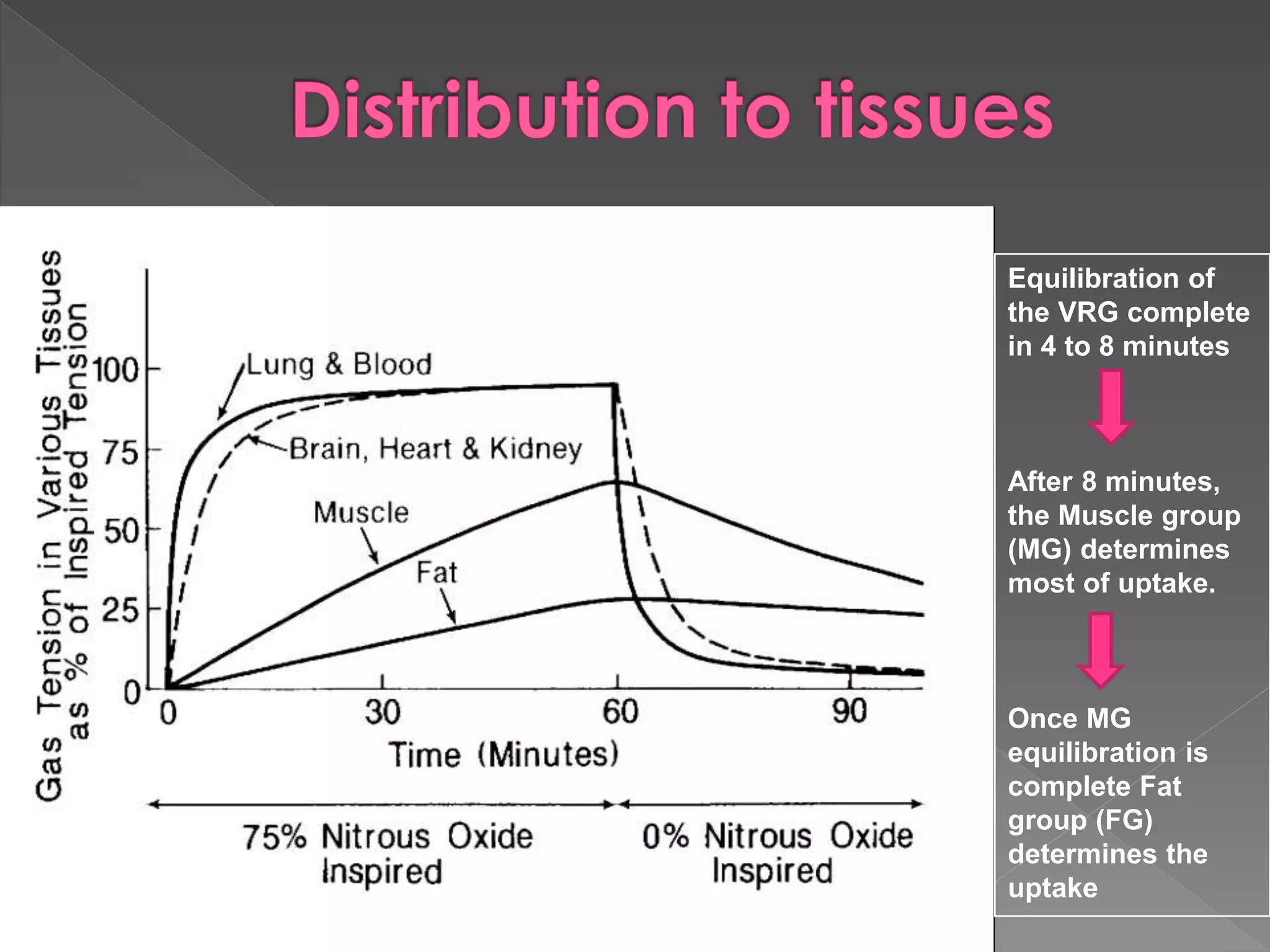
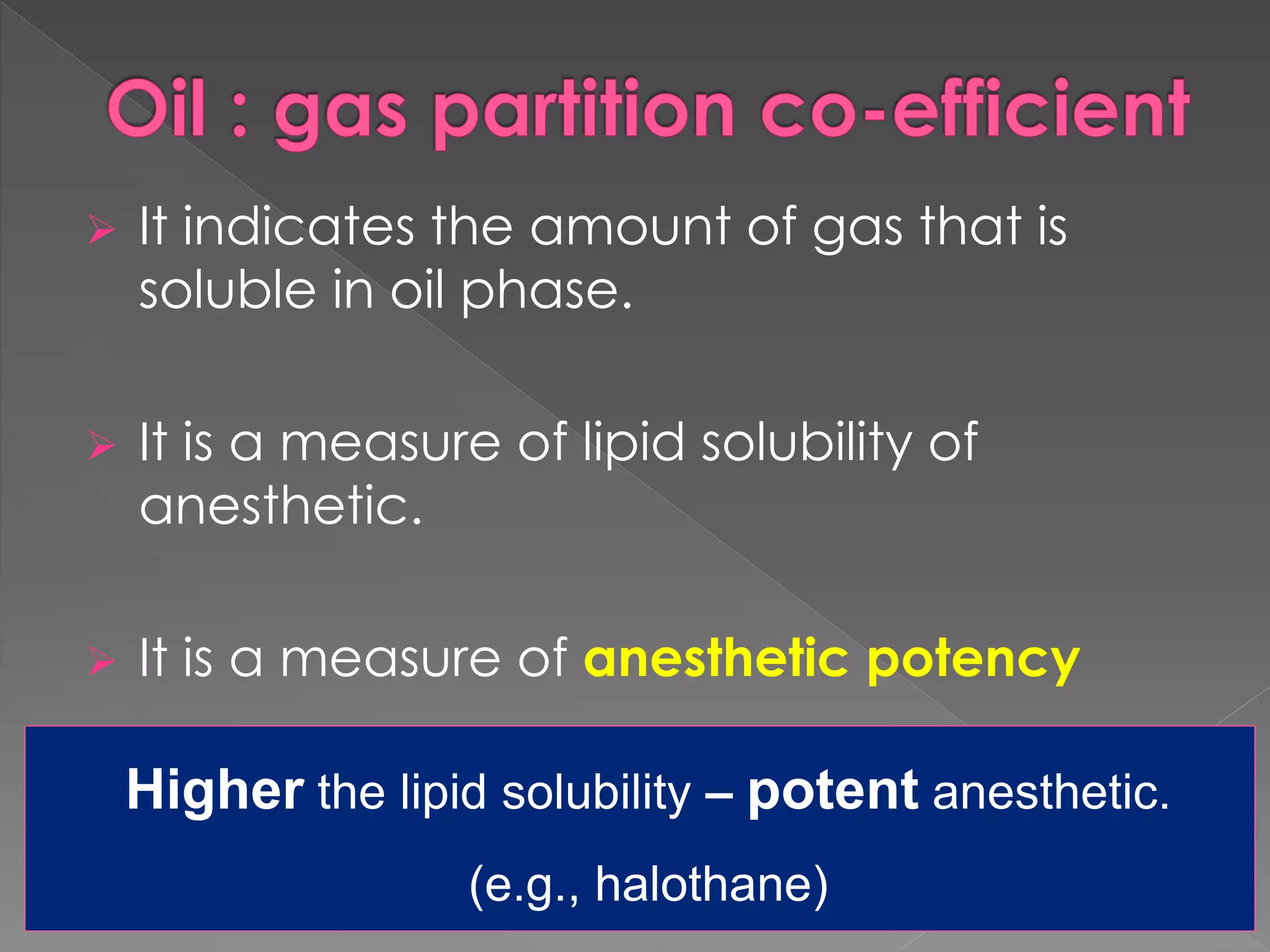
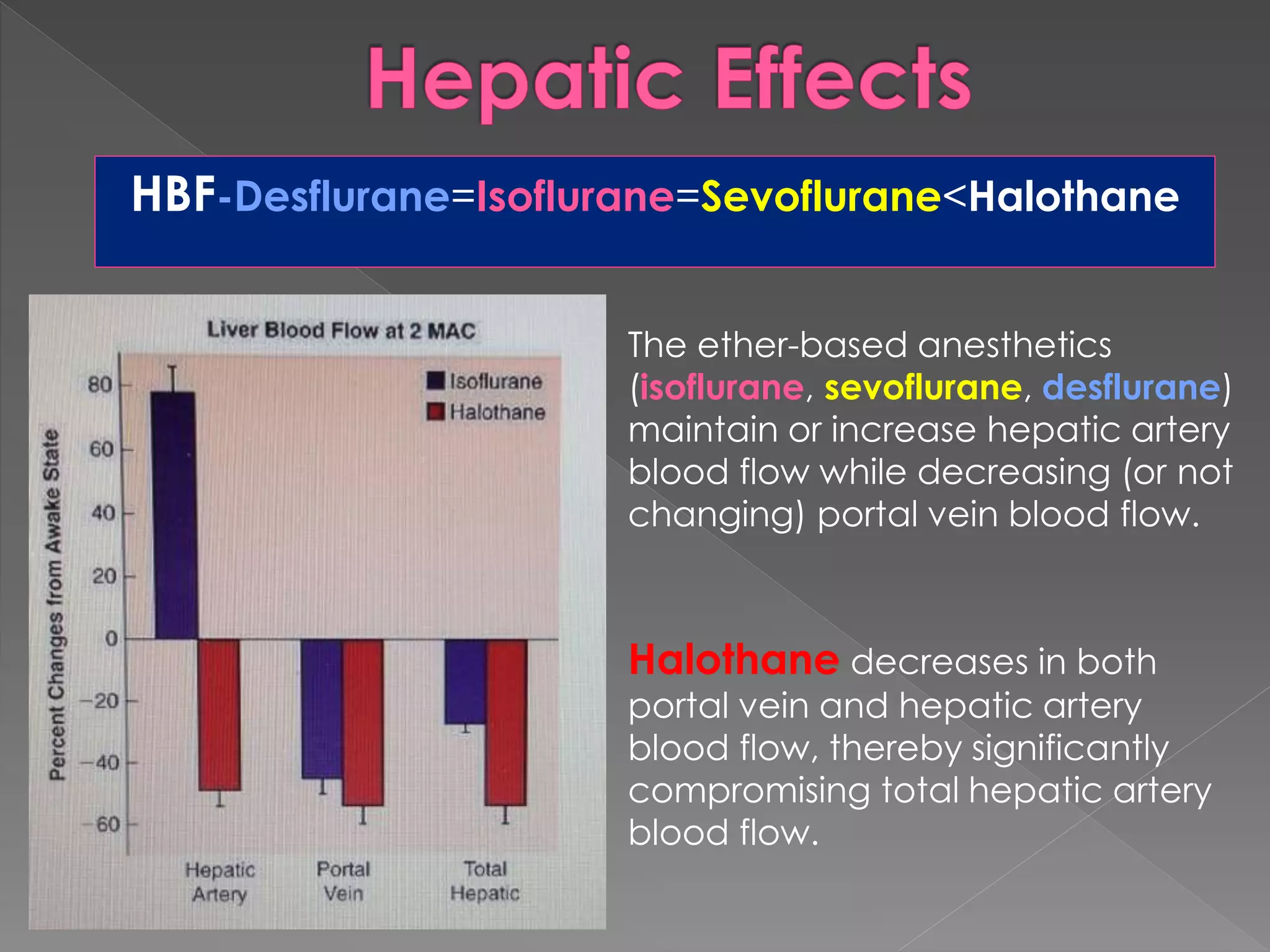
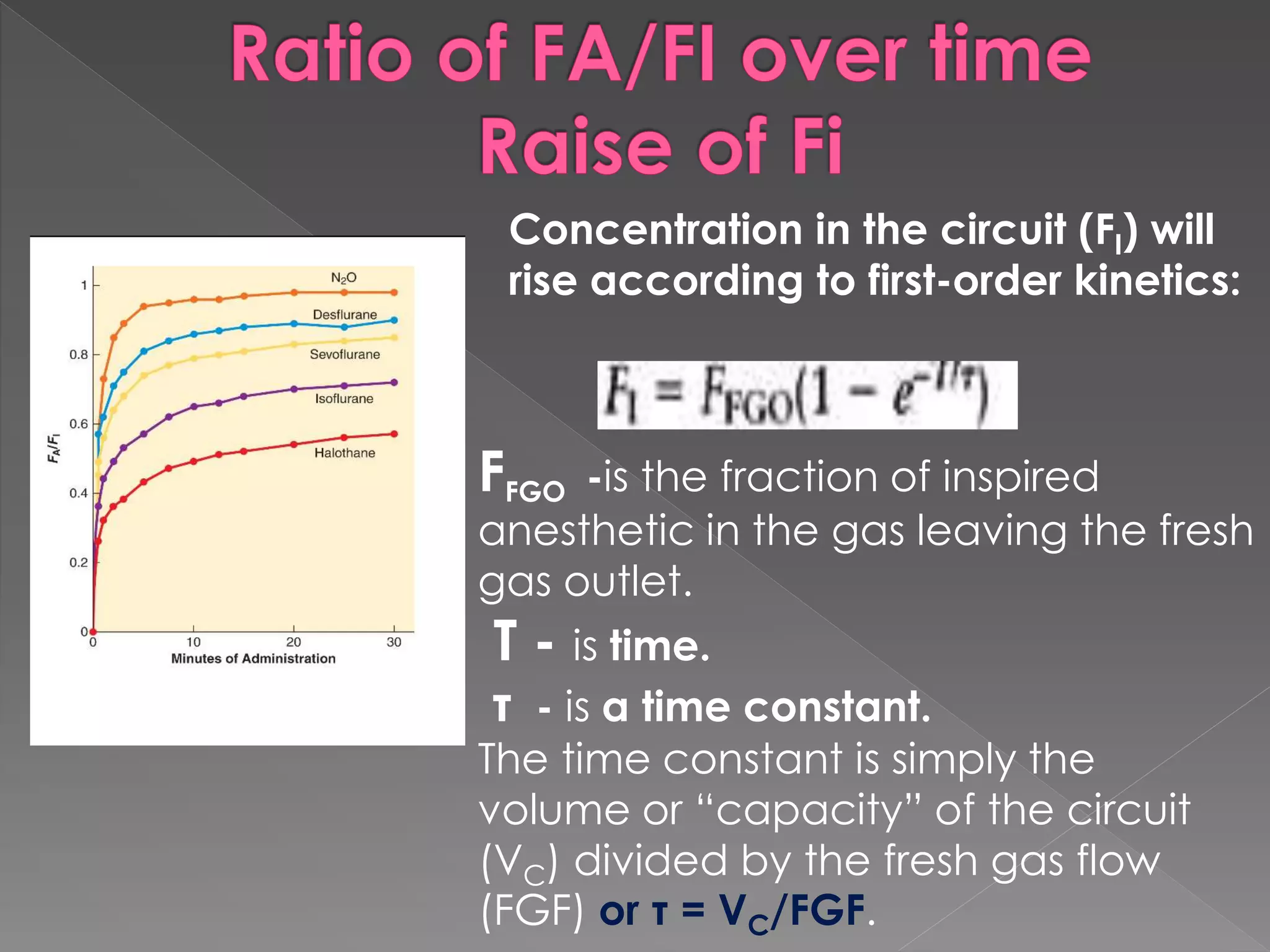
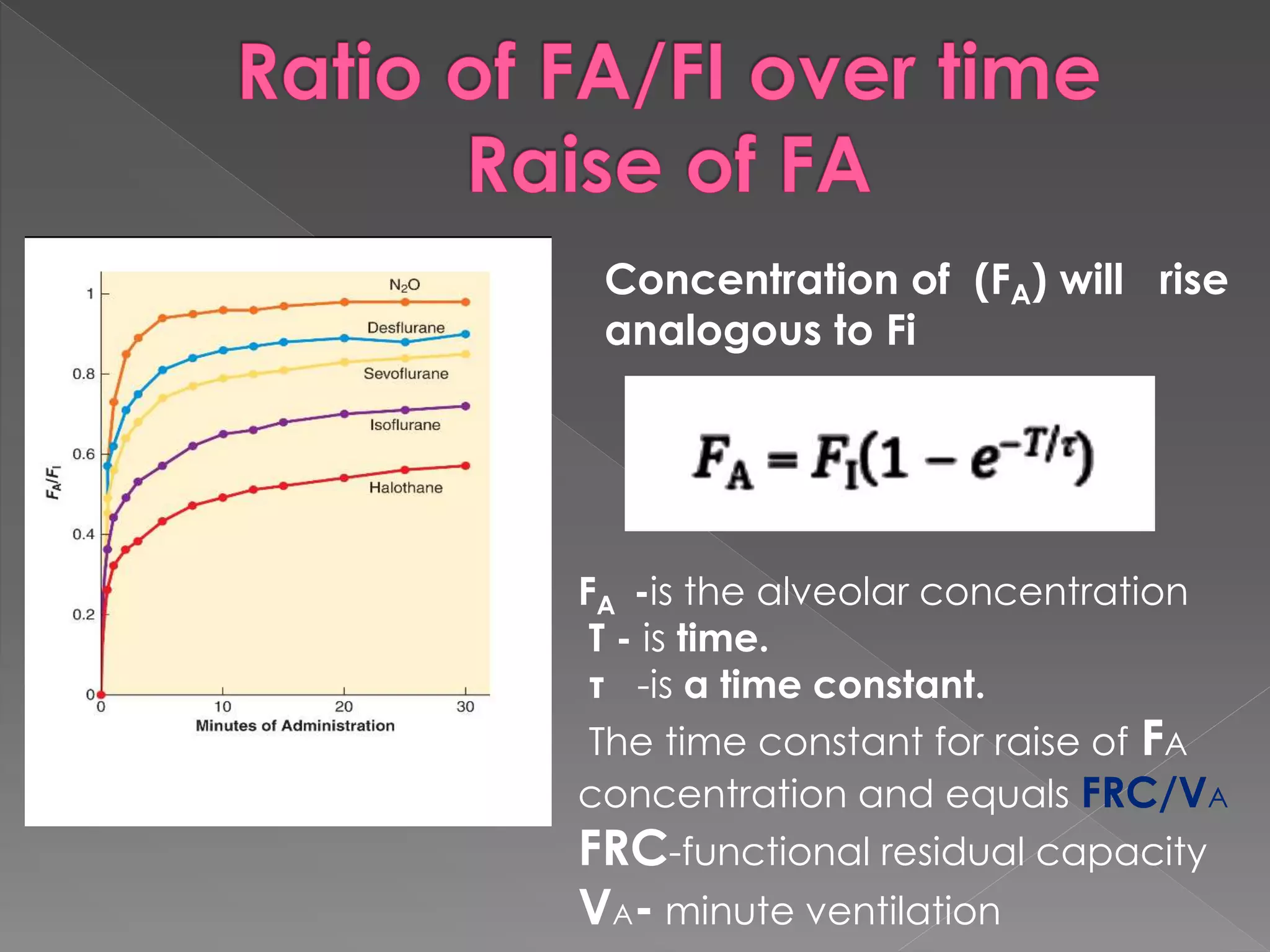
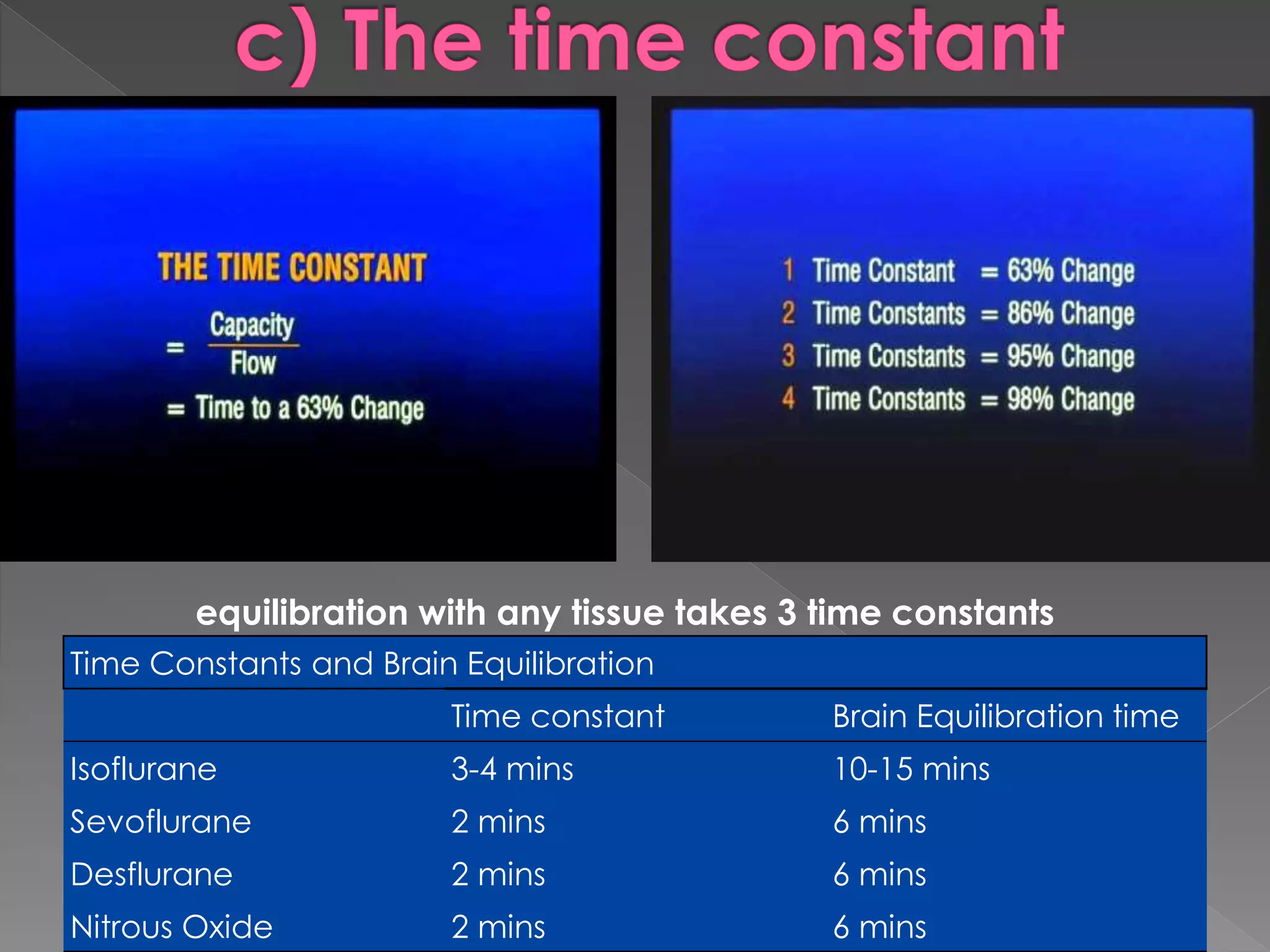
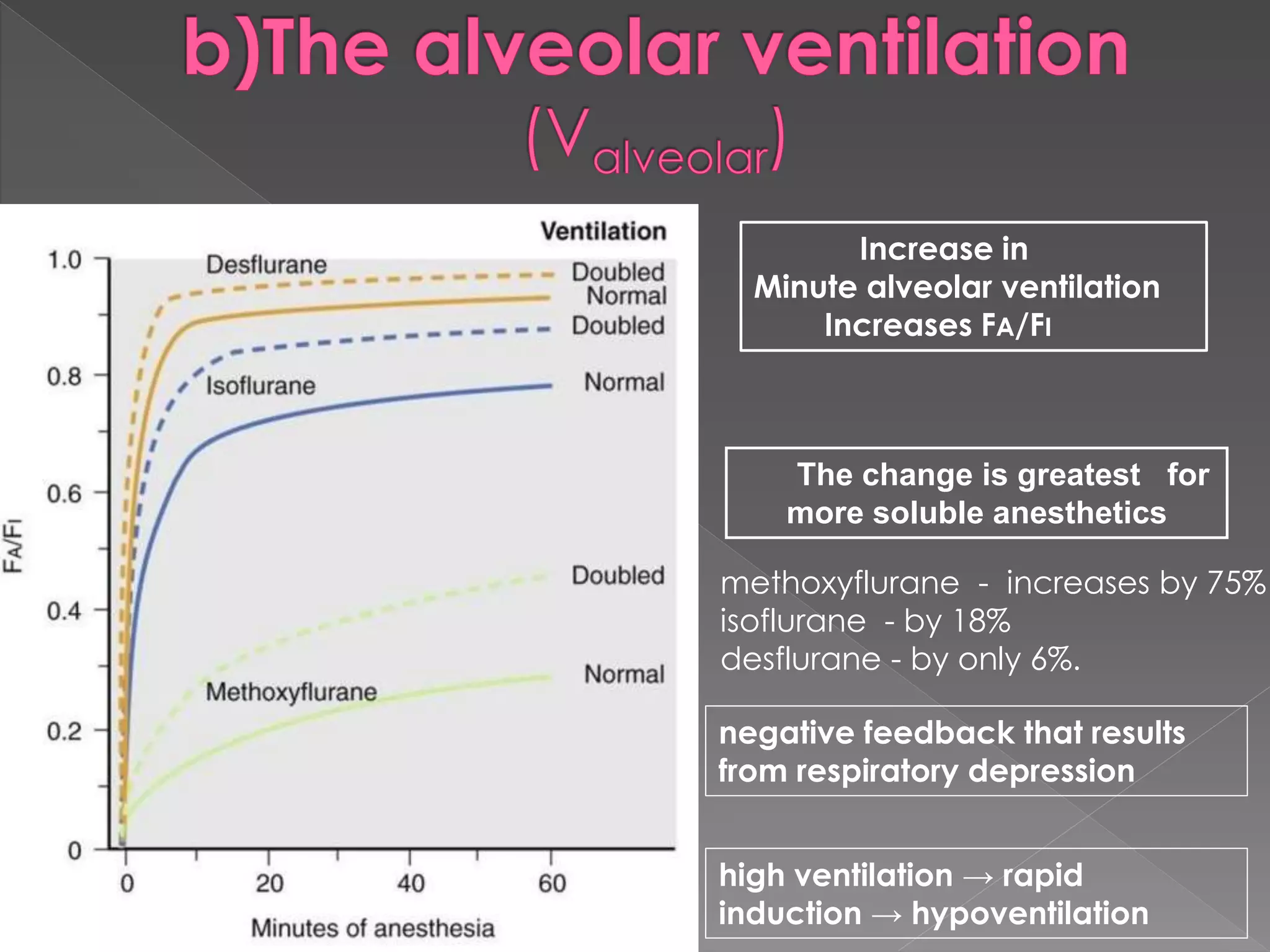
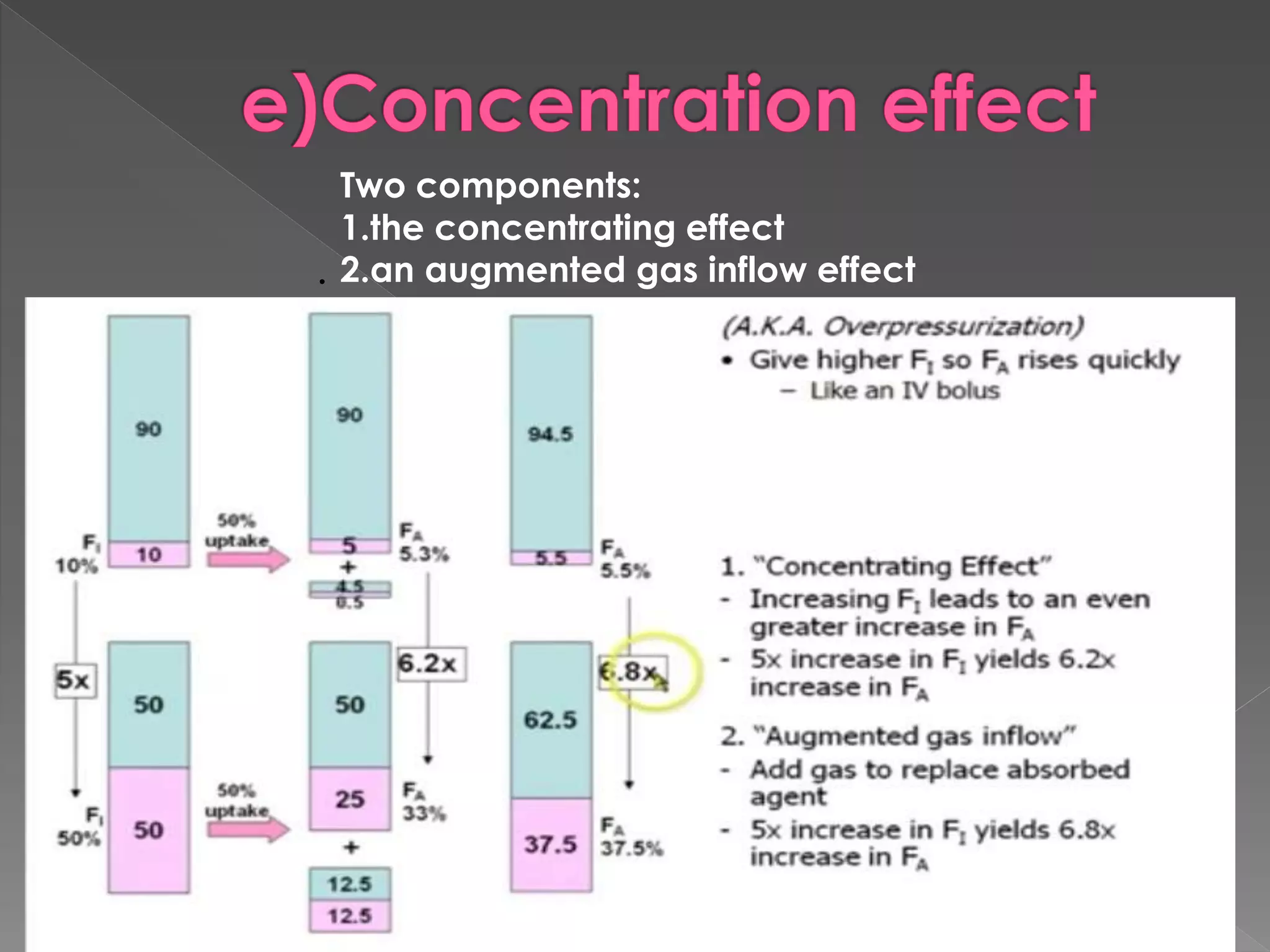
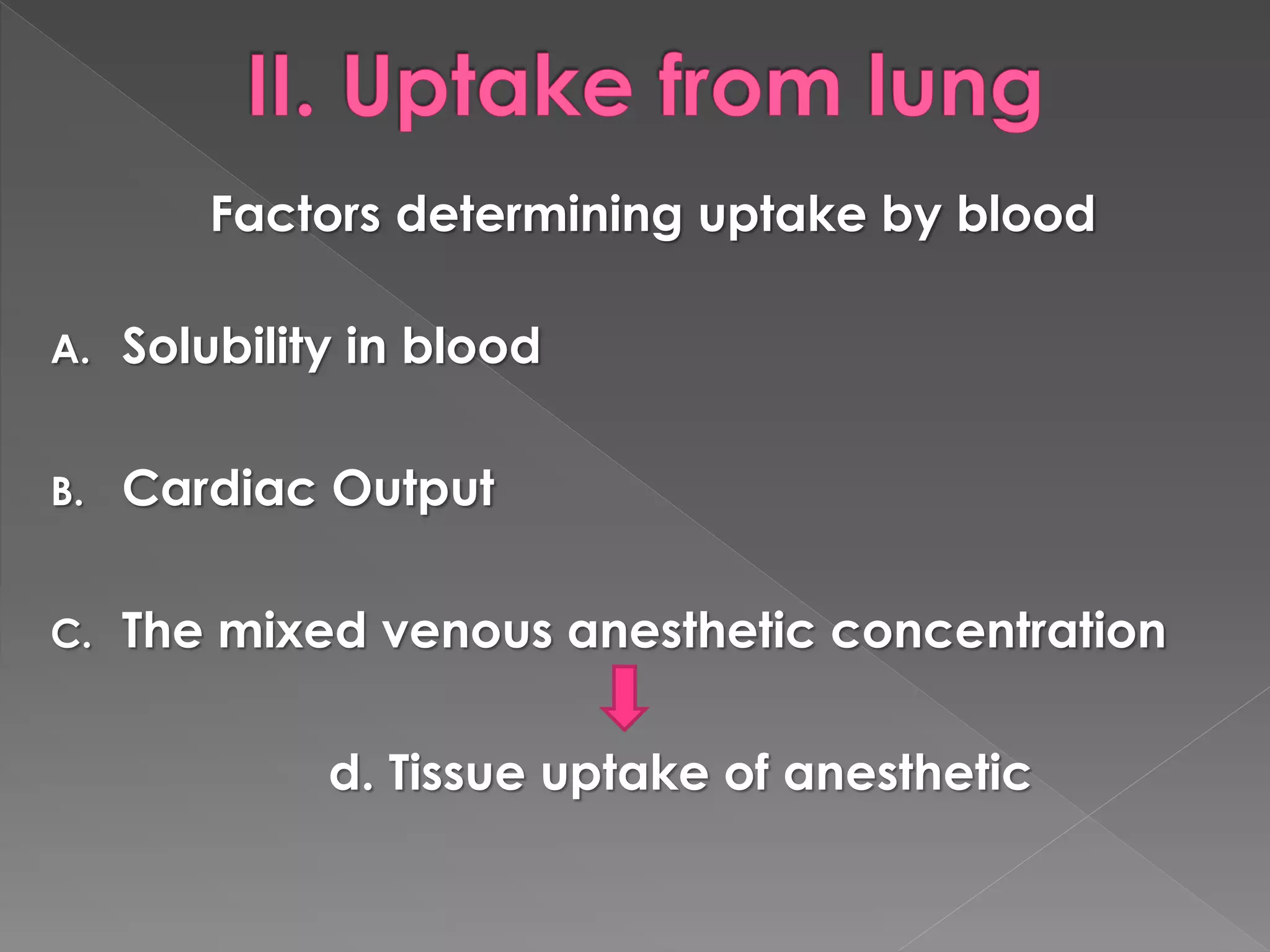
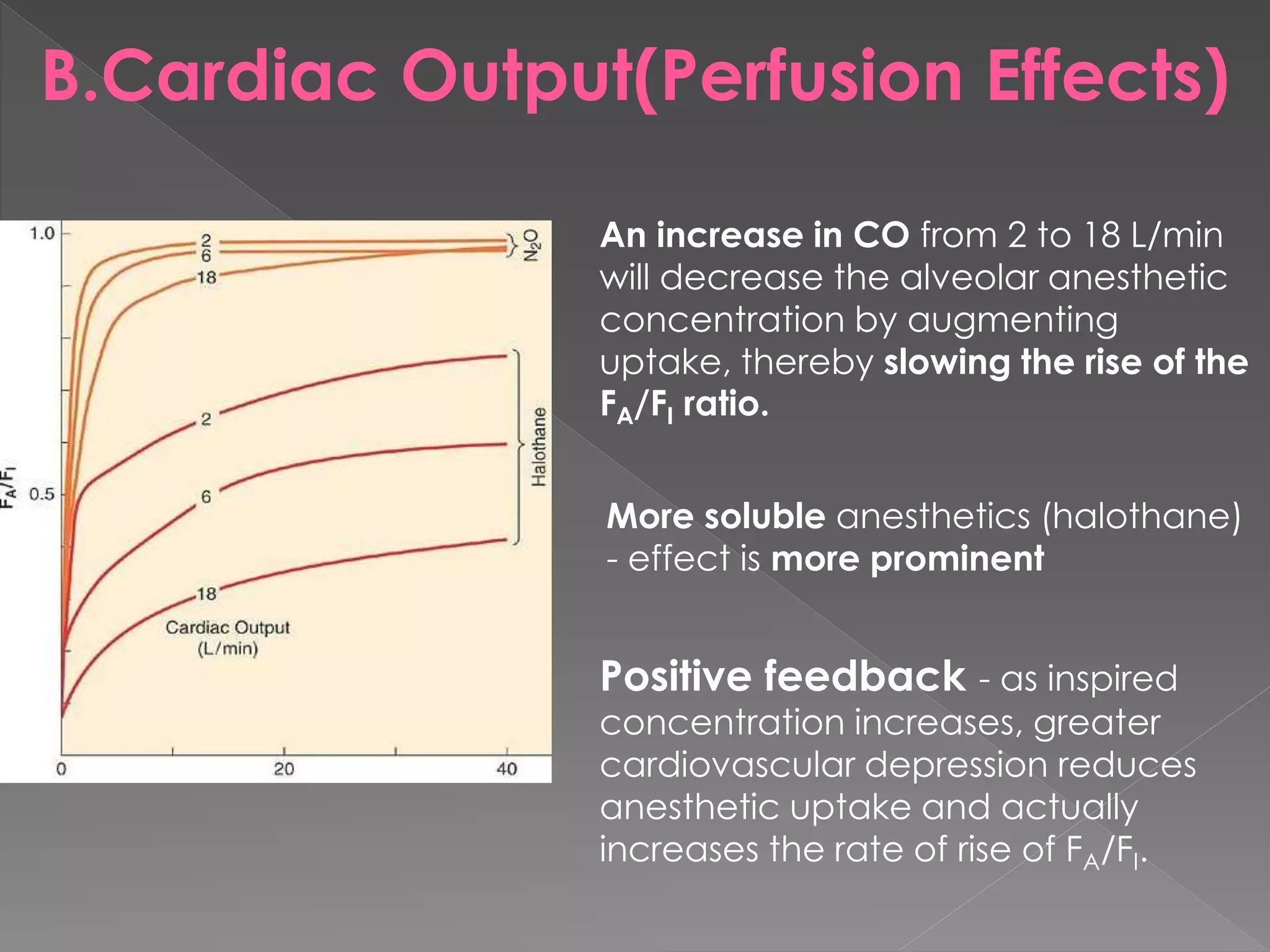
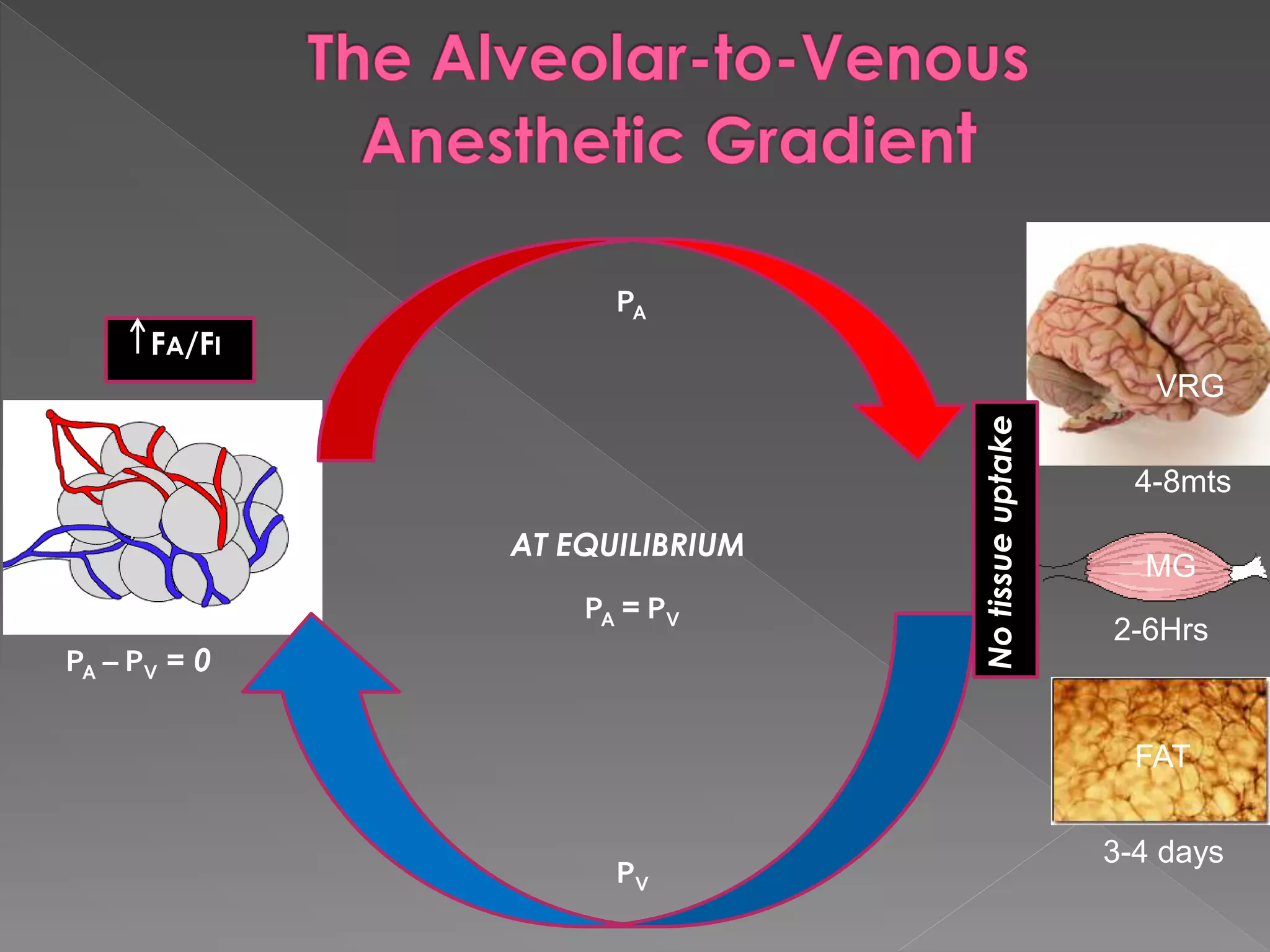
