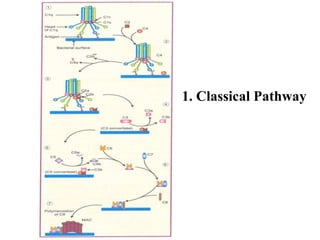
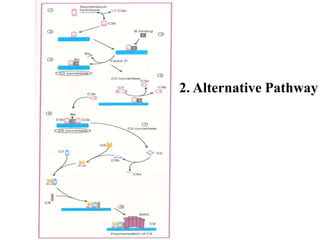
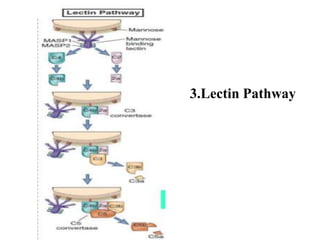
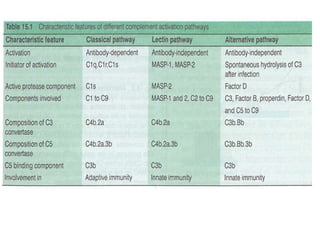
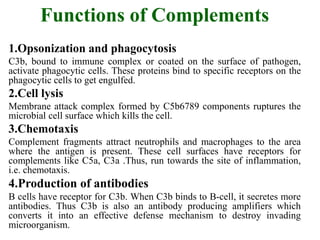
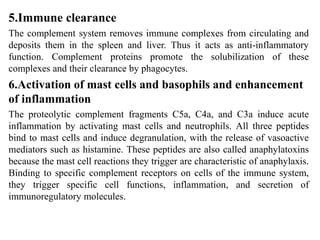
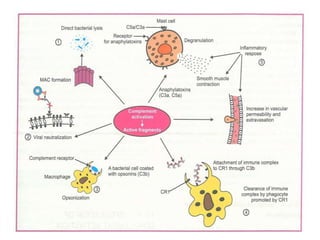
The document summarizes the complement system. It is part of the immune system and consists of proteins that interact in a regulated cascade to eliminate pathogens and damaged cells. There are over 20 complement proteins that are activated via the classical, alternative, or lectin pathways and work in both innate and adaptive immunity. The complement system opsonizes pathogens, causes cell lysis, promotes inflammation, and clearance of immune complexes. Deficiencies or dysregulation of complements can cause diseases.


![REFERENCES
• Owen.J.A , Punt.J , Strandford.S.A and Jones.P.P,[2013],
Kuby-Immunology, 7th Edn , W.H.Freeman and company.
New York,Pp-692
• Male.D and Brostoff.J, Immunology, 8th Edn, published
by Dianne zark International Pvt Ltd,Pp-455
• Rabson.A , Ivan.M.R , Delves.P.J. Medical Immunology,
2nd Edn, Blackwell publishers. USA,Pp-213
• Javetz , Melnick and Adelberg’s [2013] Medical
Microbiology,26th Edn, McGrawHill publications.Pp-823
• Murphy.K and Weaver.C, Immunology 9th Edn,
Published by Garland science Taylor .New York, Pp-855](https://image.slidesharecdn.com/comp-190626174121/85/Complement-system-18-320.jpg)