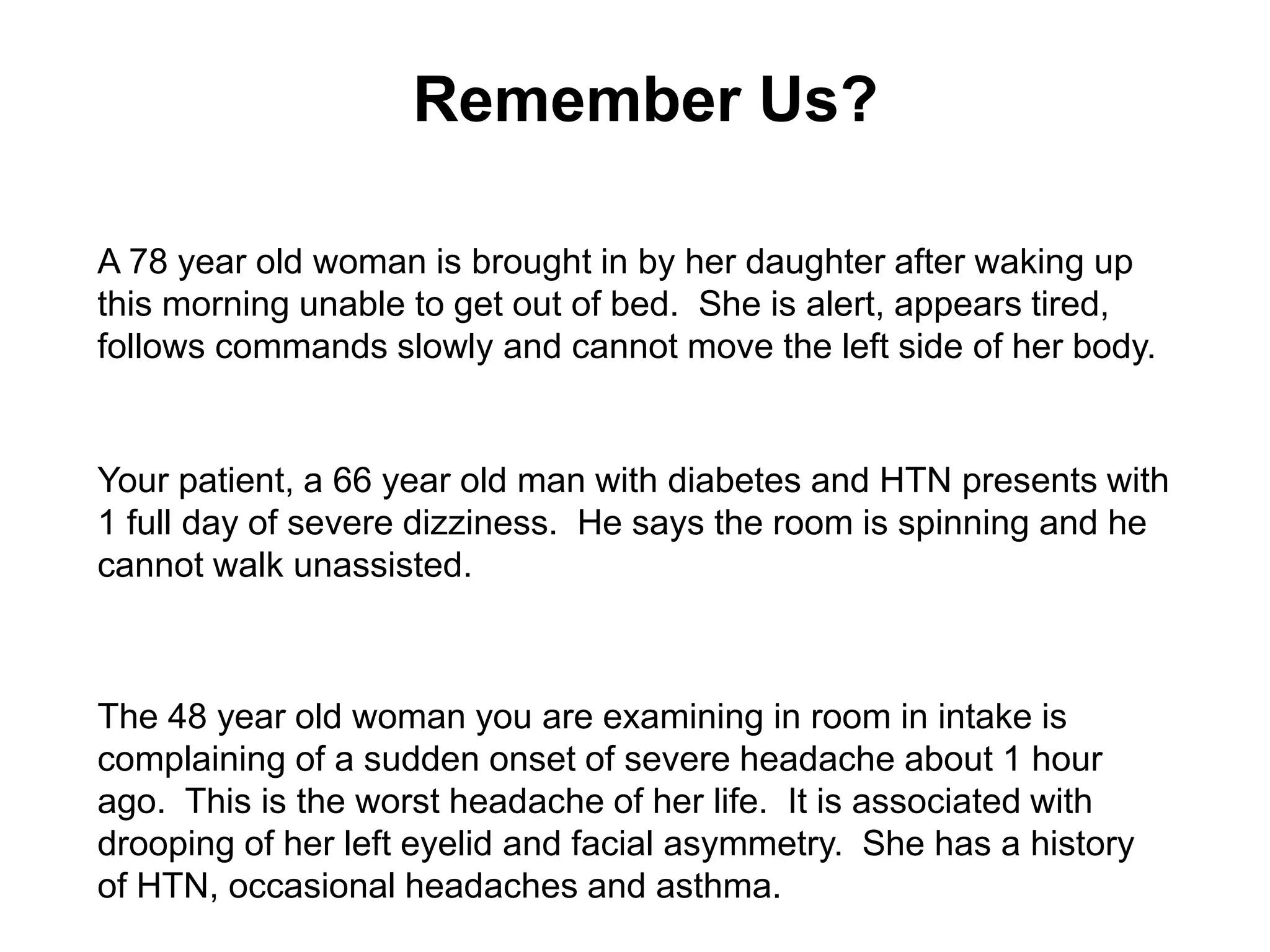
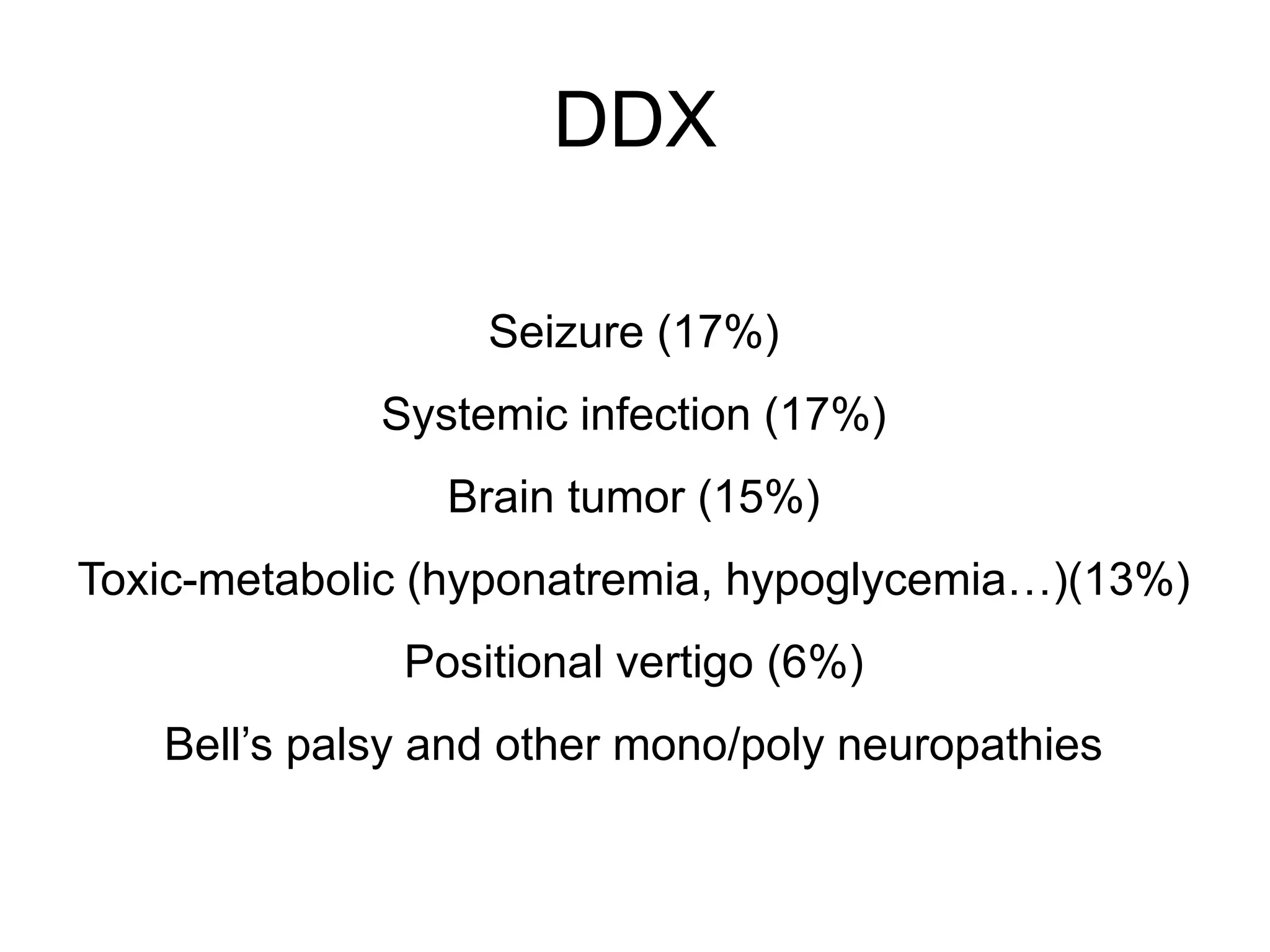
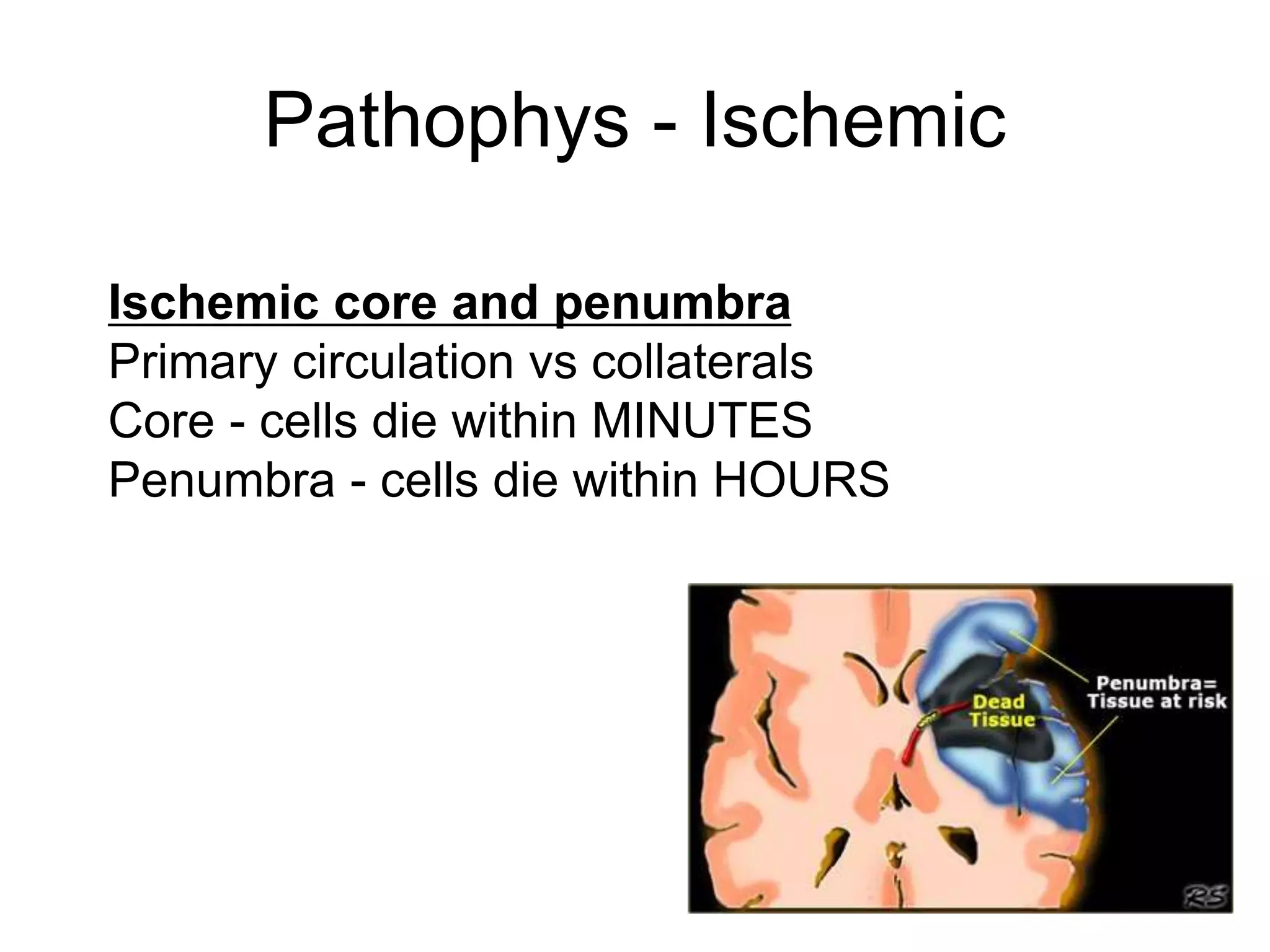
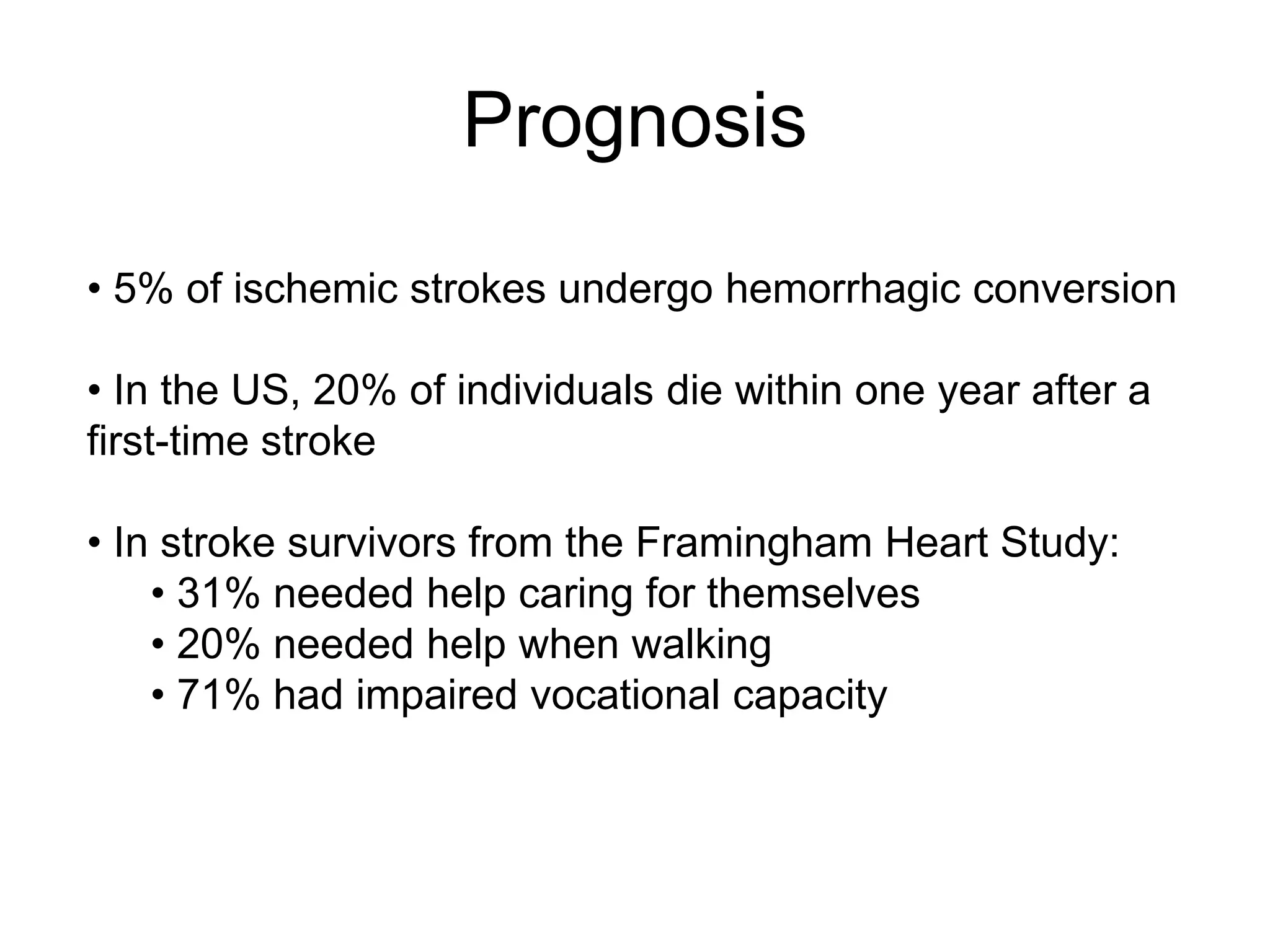
The document discusses stroke presentation, including case examples of patients and their symptoms, and outlines the epidemiology, pathophysiology, risk factors, evaluation, and management of strokes. It highlights key differentiating conditions and includes information on the use of IV-tPA for ischemic stroke, its indications, contraindications, and dosing protocol. The document also emphasizes the importance of neurologic exams and scoring systems in assessing stroke patients.