This document discusses the history of anesthesia and how inhalational anesthetics work. It notes that Joseph Priestly discovered nitrous oxide in 1773. Crawford Long performed the first surgery using ether anesthesia in 1842 but did not publicize it. Morton's public demonstration of ether anesthesia in 1846 is considered the official beginning of surgical anesthesia. The document also summarizes that the mechanism of how inhalational anesthetics work is still not fully understood, but they likely act through interactions with lipid membranes and various receptor sites in the brain. Key factors such as solubility, cardiac output, ventilation, and circuit volume influence how quickly anesthetic gases equilibrate between the lungs and brain.




![ Vaporizer
Breathing Circuit
Alveoli (lungs)
Arterial Blood
Tissues (VRG [brain], MUS,FAT)
Venous blood (coming back to lungs)
Alveoli (lungs, again)
Breathing Circuit (to be rebreathed)](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-8-2048.jpg)
![Time constant
Uptake and distribution of anesthetic
gases
FI
FA
FD
MAC
Brain Partial pressure
drives depth of
anesthesia
Equilibrates
Ventilation
λB/G
CO
PA - PV
λT/B
Tissue blood flow
[Parterial - PTissue]
1
2
FA/FI
Concentration and
second gas effects
Time constant
VRG](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-9-2048.jpg)









