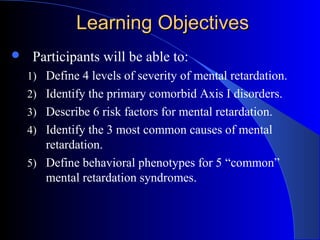
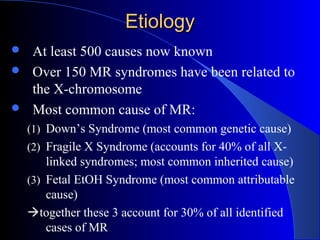
This document provides information on intellectual disability (ID), including definitions, levels of severity, comorbid disorders, risk factors, causes, and treatment with psychotropic medications. Key points include:
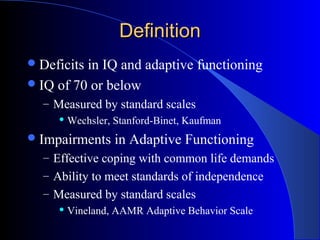
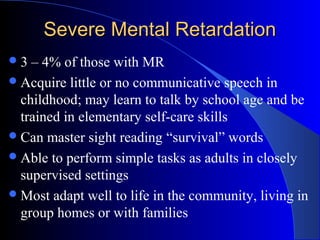
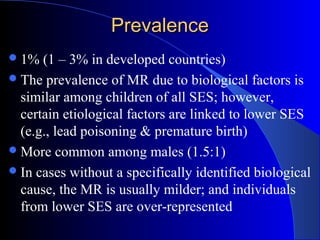
- ID is defined by deficits in both IQ (70 or below) and adaptive functioning. It ranges from mild to profound depending on IQ scores.
- The most common causes are Down syndrome, Fragile X syndrome, and fetal alcohol syndrome, together accounting for 30% of cases.
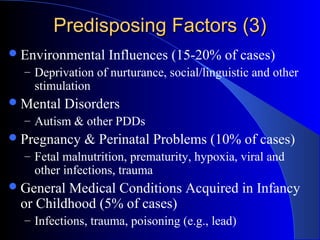
- Risk factors include heredity, early embryonic alterations, environmental influences, and pregnancy/birth complications.
- Common comorbid disorders are ADHD, mood disorders, and autism spectrum disorders. Stimulants and


















![Fetal EtOH SyndromeFetal EtOH Syndrome
Incidence > 1:1000
Irritable as infants, hyperactive as children (ADHD)
Teratogen amount: 2 drinks/day (smaller birth size), 4-6
drinks/day (subtle clinical features), 8-10 drinks/day (full
syndrome)
General problems: prenatal onset of growth deficiency,
microcephaly, short palpebral fissures
Syndrome can include:
– Facial deformities (ptosis of eyelid, microphthalmia, cleft lip [+/- palate],
micrognathia, flattened nasal bridge and filtrum, & protruding ears)
– CNS deformities (meningomyelocele, hydrocephalus)
– Neck deformities (mild webbing, cervical vertebral & rib abmormalities)
– Cardiac deformities (tetralogy of Fallot, coarctation of aorta)
– Other abnormalities (hypoplastic labia majora, strawberry hemangiomata)](https://image.slidesharecdn.com/intellectualdisability-150415051941-conversion-gate01/85/Intellectual-disability-25-320.jpg)