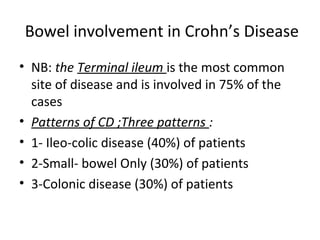
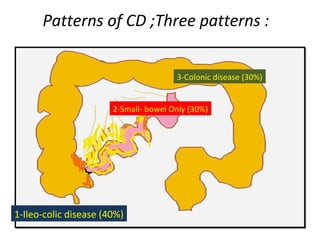
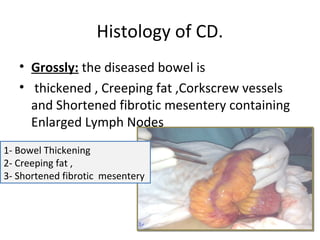
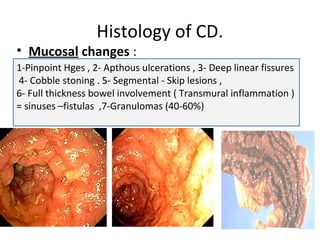
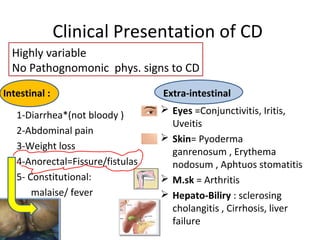
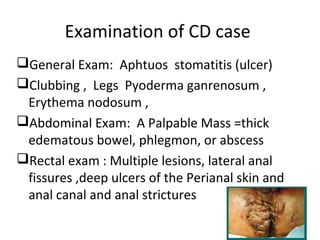
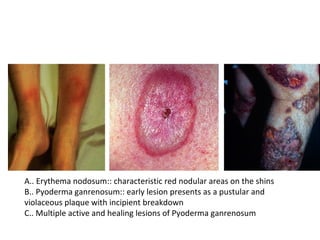
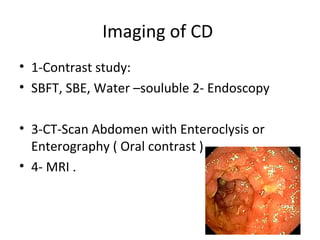
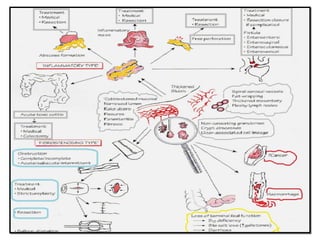
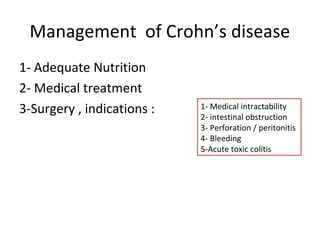
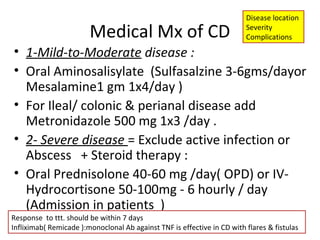
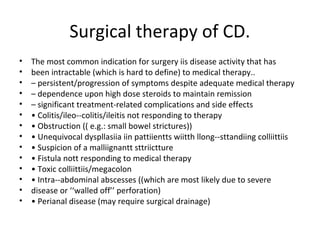
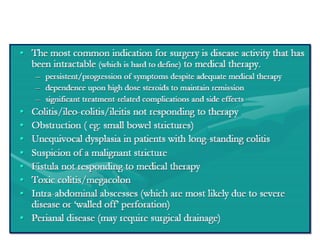
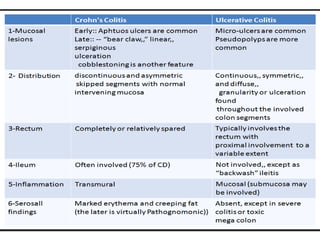
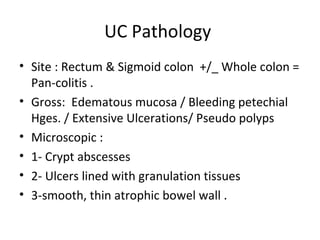
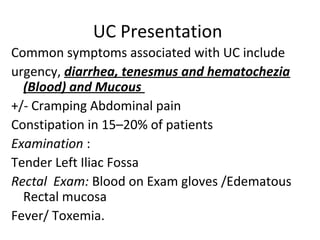
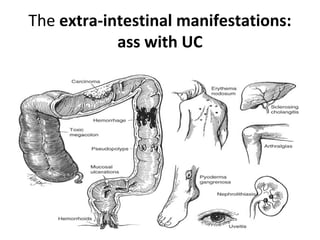
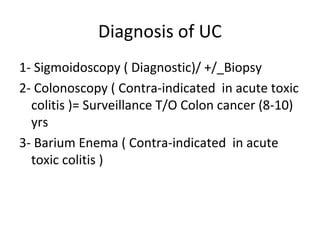
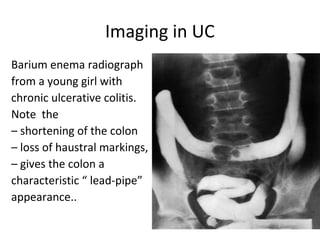
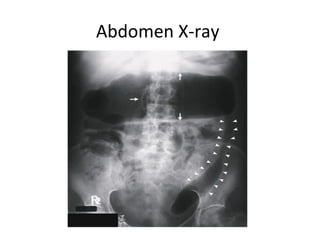
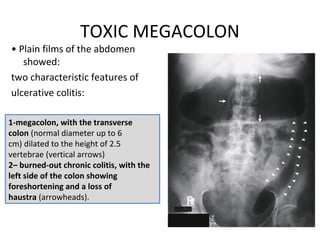
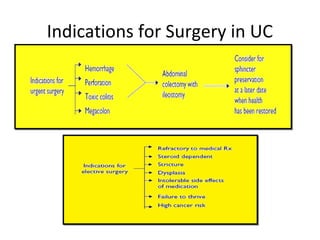
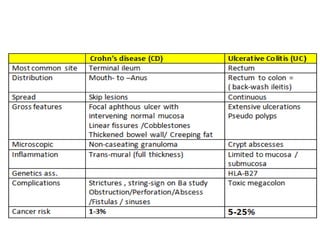
This document provides information on Crohn's disease and ulcerative colitis. It discusses the definition, symptoms, diagnosis, and treatment of Crohn's disease, including that it is a chronic inflammatory bowel disease that can affect any part of the GI tract. It also summarizes ulcerative colitis as an inflammatory disease confined to the colon and rectum, noting its symptoms include bloody diarrhea and abdominal pain. The document provides details on evaluating and managing both conditions medically or surgically.