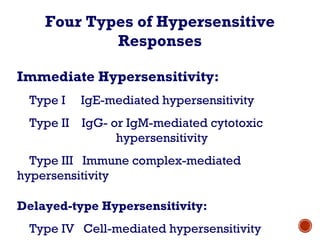
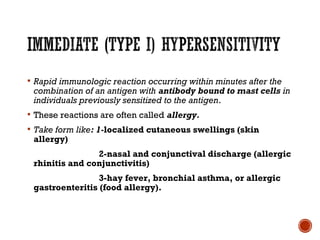
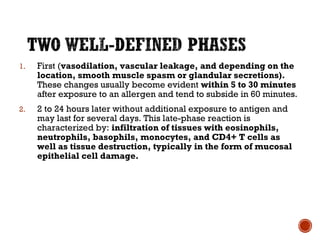
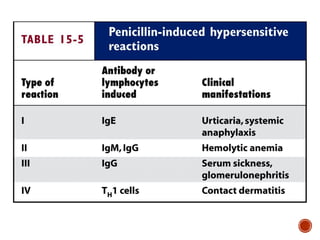
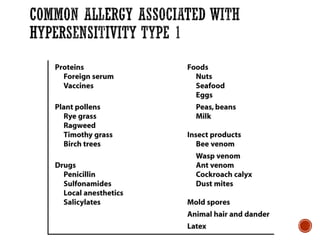
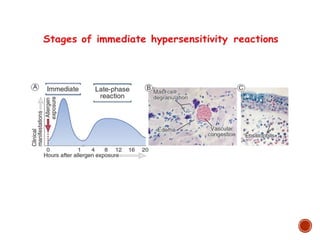
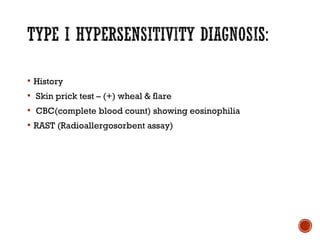
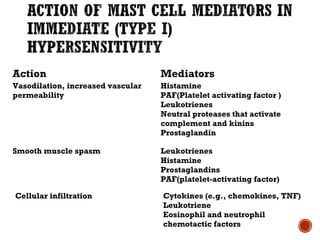
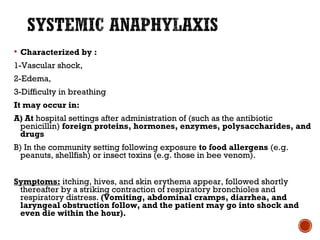
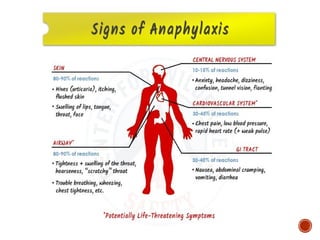
Hypersensitivity reactions are inappropriate immune responses to antigens rather than heightened responses. There are four main types: Type I immediate hypersensitivity is IgE-mediated and causes rapid allergic reactions through mast cell degranulation and the release of histamine; Type II involves IgG or IgM antibodies causing cytotoxicity; Type III occurs via immune complex deposition; Type IV is cell-mediated hypersensitivity. Symptoms range from mild rhinitis and skin reactions to life-threatening anaphylaxis.