![Increase FA/FI Decrease FA/FI
Comment
Low blood solubility High blood solubility
As the blood solubility
decreases, the rate of rise in
FA/FI increases.
Low cardiac output High cardiac output
The lower the cardiac
output, the faster the rate of
rise in FA/FI
High minute ventilation Low minute ventilation
The higher the minute
ventilation, the faster the
rate of rise in FA/FI
Factors that Increase or Decrease the Rate of Rise of F /F
Uptake from the lung = Blood solubility x Cardiac Output x [PA-PV]
Bar. pressure](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-27-2048.jpg)




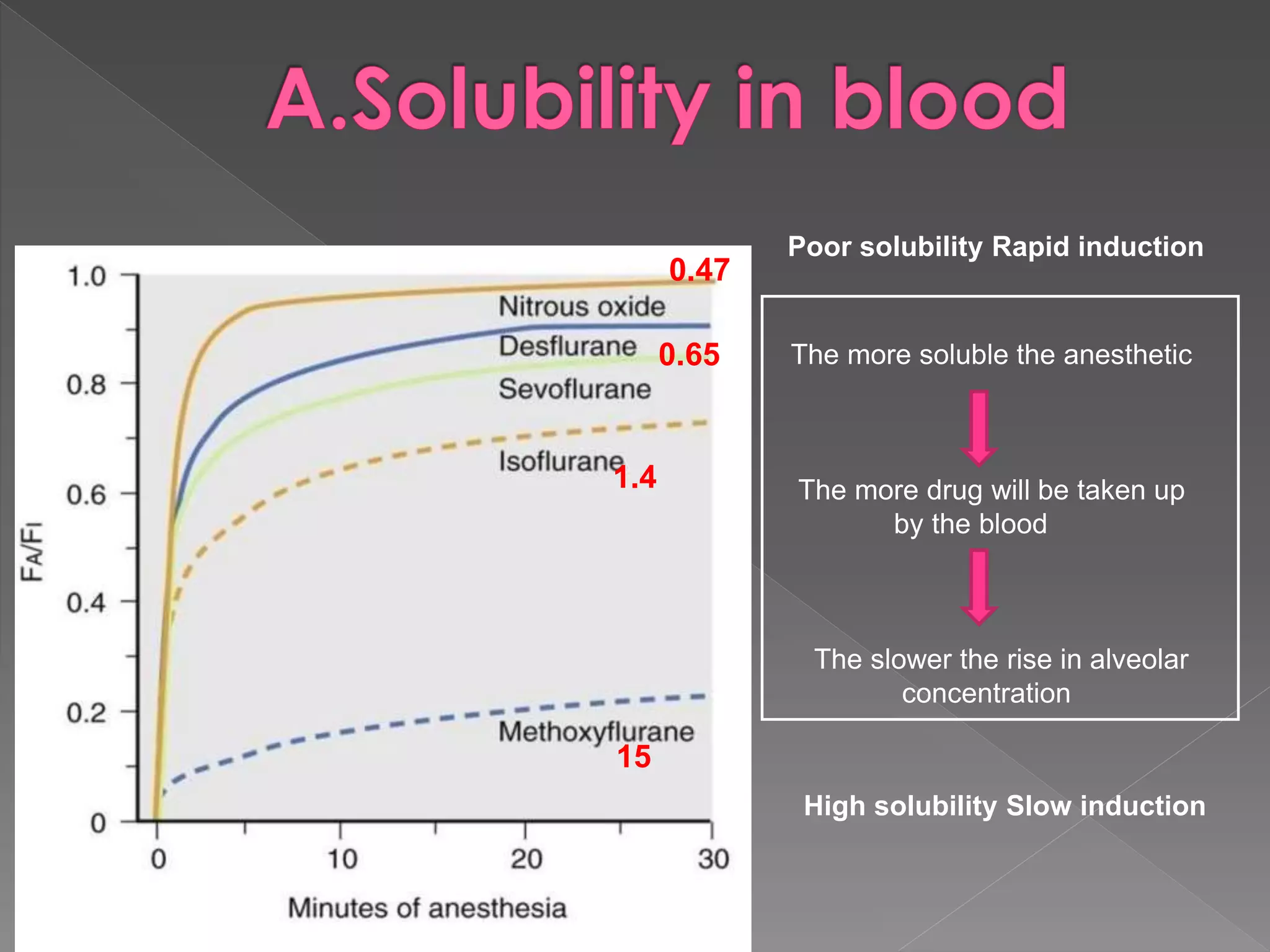
![Uptake from the lung = Blood solubility x Cardiac Output x [PA-PV]
Barometric pressure
U Lung = λB/G x Q x ((PA-Pvenous)
Barometric pressure
Fick equation
λB/G - blood:gas partition coefficient
Q - cardiac output
