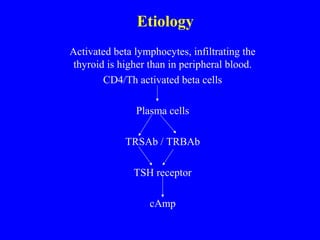
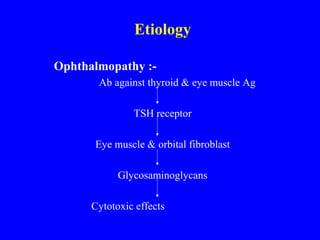
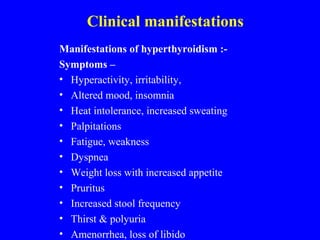
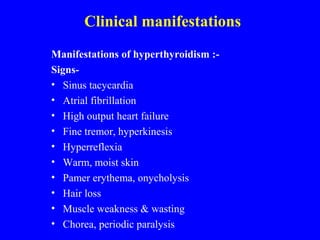
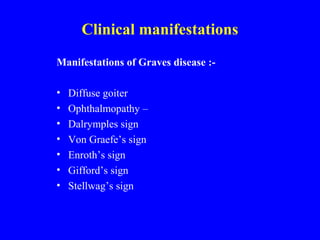
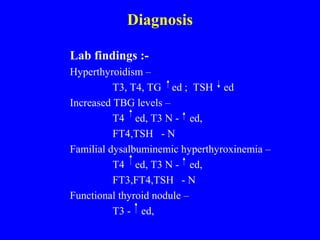
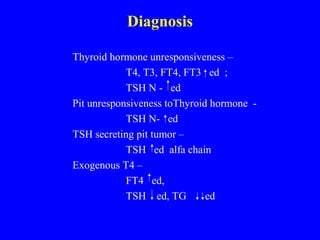
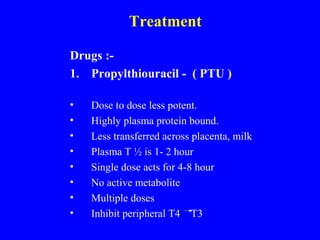
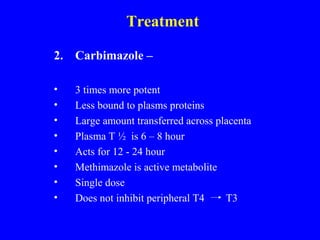
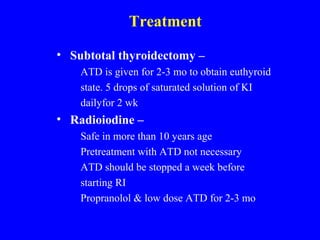
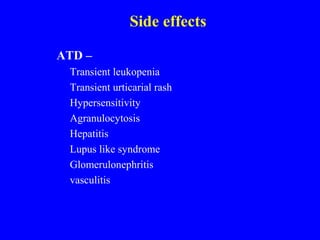
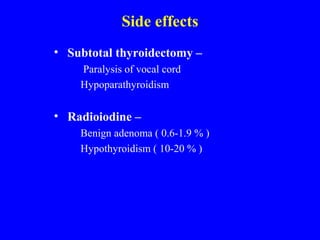
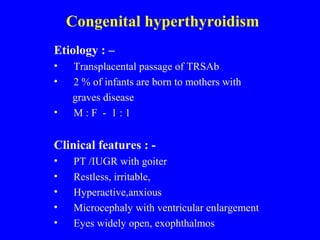
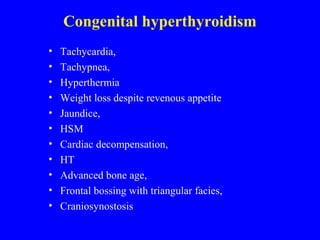
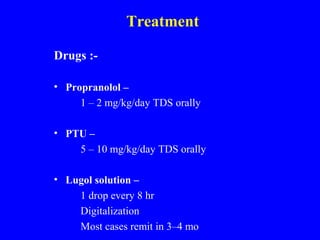
This document discusses hyperthyroidism, its causes, clinical manifestations, diagnosis, and treatment. The main causes discussed are Graves' disease, toxic multinodular goiter, and toxic adenomas. Graves' disease is an autoimmune disorder causing thyroid infiltration. Clinical manifestations include symptoms of hyperthyroidism as well as signs specific to Graves' such as ophthalmopathy. Diagnosis involves thyroid hormone blood tests. Treatment options include antithyroid medications, radioactive iodine therapy, and subtotal thyroidectomy. Congenital hyperthyroidism can occur when mothers pass antibodies to their infants and requires similar treatments.