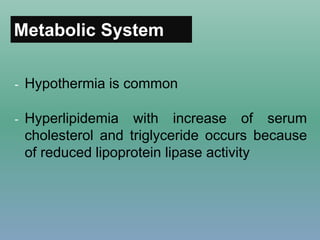
This document provides information on hypothyroidism, including:
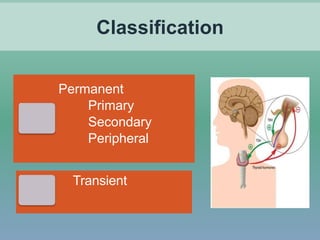
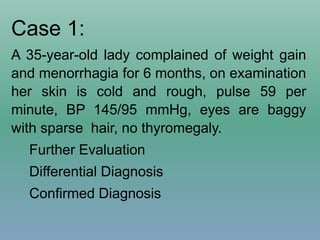
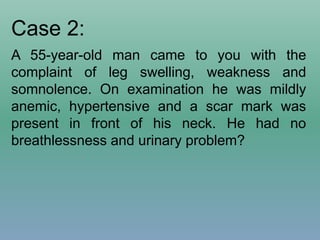
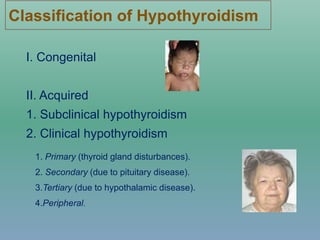
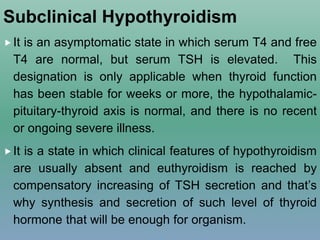
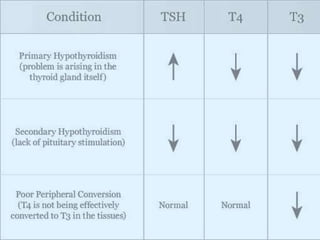
- Definitions and classifications of hypothyroidism
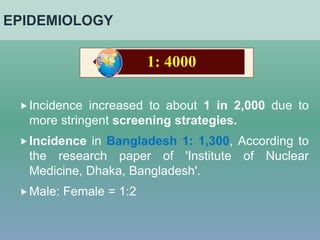
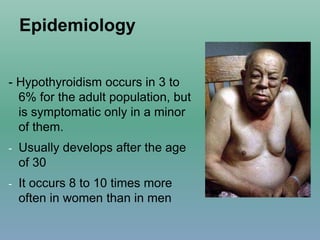
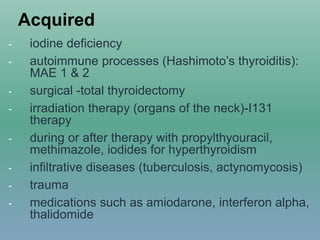
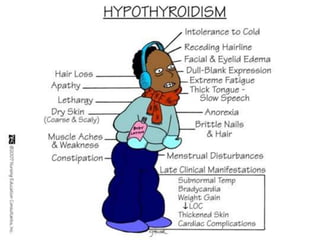
- Epidemiology, etiologies, clinical features, diagnosis and treatment of acquired hypothyroidism
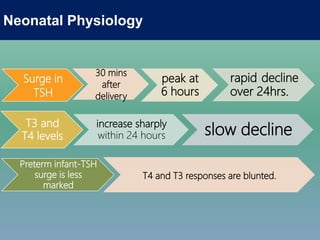
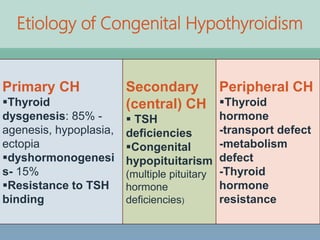
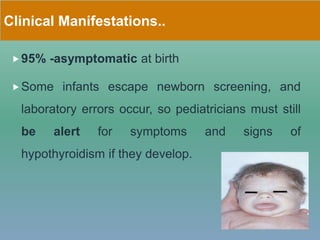
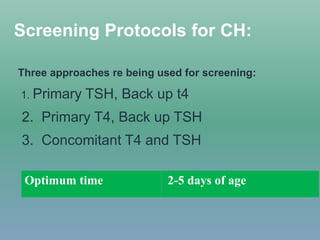
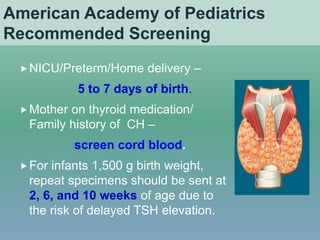
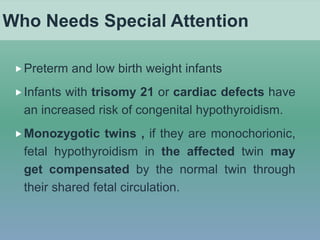
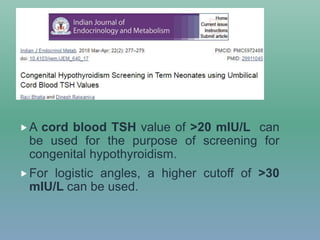
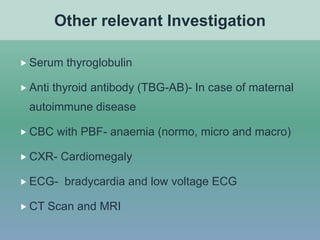
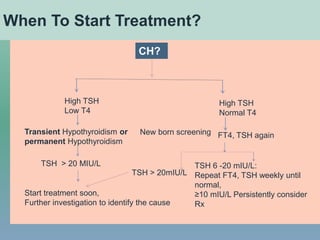
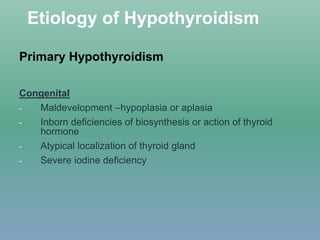
- Etiologies, clinical manifestations, newborn screening and protocols for congenital hypothyroidism
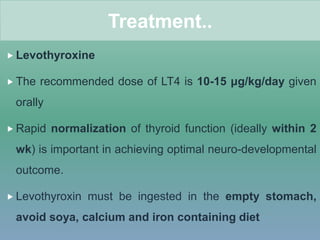
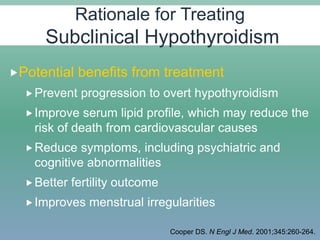
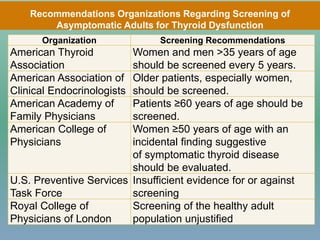
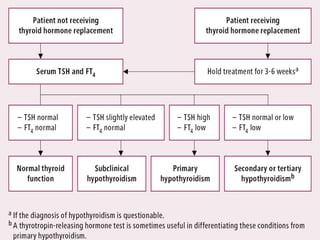
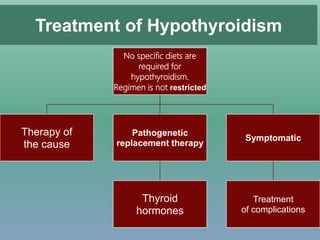
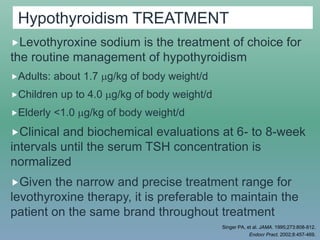
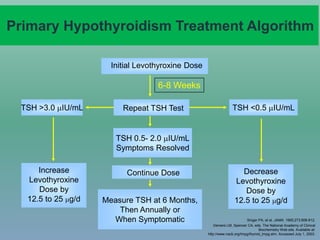
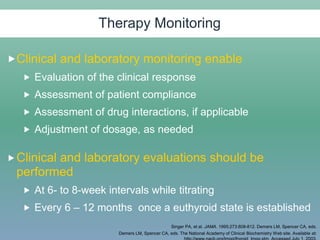
It discusses evaluation, management, and goals of treatment for hypothyroidism with levothyroxine replacement therapy and monitoring. It also addresses subclinical hypothyroidism and factors that can impact levothyroxine effectiveness.
