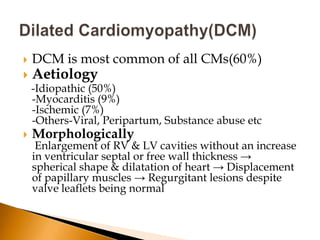
This document discusses dilated cardiomyopathy (DCM), the most common type of cardiomyopathy. It provides details on:
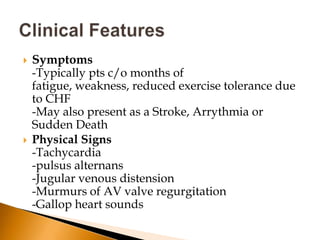
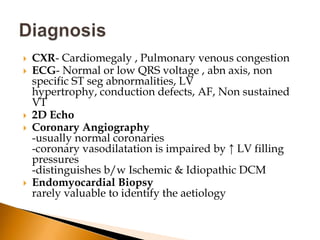
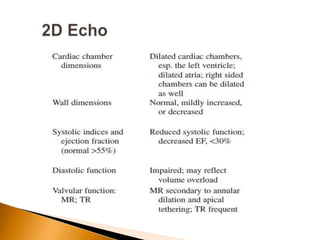
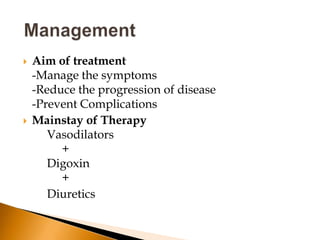
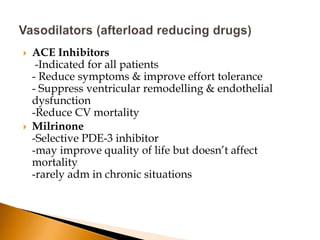
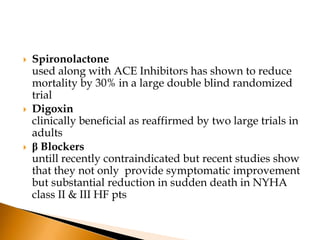
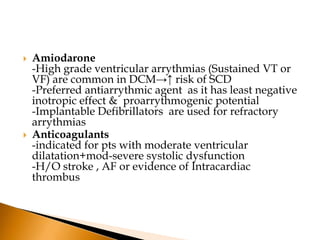
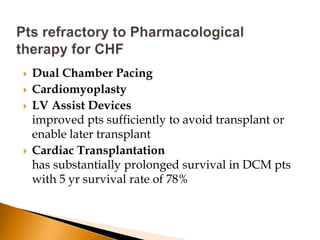
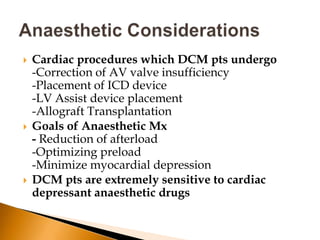
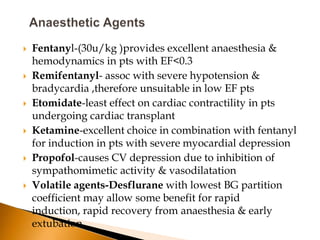
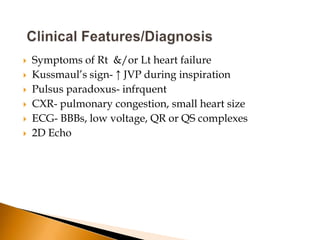
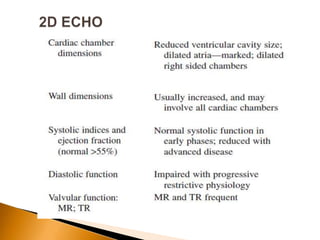
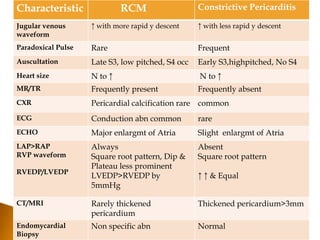
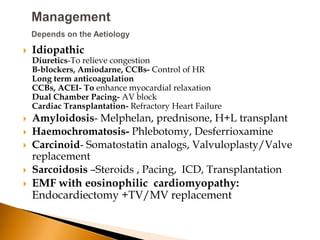
1) The causes, symptoms, signs, diagnostic tests and goals of treatment for DCM. The mainstay of therapy includes vasodilators, digoxin and diuretics.
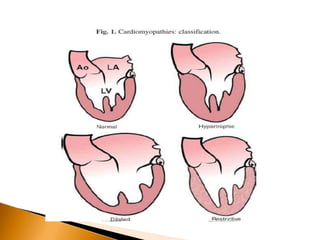
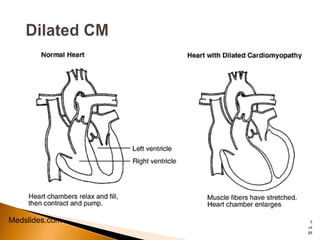
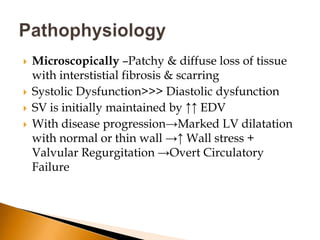
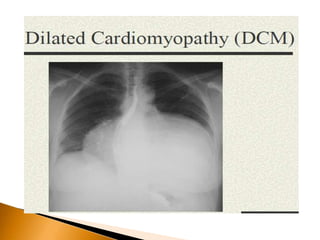
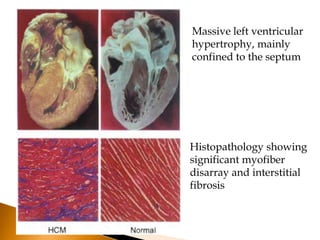
2) The morphological and microscopic features of DCM which involve enlargement and spherical dilation of the heart chambers.
3) Disease progression can lead to marked left ventricular dilatation and circulatory failure if left untreated. Management aims to relieve symptoms and slow progression.