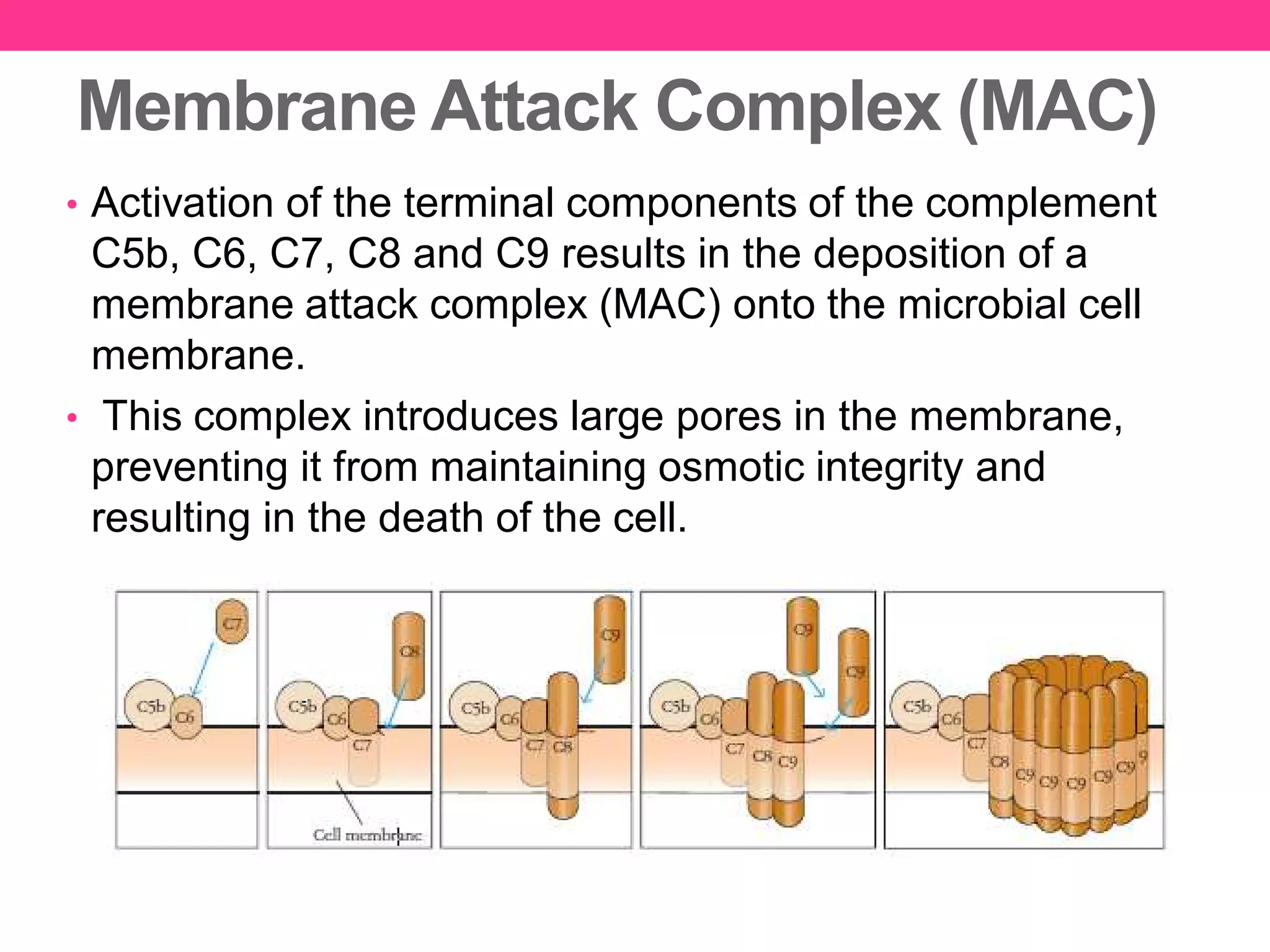
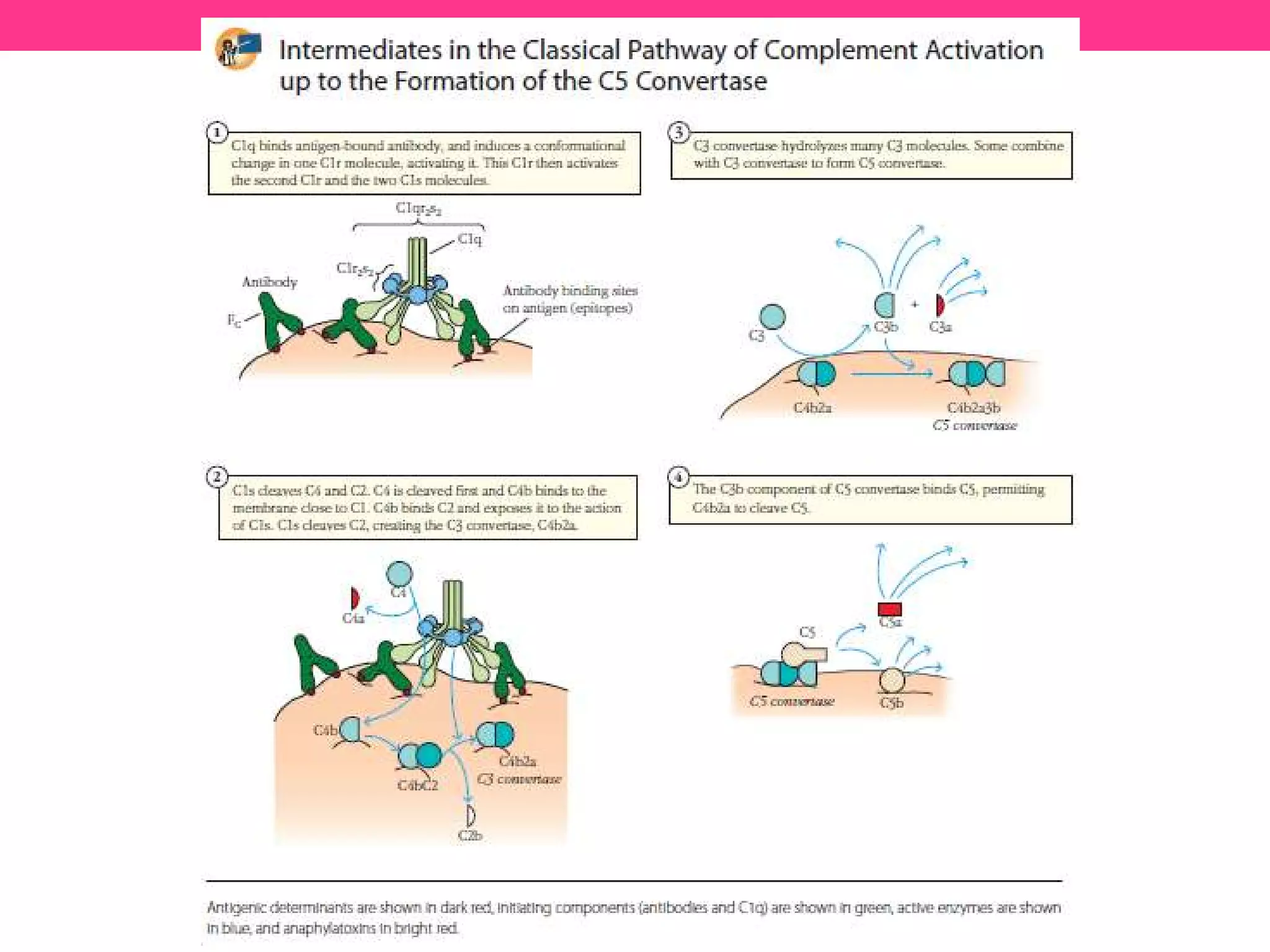
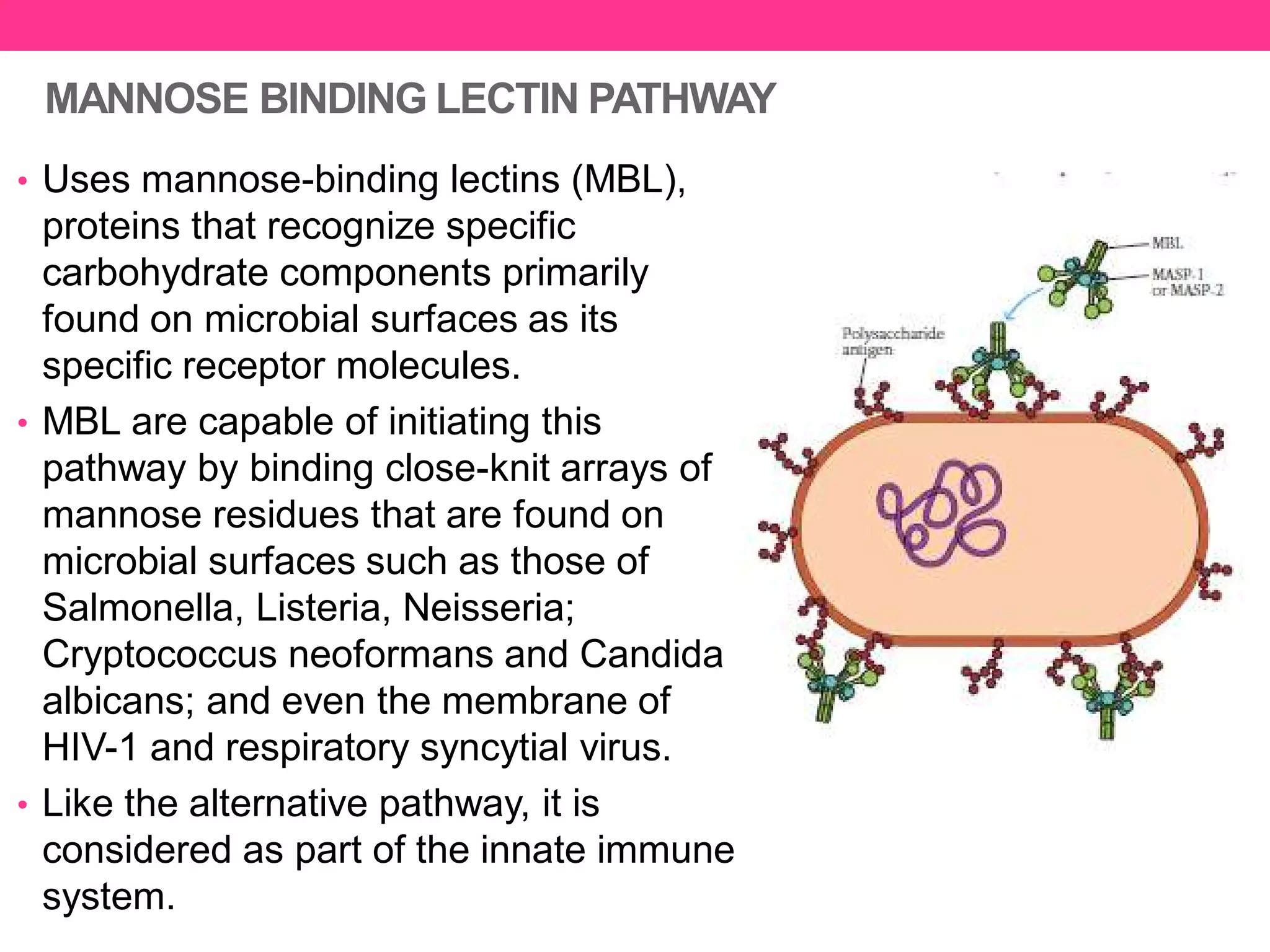