PA - alveolar partial pressure of anesthetic
Pv - mixed venous partial pressure of anesthetic
PB is barometric pressure.](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-34-2048.jpg)
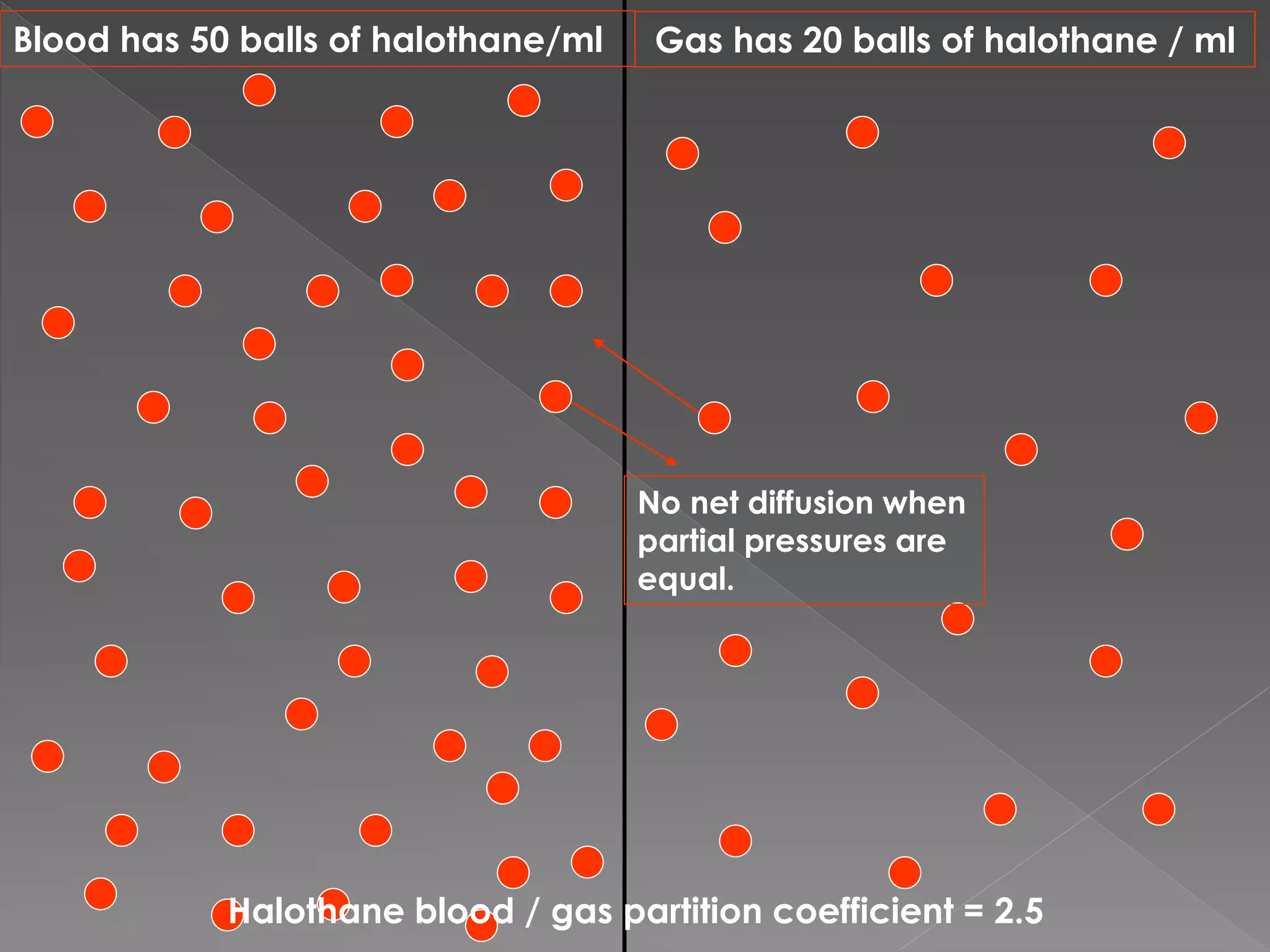
![ Solubility is defined in terms of the partition
coefficient
Partition coefficient is the ratio of the
amount of substance present in one phase
compared with another, the two phases
being of equal volume and in equilibrium
[λB/G = CB ]
CG](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-35-2048.jpg)





![1. The tissue/blood partition coefficient (tissue solubility)
2. The tissue blood flow.
3. The tissue anesthetic concentration
Tissue Uptake = Tissue solubility x Tissue blood flow x [Parterial - PTissue]
Atmospheric pressure](https://image.slidesharecdn.com/ingalationanesthetics-150211135231-conversion-gate01/75/Ingalation-anesthetics-46-2048.jpg)