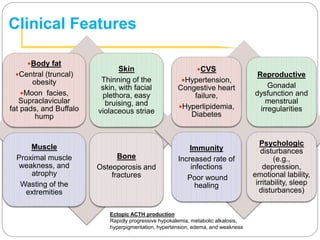
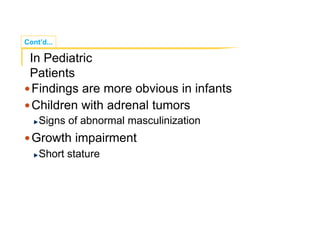
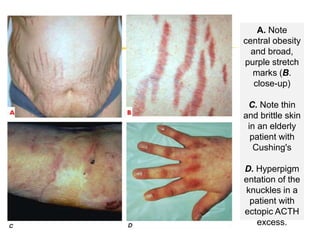
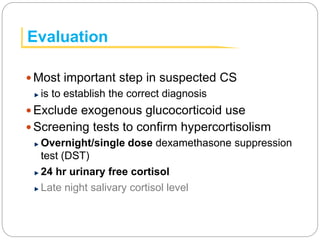
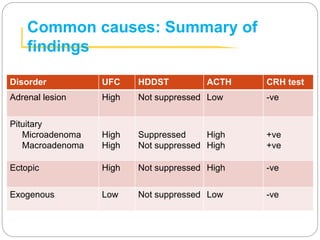
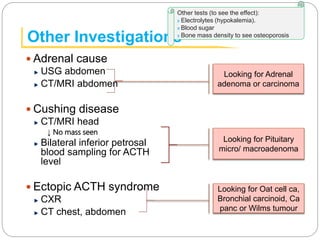
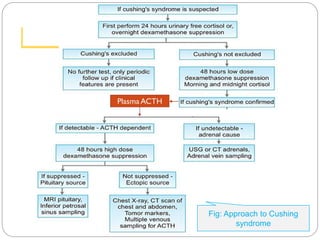
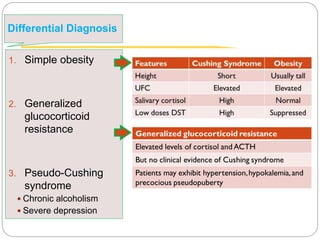
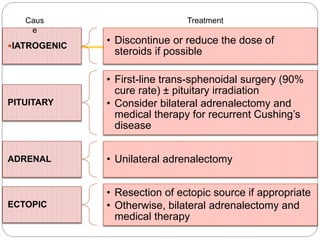
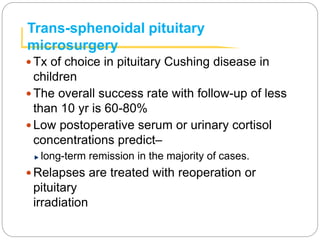
This document discusses Cushing's syndrome, which results from high cortisol levels in the blood. It can be caused by exogenous glucocorticoid use, pituitary tumors, adrenal tumors, or ectopic ACTH-secreting tumors. Signs include central obesity, thin skin, high blood pressure, and bone weakness. Diagnosis involves screening tests like dexamethasone suppression tests and measuring ACTH and cortisol levels. If endogenous, further tests localize the source and guide treatment like surgery, radiation, or medication. The most common causes and their treatment approaches are summarized.

![Cont’d...
If Dx of Cushing syndrome has been established
then,
The next step is to find out the cause
↓
Serum ACTH level
If low or undetectable– ACTH independent cause
[Adrenal cause likely]
If high– Cushing’s disease or Ectopic ACTH syndrome
Two differentiate between these two: High dose DST is to be done](https://image.slidesharecdn.com/cushingsyndrome-161203172423/85/Cushing-syndrome-10-320.jpg)

![Medical therapy
Inhibitors of adrenal steroidogenesis
[Metyrapone, ketoconazole, aminoglutethimide,
etomidate]
Used preoperatively to normalize circulating cortisol
levels
Centrally acting serotonin antagonist
[Cyproheptadine]
Blocks ACTH release](https://image.slidesharecdn.com/cushingsyndrome-161203172423/85/Cushing-syndrome-20-320.jpg)