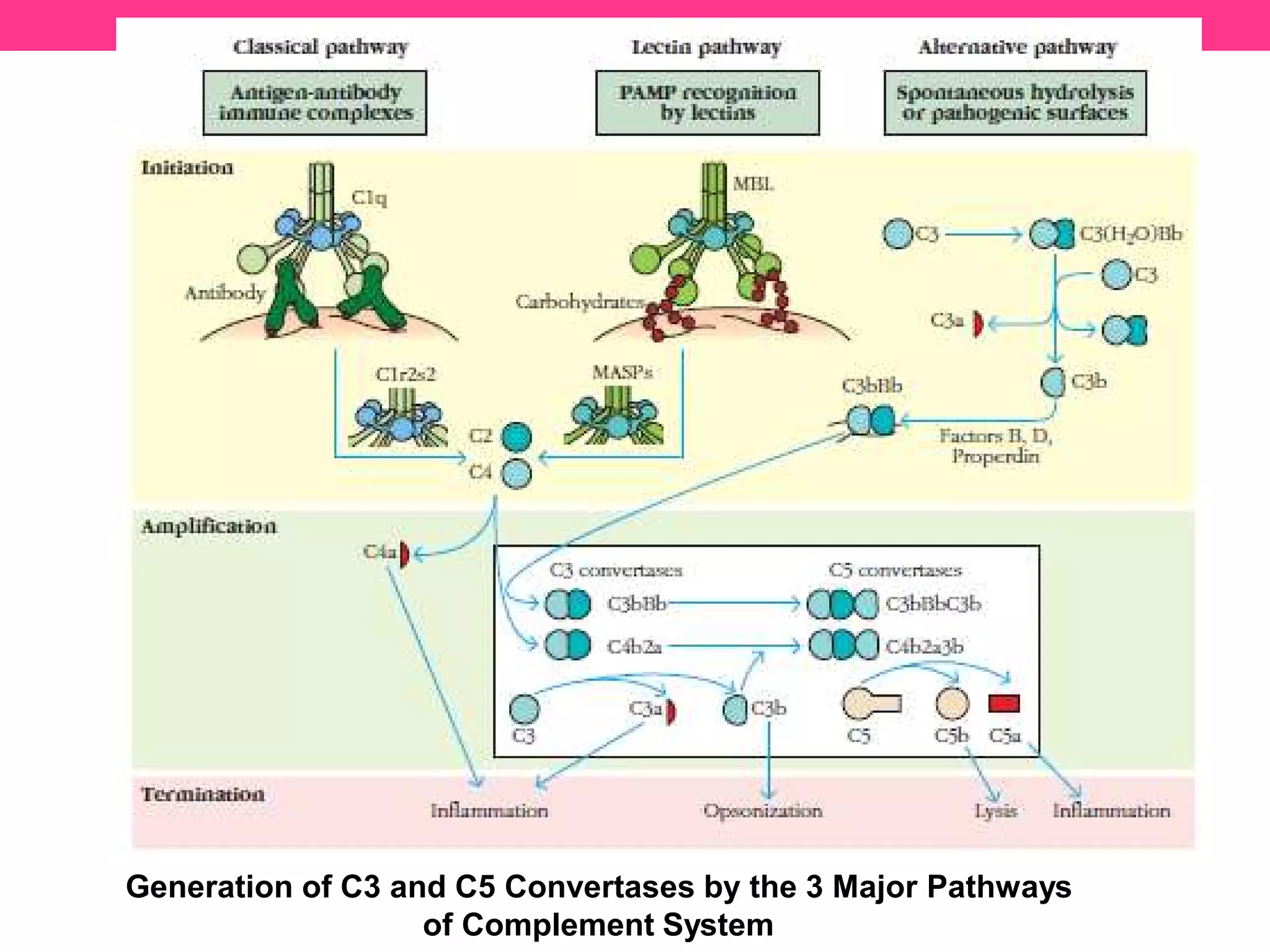
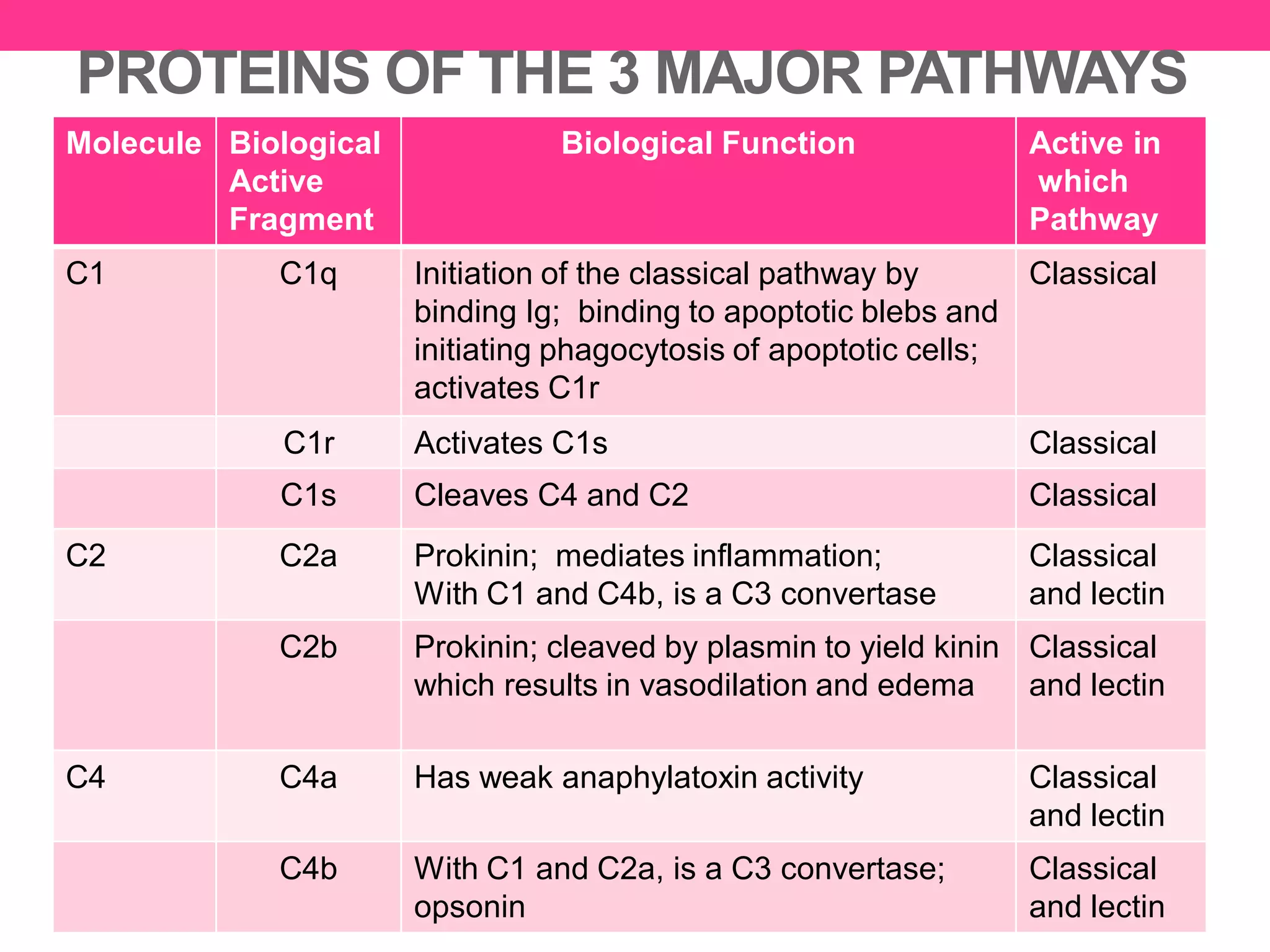
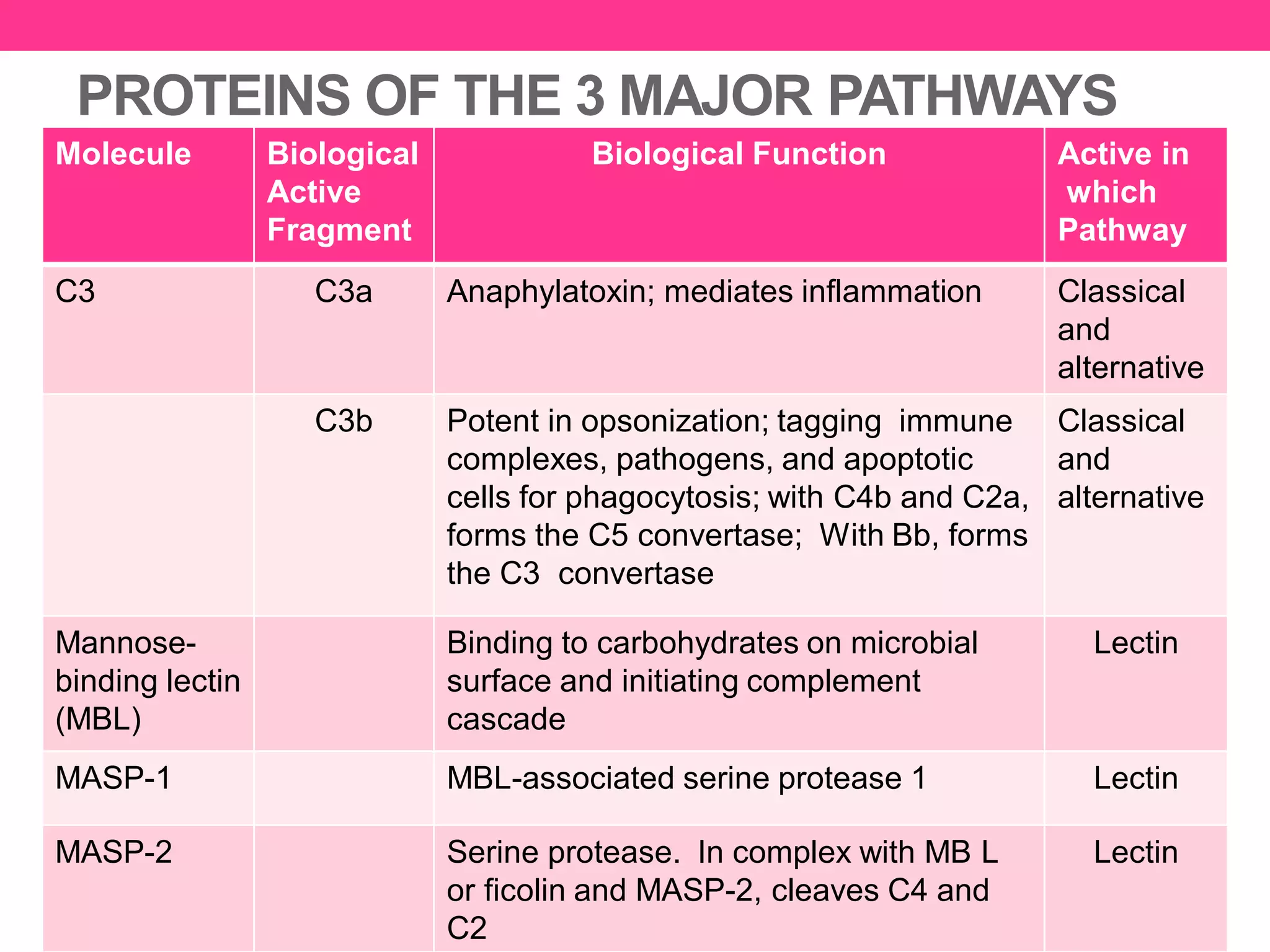
