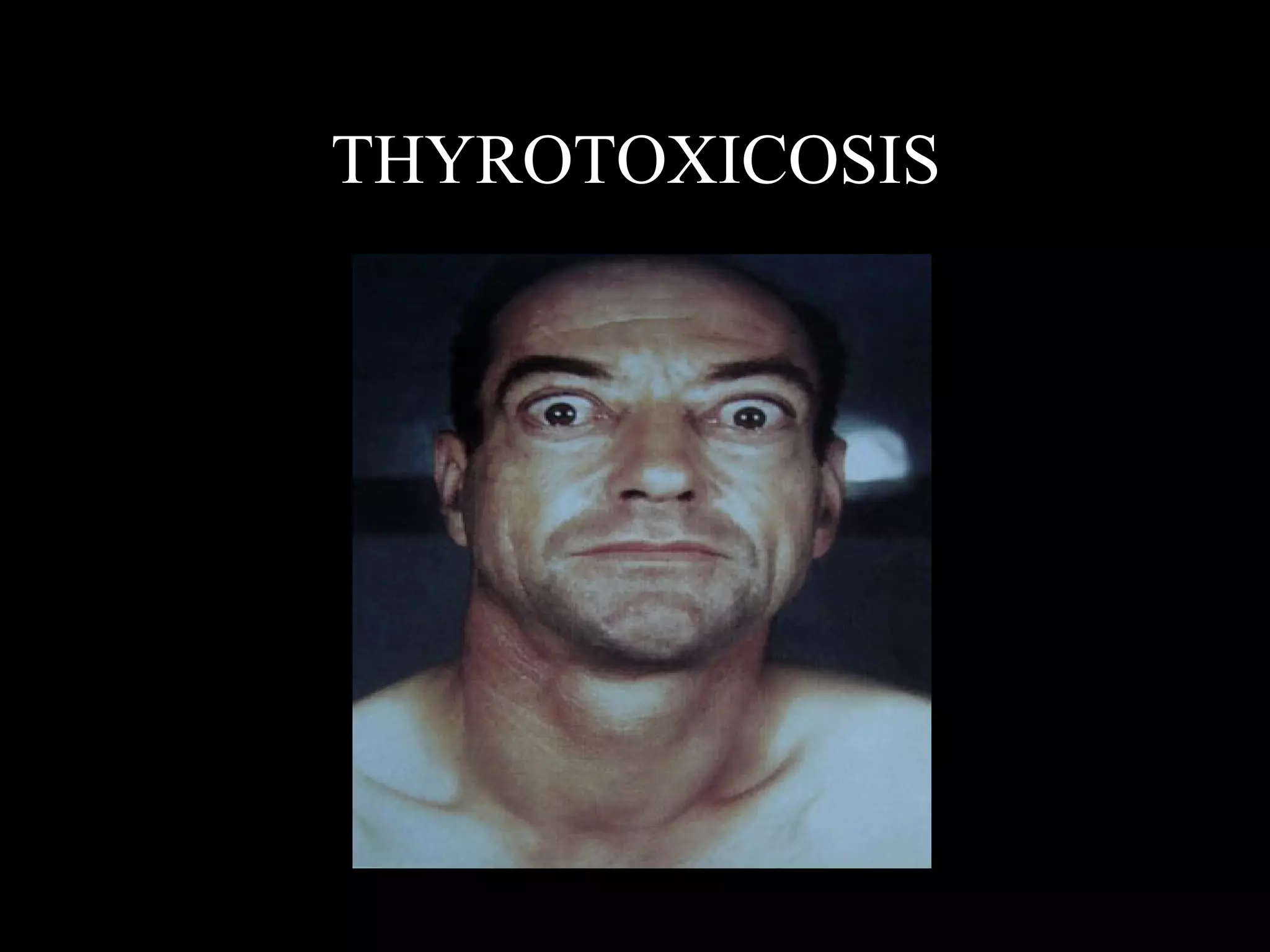
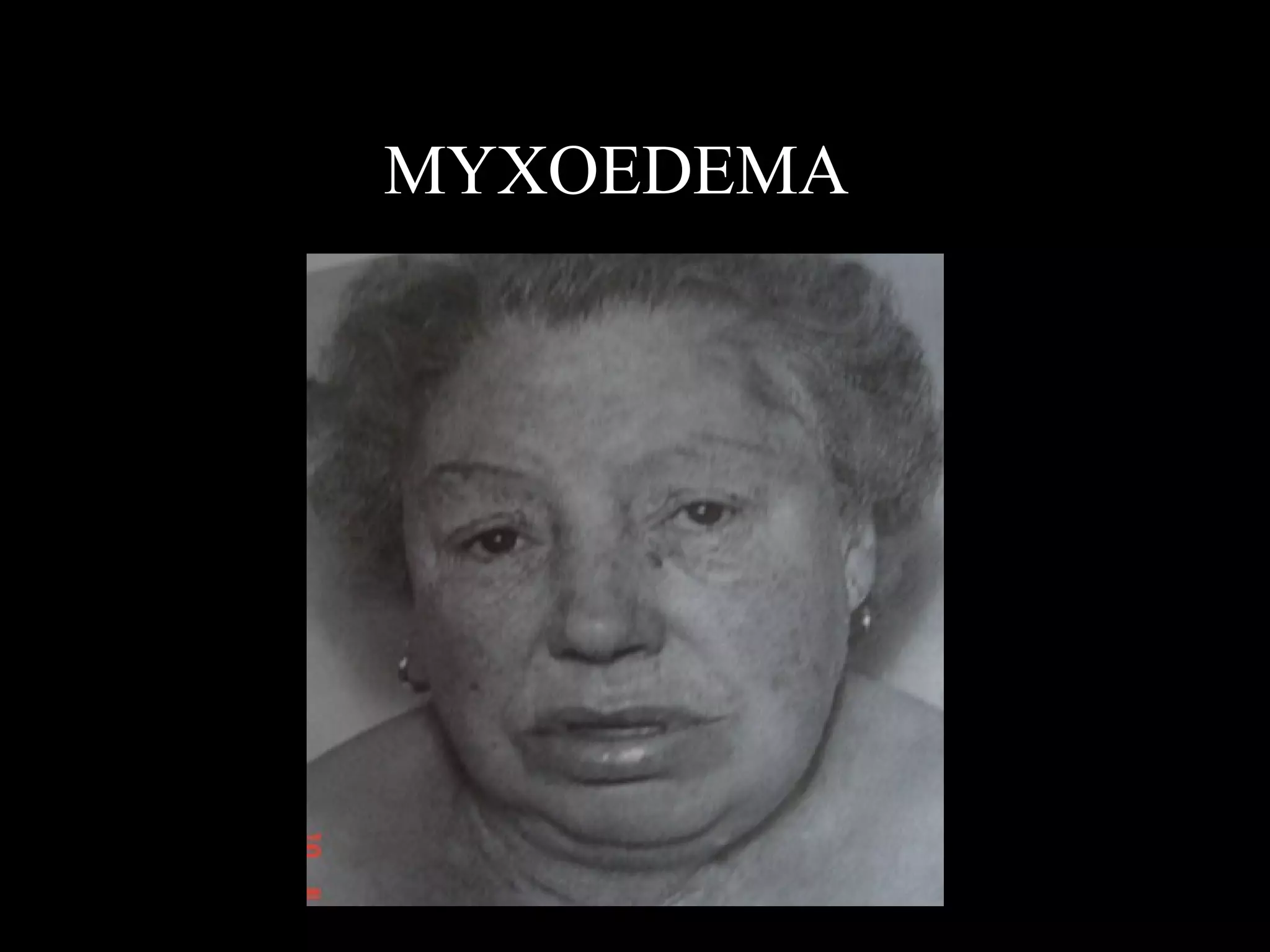
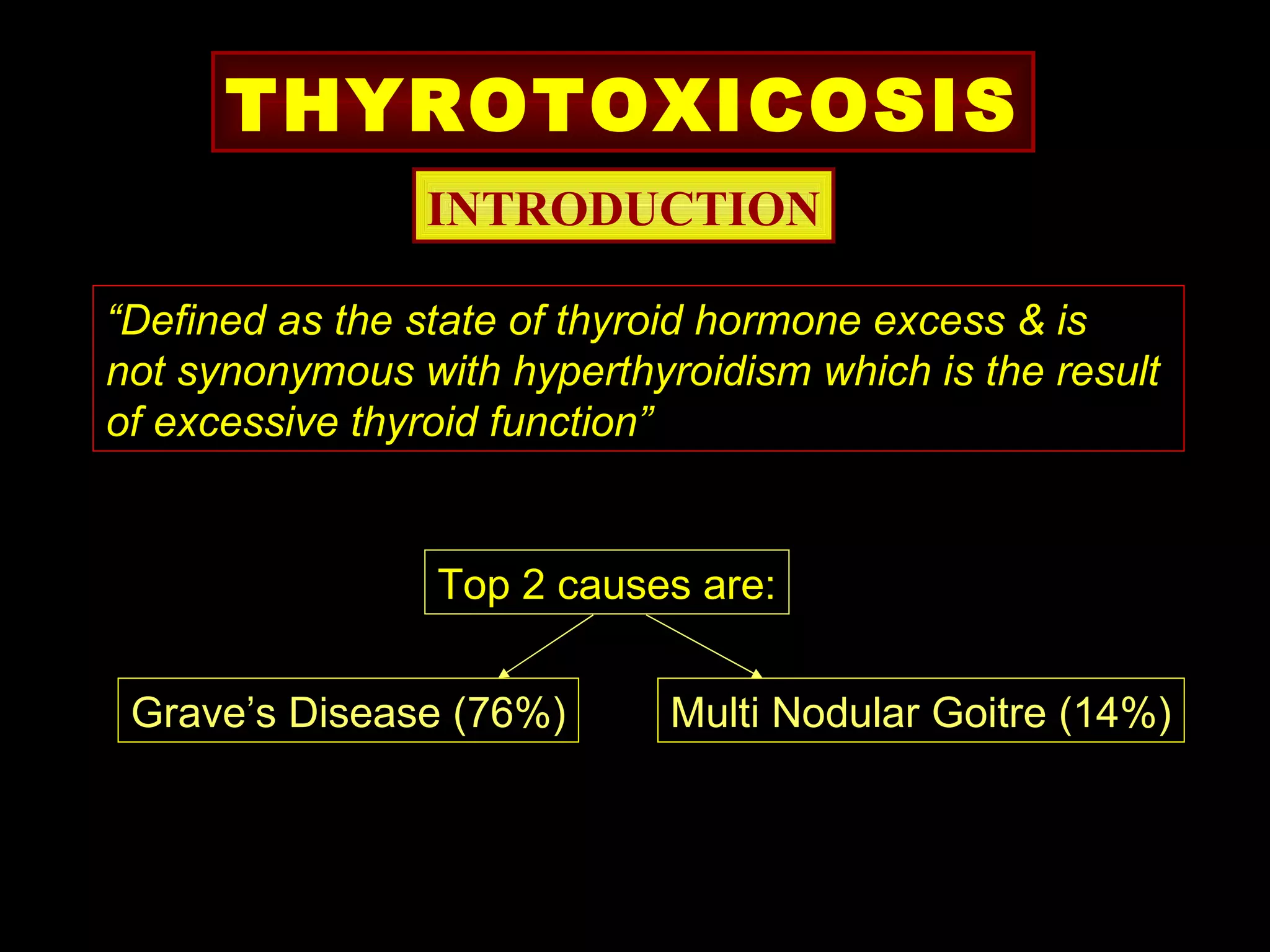
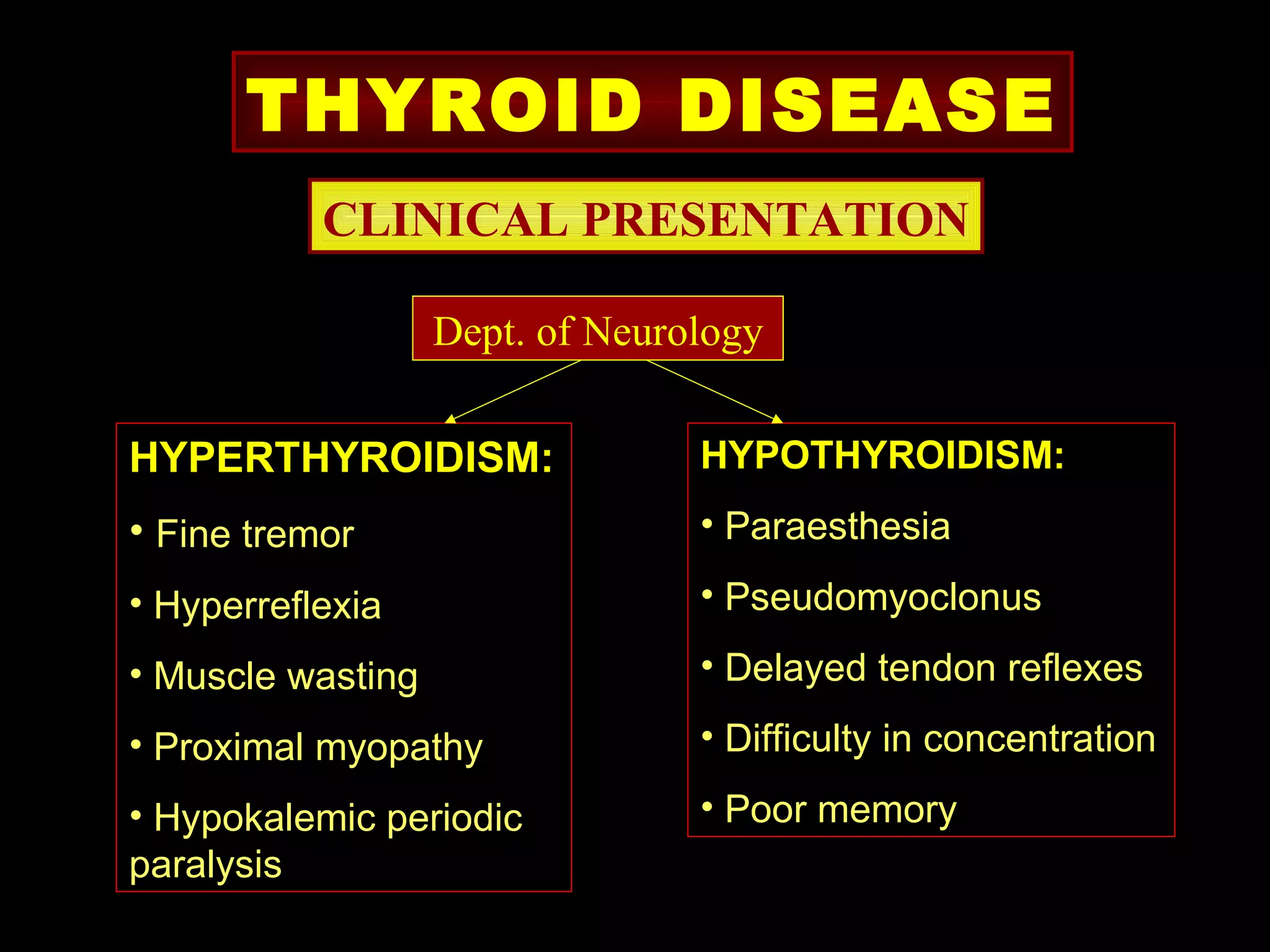
