Hypertrophic cardiomyopathy (HCM) is a genetic heart condition characterized by thickened heart muscle. It is caused by mutations affecting proteins in the heart's muscle cells. Symptoms range from none to heart failure, chest pain, fainting, and arrhythmias. Diagnosis is made through echocardiogram, which shows thickened heart muscle and sometimes left ventricular outflow tract obstruction. Treatment involves medications to reduce symptoms and surgery to relieve outflow tract obstruction if medications do not help.





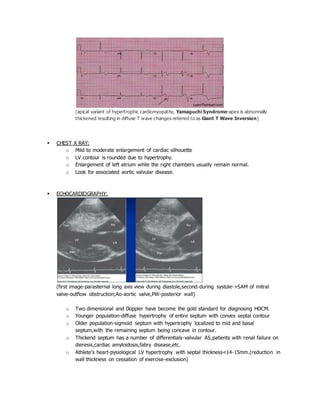
![o 2D echo-presence and severity of LVOTobstruction-indicated most commonly by systolic
anterior movement of the mitral valve with systolic open ventricular cavity.(obstruction
may be basal[classical],may extend to involve chordal apparatus or maybe mid
ventricular[papillary muscle inv.]).
o Doppler studies-high velocity “dagger shaped” signals in the presence of an LVOT
obstruction.
o Doppler colour flow imaging-presence and severity of mitral regurgitation.(in HOCM,the
jet will be directed laterally and posteriorly,predominantly in mid to late systole)
OTHER DIAGNOSTIC TESTS:
o Cardiac magnetic resonance imaging
o Cardiac catheterization
o Stress testing
TREATMENT:
Importance must be given to family screening due to autosmal dominant nature of this disorder.](https://image.slidesharecdn.com/i85as98q3aj873bsx91w-signature-2338e707061b8d73ba9337ed5b015122bfde6884eb575b4715f9c53a1849561f-poli-161104185045/85/Hypertrophic-cardiomyopathy-7-320.jpg)