![Caution in Patients with Underlying
Cardiac Disease
Using LT4 in those with IHD increases the risk of MI,
aggravation of angina, or cardiac arrhythmias
For patients <50 years of age with underlying
cardiac disease, initiate LT4 at 25-50 g/d with
gradual dose increments at 6- to 8-week intervals
For elderly patients with cardiac disease, start LT4 at
12.5-25 g/d, with gradual dose increments at 4- to
6-week intervals
The LT4 dose is generally adjusted in 12.5-25 g
increments
Braverman LE, et al. Werner & Ingbar’s The Thyroid. A Fundamental and Clinical Text. 8th ed. 2000.
Kohno A, et al. Endocr J. 2001;48:565-572.
Synthroid® [package insert]. Abbott Laboratories; 2003.](https://image.slidesharecdn.com/2-210121133207/85/Hypothyroidism-Evaluation-Management-by-Dr-Selim-31-320.jpg)
![Factors That May Reduce Levothyroxine Effectiveness
Malabsorption Syndromes
Post-jejunoileal bypass
surgery
Short bowel syndrome
Celiac disease
Reduced Absorption
Colestipol hydrochloride
Sucralfate
Ferrous sulfate
Food (eg, soybean formula)
Aluminum hydroxide
Cholestyramine
Sodium polystyrene
sulfonate
Drugs That Increase
Clearance
Rifampin
Carbamazepine
Phenytoin
Factors That Reduced T4 to
T3 Clearance
Amiodarone
Selenium deficiency
Other Mechanisms
Lovastatin
Sertraline
Braverman LE, Utiger RD, eds. The Thyroid: A Fundamental and Clinical Text. 8th ed. 2000.
Synthroid® [package insert]. Abbott Laboratories; 2003.](https://image.slidesharecdn.com/2-210121133207/85/Hypothyroidism-Evaluation-Management-by-Dr-Selim-32-320.jpg)