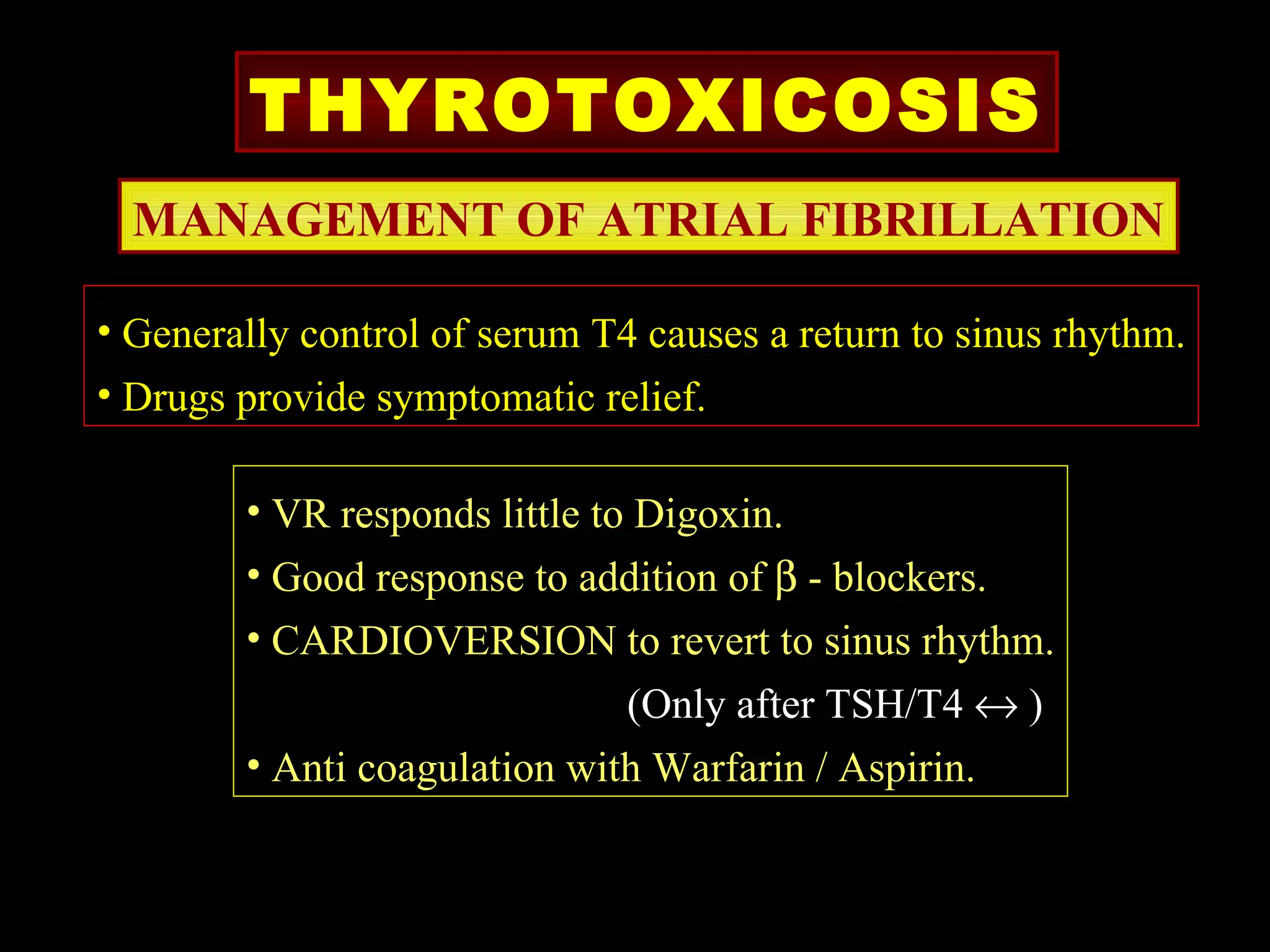
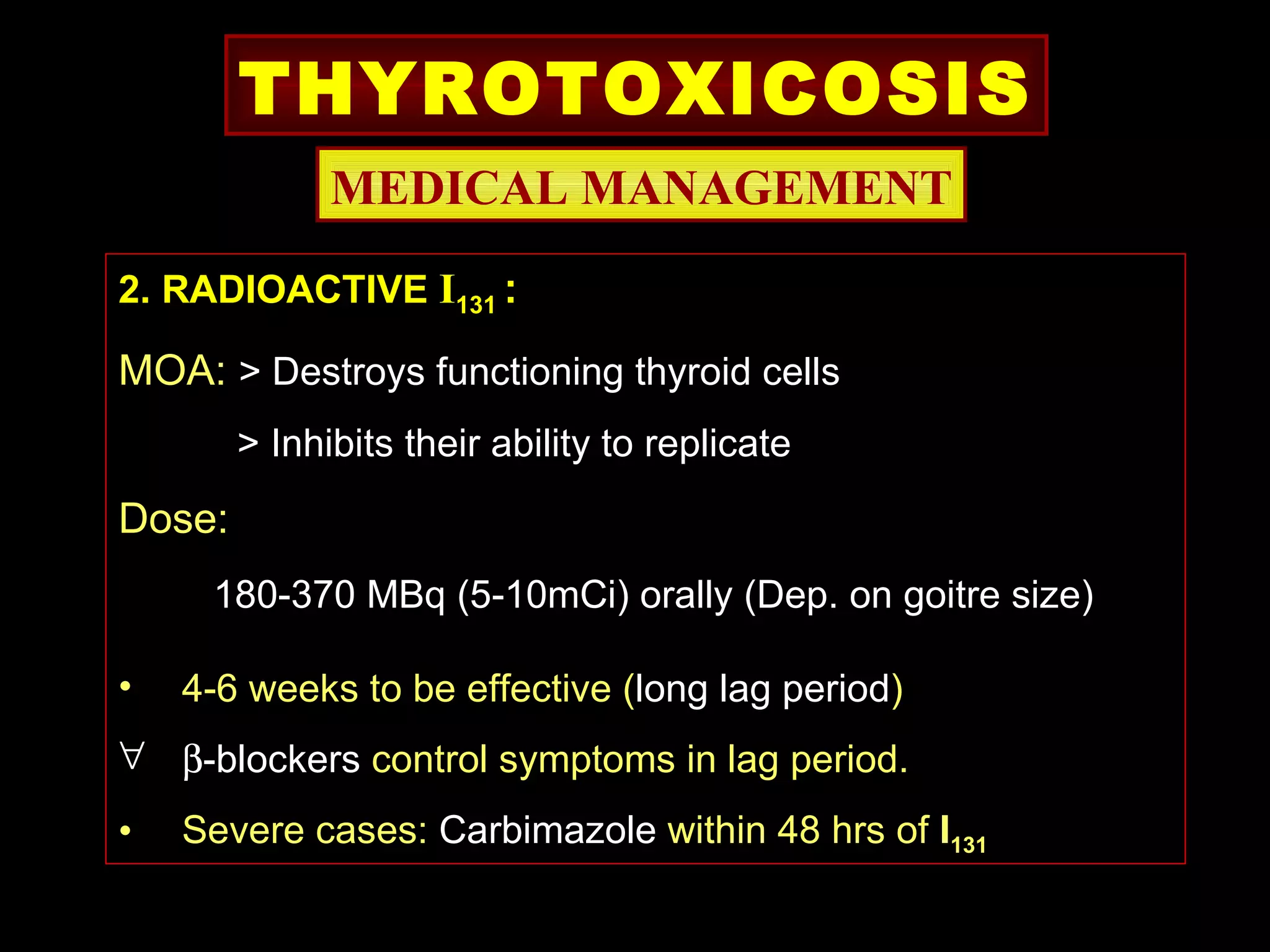
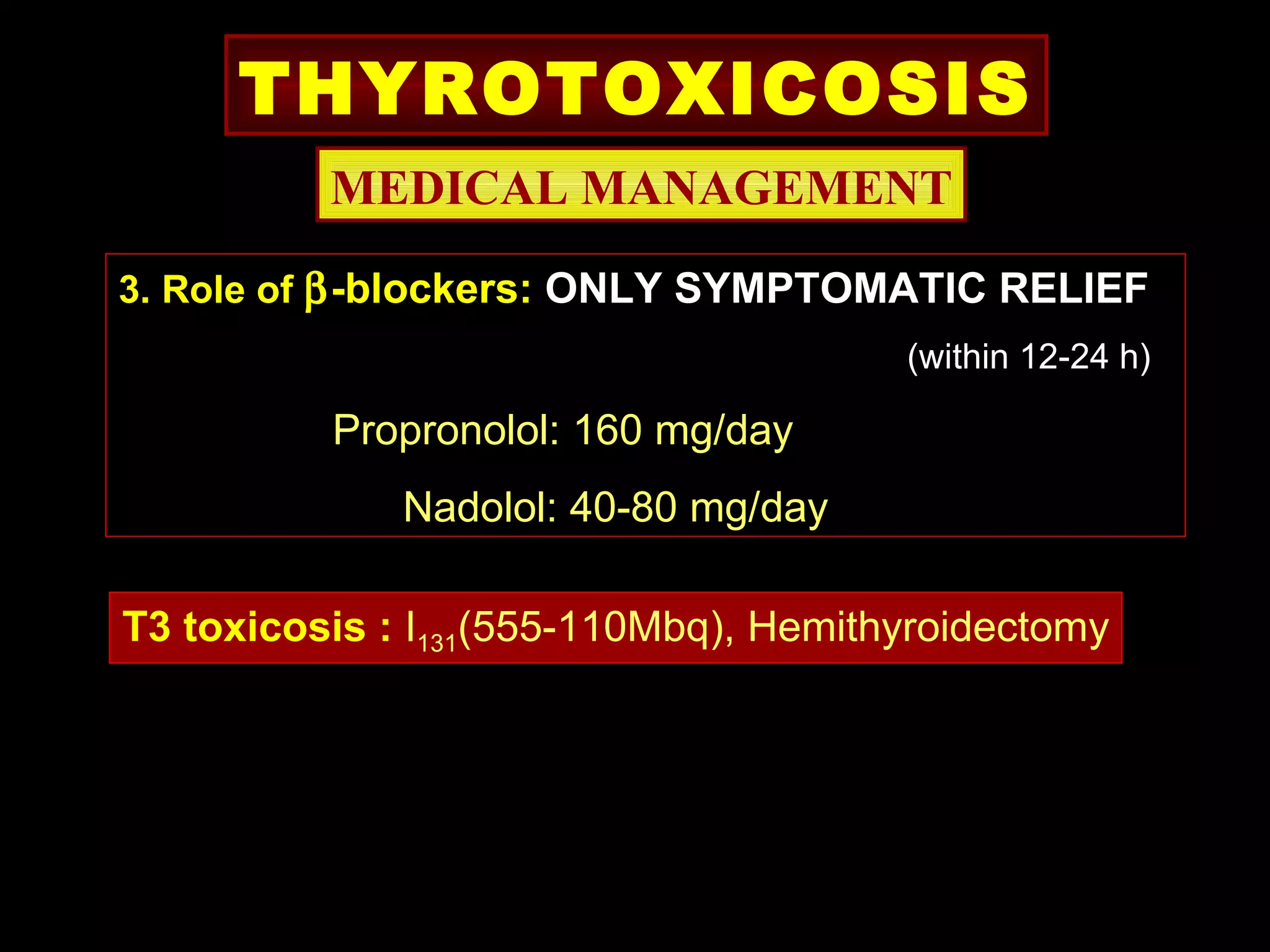
