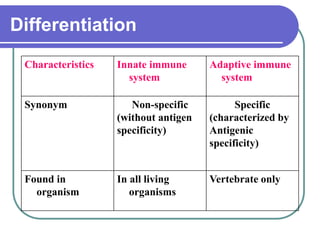
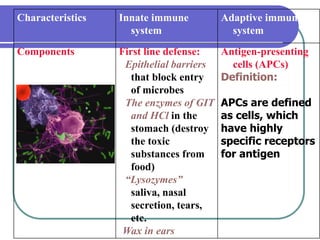
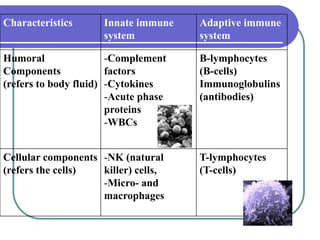
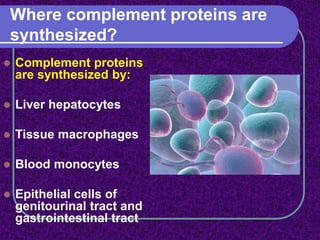
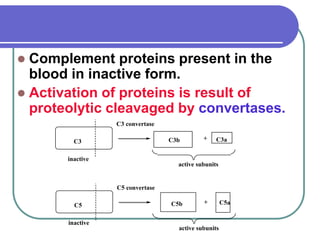
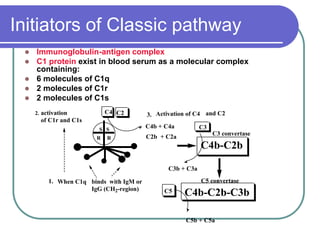
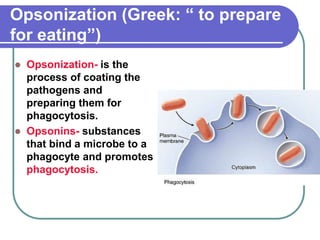
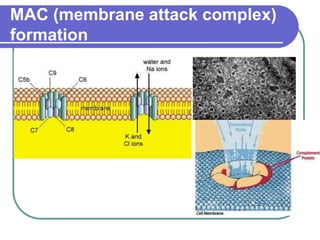
The document defines immunity and distinguishes between innate and adaptive immunity, outlining their characteristics and components. It provides an in-depth explanation of the complement system, its activation pathways, and the roles of various proteins in pathogen clearance and inflammatory responses. Additionally, it discusses complement deficiencies and their clinical manifestations, highlighting their association with conditions like systemic lupus erythematosus and glomerulonephritis.