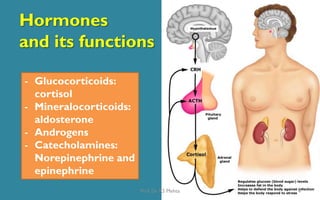
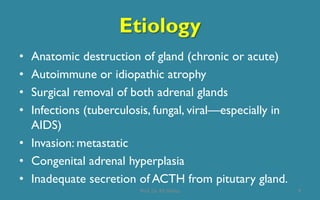
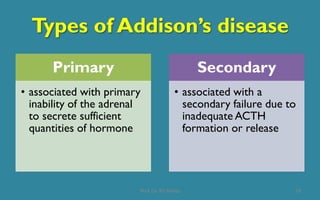
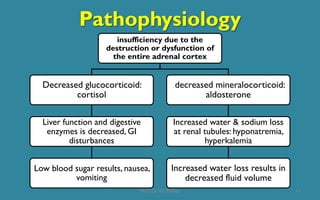
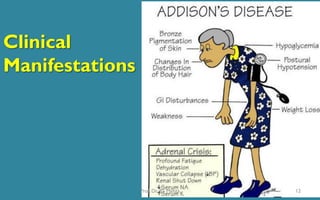
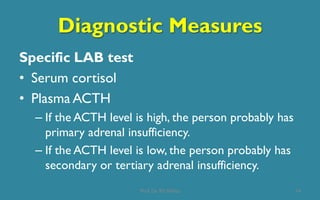
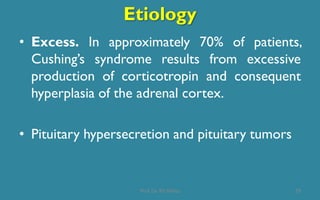
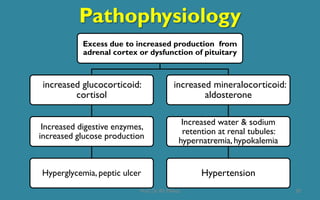
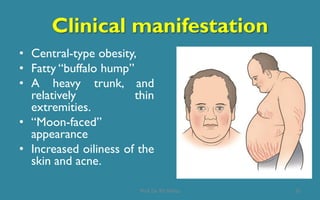
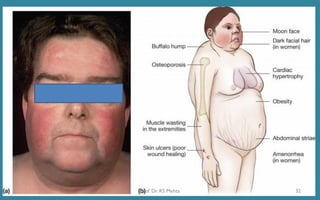
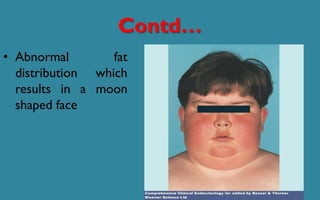
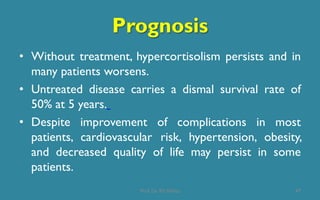
Addison's disease and Cushing's syndrome are both adrenal disorders but with opposite causes and manifestations. Addison's disease is caused by adrenal insufficiency leading to low cortisol and aldosterone. Symptoms include fatigue, weight loss, hyperpigmentation and hypotension. Cushing's syndrome is caused by excessive cortisol secretion leading to central obesity, hypertension and hyperglycemia. Diagnosis involves blood and urine tests to measure hormone levels. Treatment of Addison's disease involves hormone replacement therapy while treatment of Cushing's focuses on reducing excess cortisol levels through surgery, radiation or drug therapy.