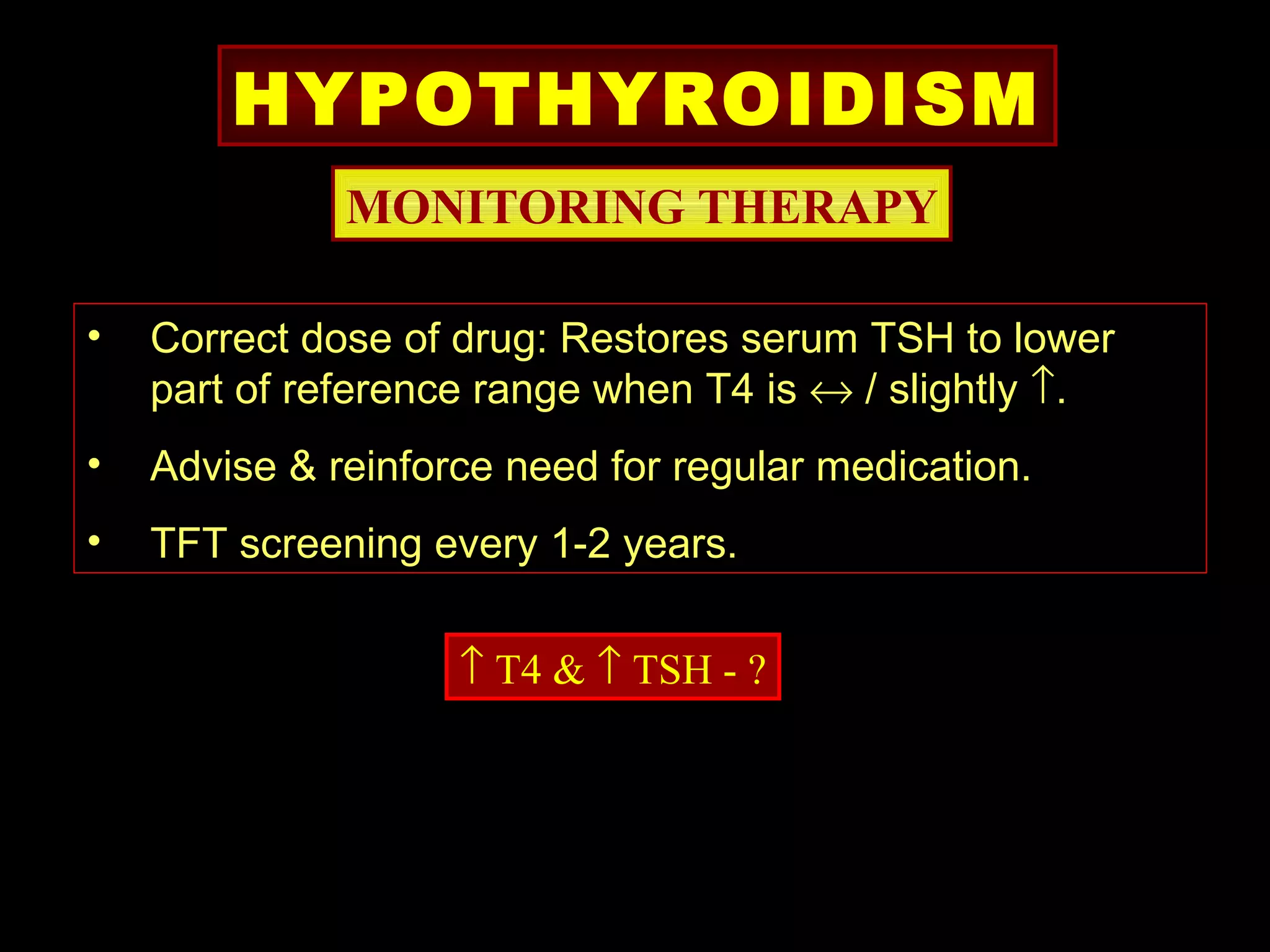
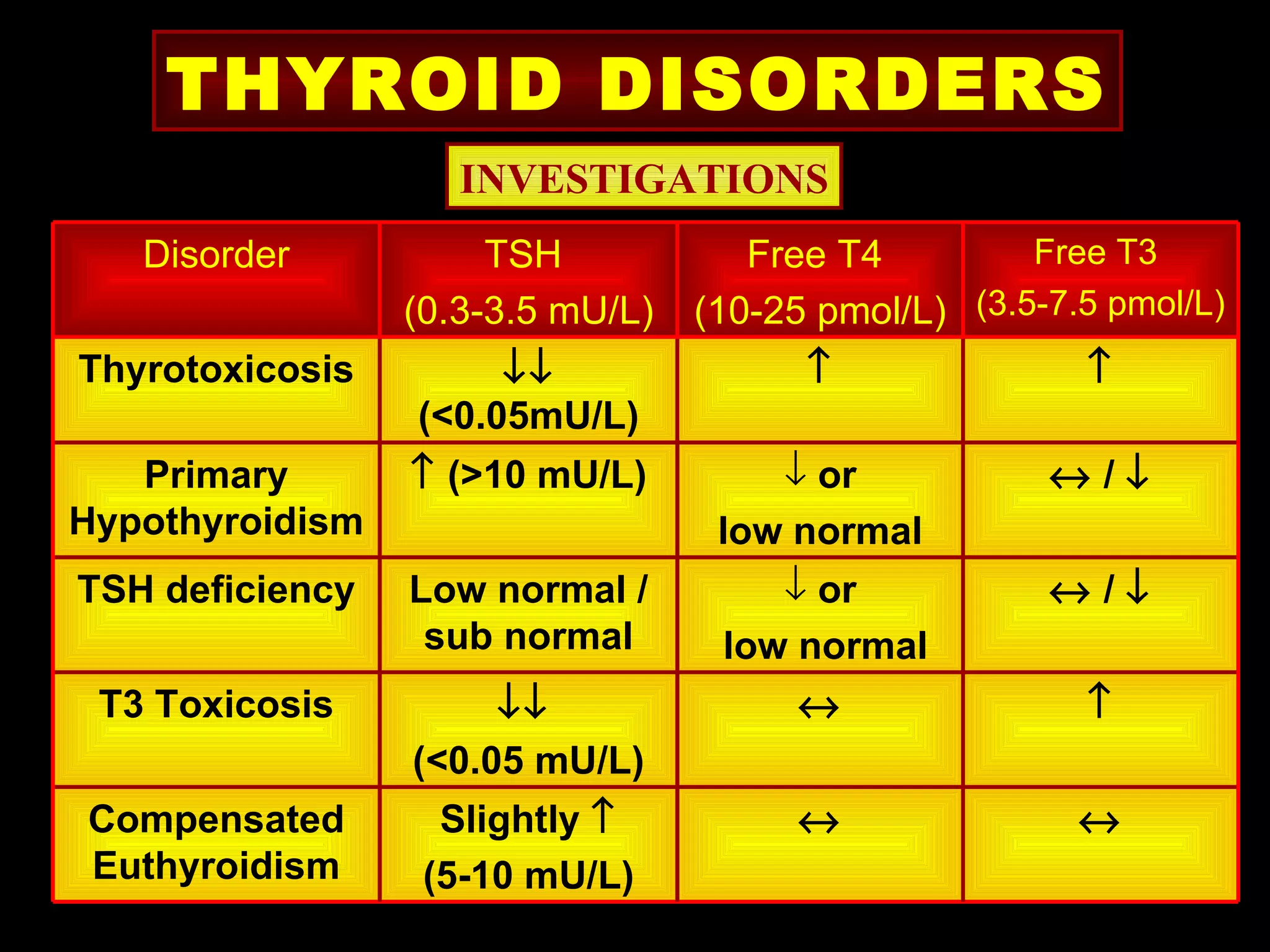
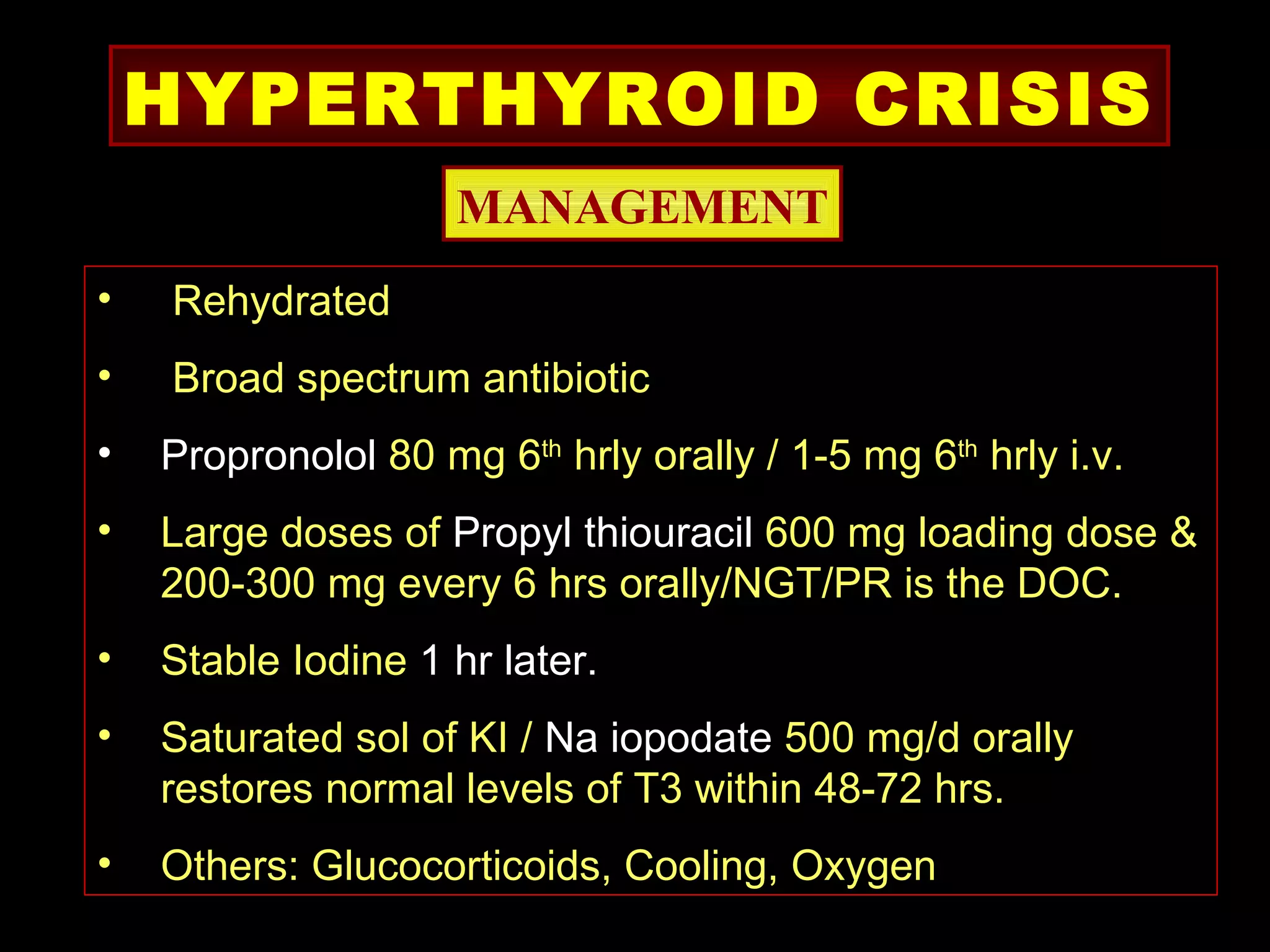
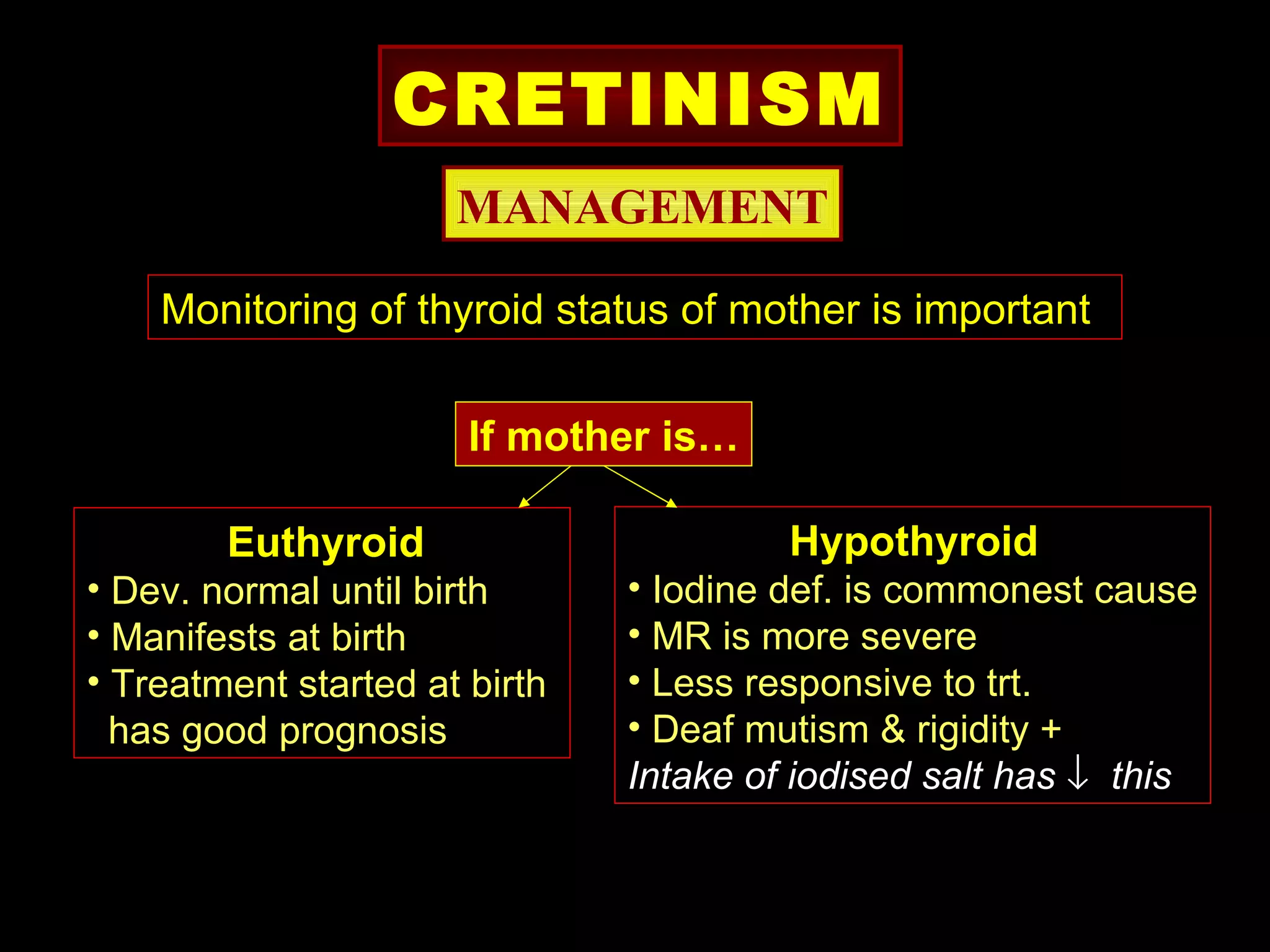
