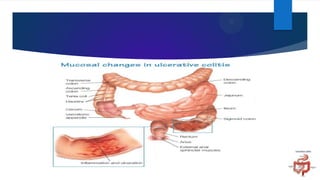
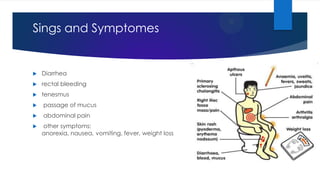
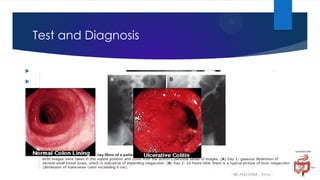
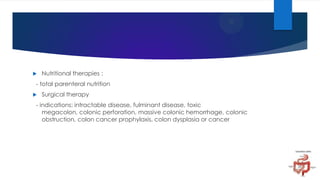
Ulcerative colitis is a chronic inflammatory disease of the colon that causes diarrhea, abdominal pain, and rectal bleeding. The disease involves inflammation and ulceration of the innermost lining of the colon. A colonoscopy with biopsies is usually required for diagnosis. Treatment involves medications to reduce inflammation and surgery to remove the colon in severe cases. Complications can include severe bleeding, colon perforation, and an increased risk of colon cancer.