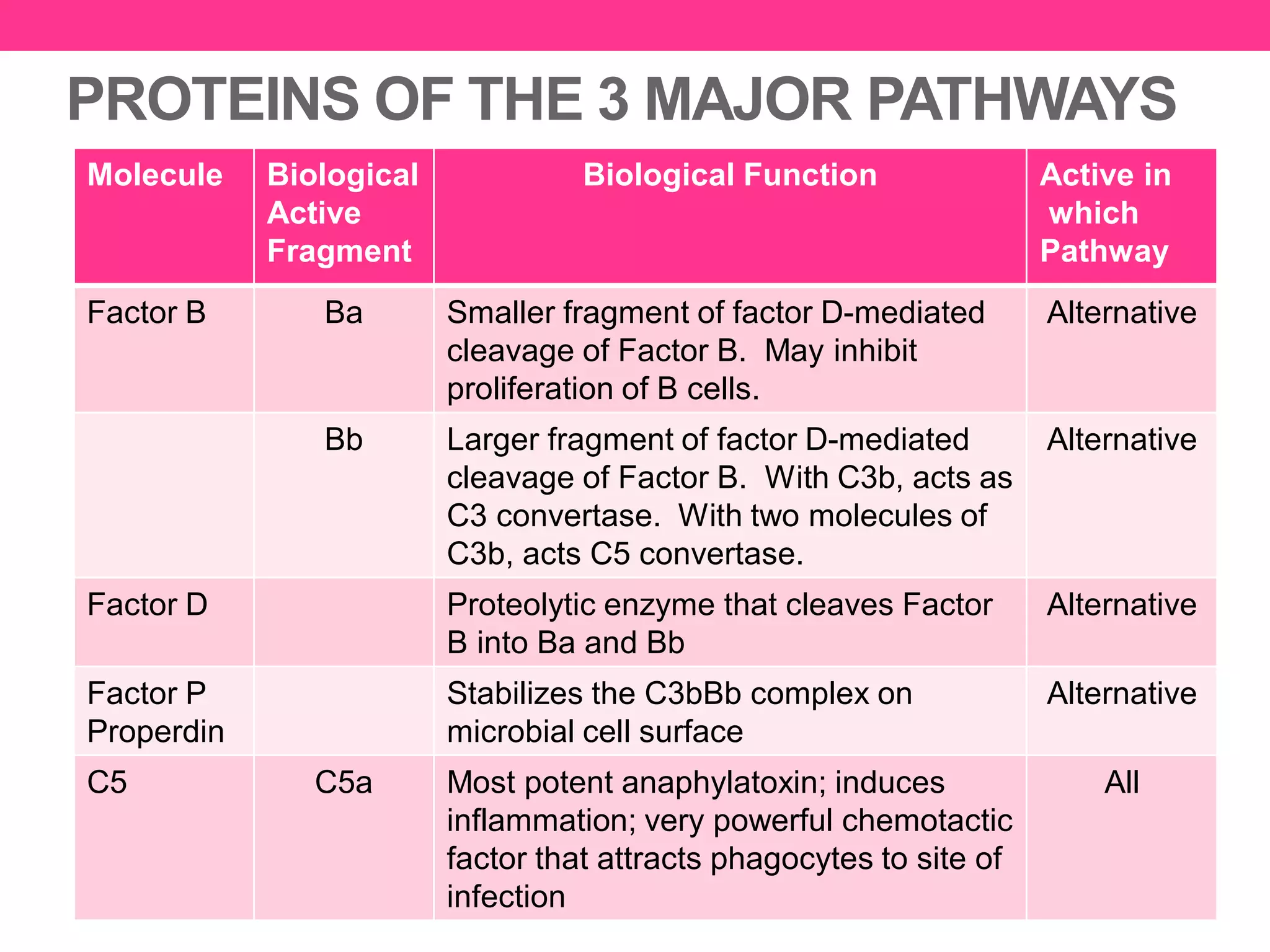
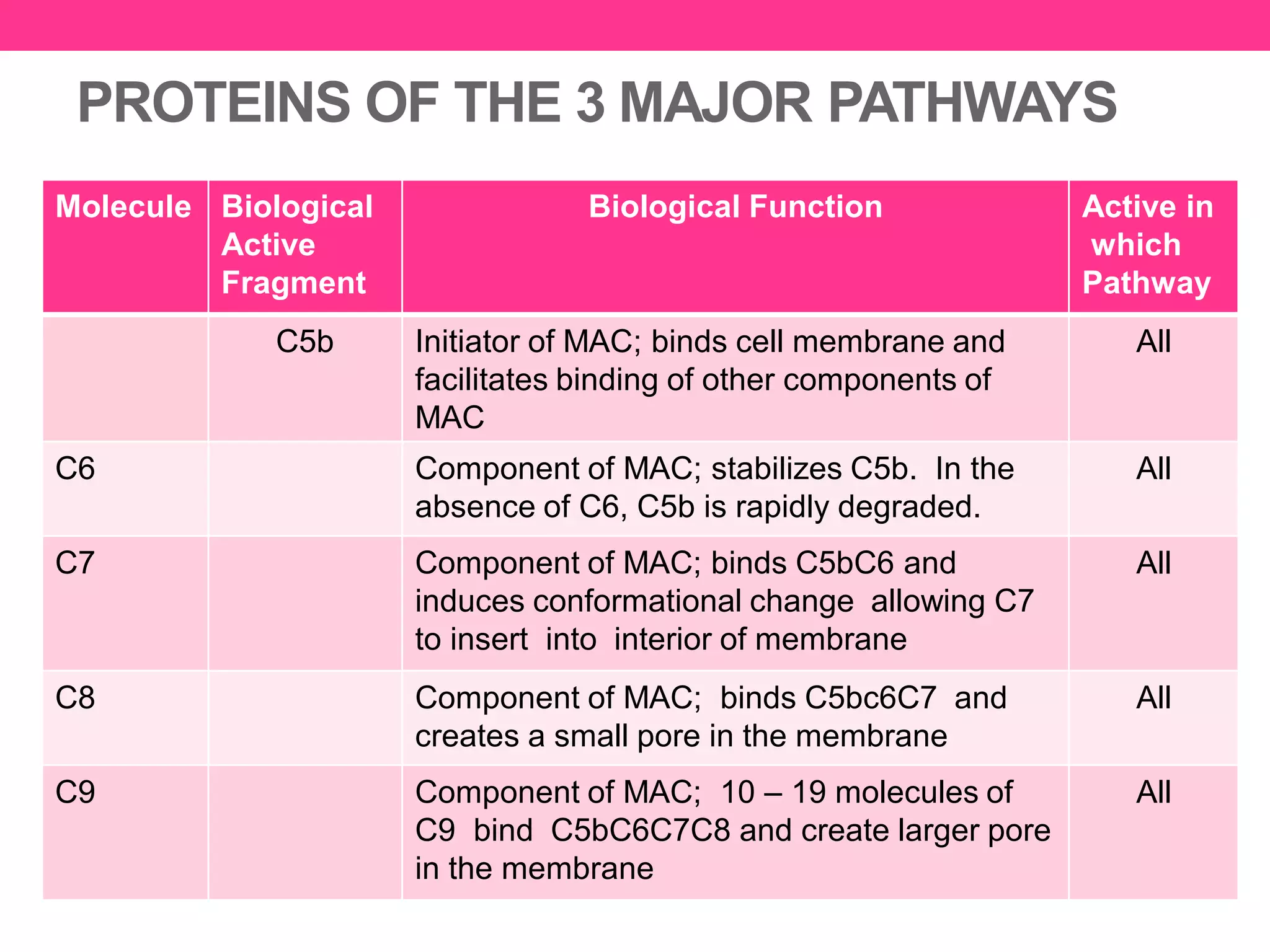
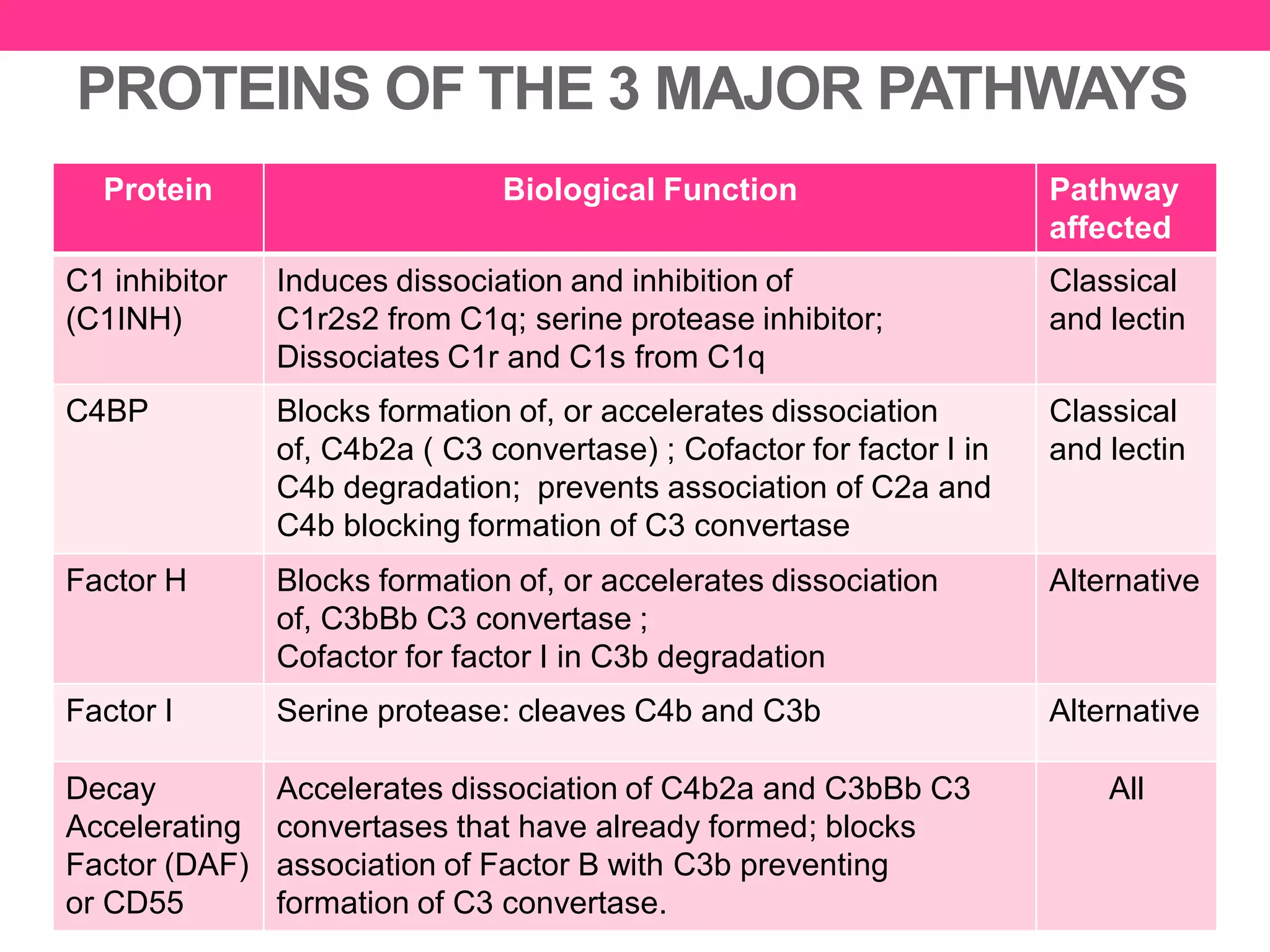