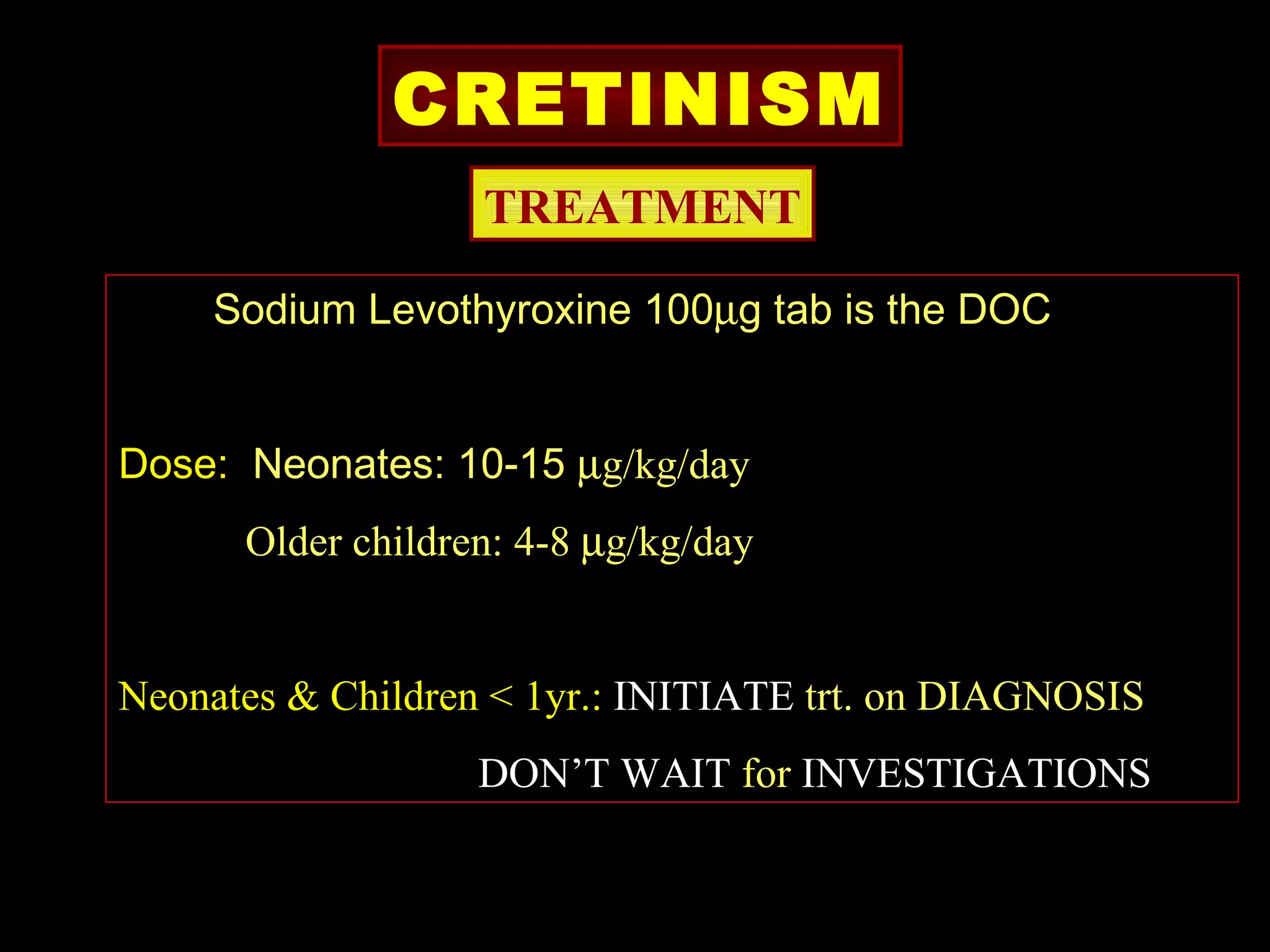
This document discusses various thyroid disorders including thyrotoxicosis, hypothyroidism, thyroid disease complicating pregnancy, and medical emergencies related to thyroid disease. Key points include: 5% of the world population suffers from thyroid disease; congenital hypothyroidism is one of the most common causes of preventable mental retardation worldwide; thyrotoxicosis is defined as excess thyroid hormone levels and its main causes are Graves' disease and multinodular goiter; hypothyroidism is commonly caused by iodine deficiency or Hashimoto's thyroiditis; and medical emergencies related to thyroid disease include thyrotoxic crisis characterized by high fever and hypothyroidism coma which has a high mortality