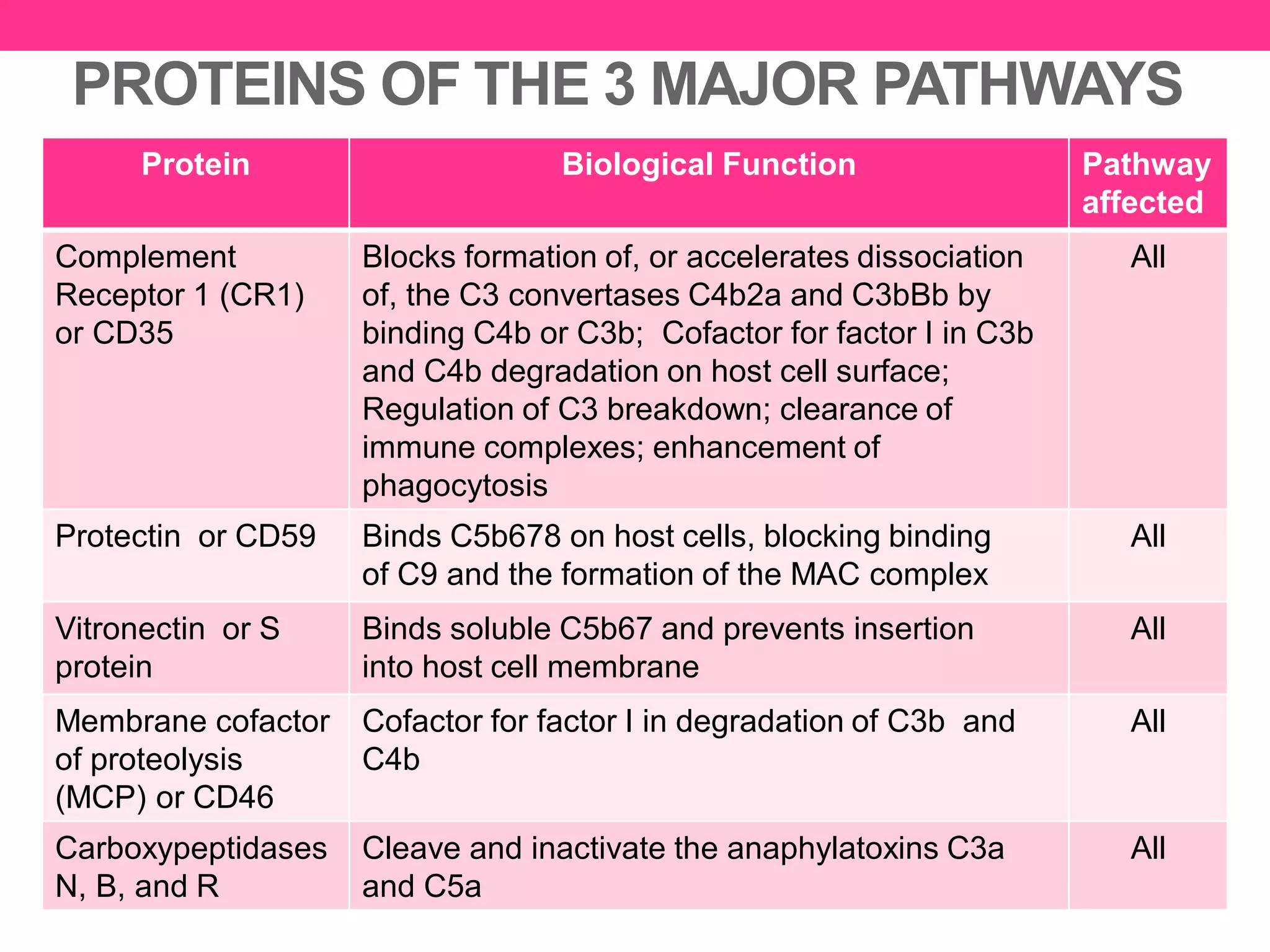
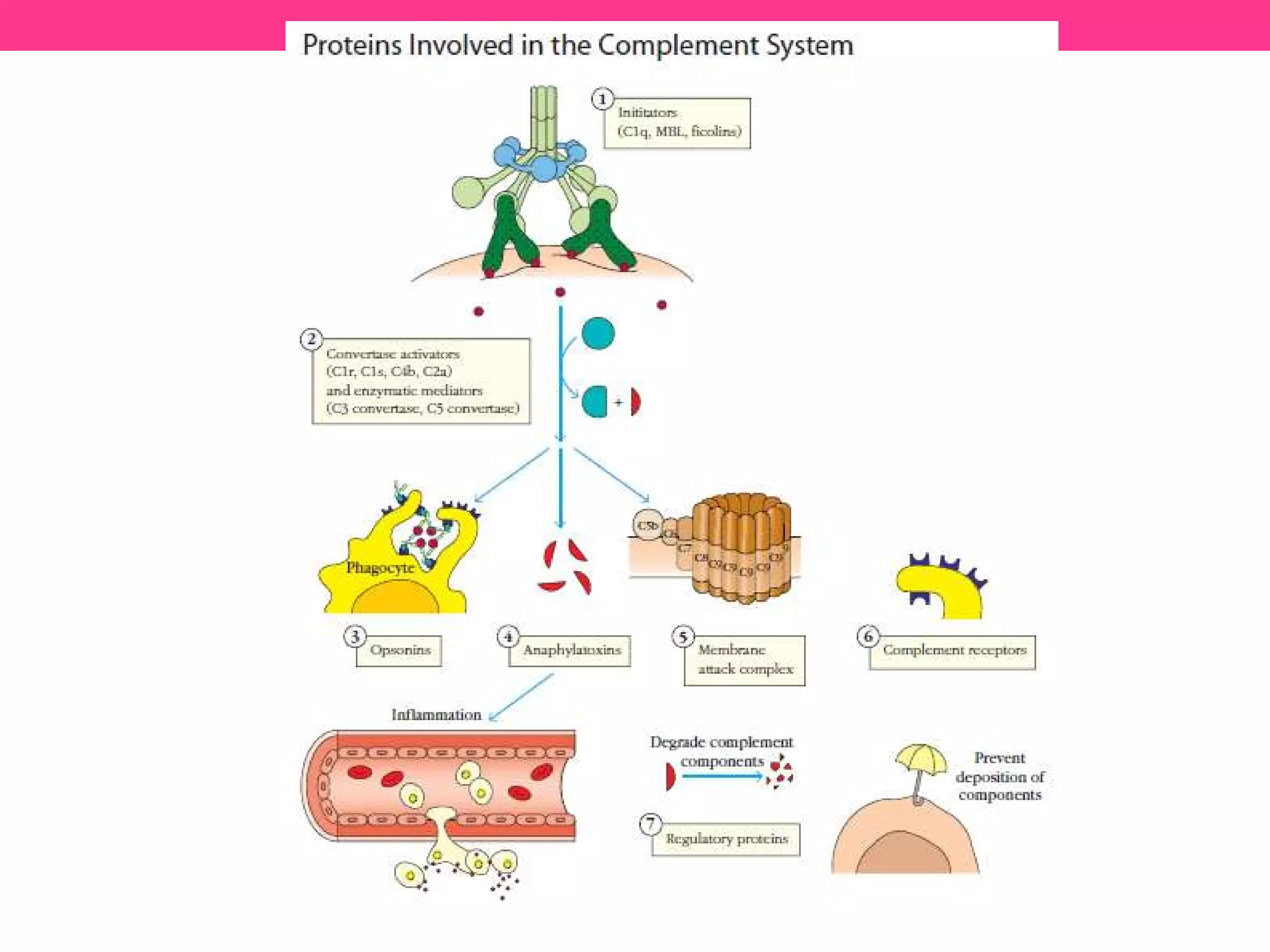
The complement system consists of over 30 proteins that circulate in the blood and tissues. It helps destroy harmful microbes via opsonization, phagocytosis, cytolysis, and inflammation. There are 3 major pathways - classical, lectin, and alternative - that are initiated by different mechanisms but all generate C3 and C5 convertases and the membrane attack complex (MAC). Complement proteins include initiators, enzymes, opsonins, anaphylatoxins, membrane attack components, receptors, and regulators. Together they help bridge the innate and adaptive immune responses.