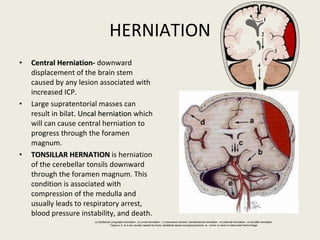
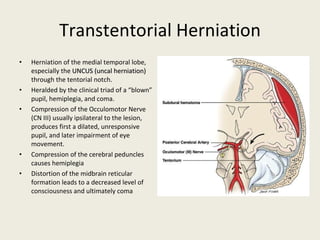
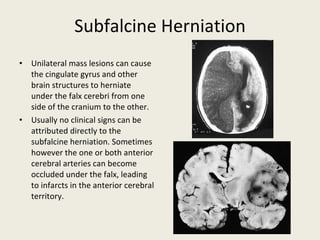
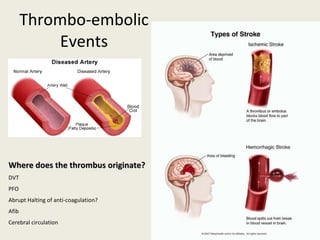
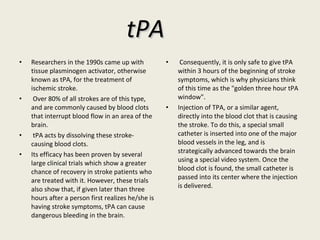
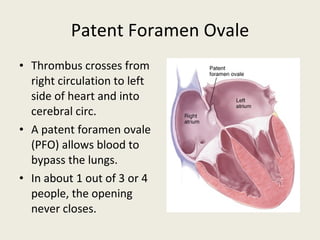
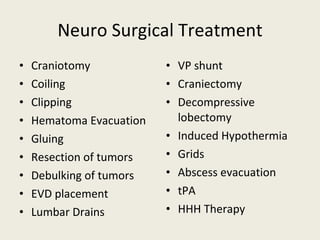
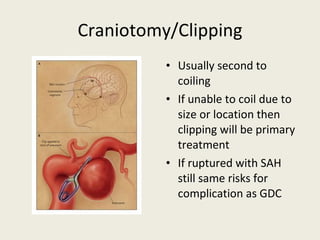
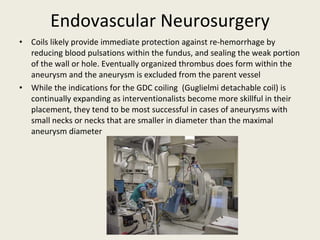
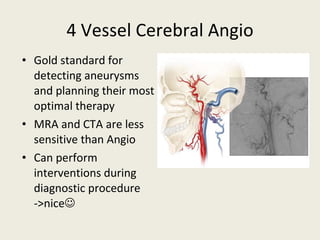
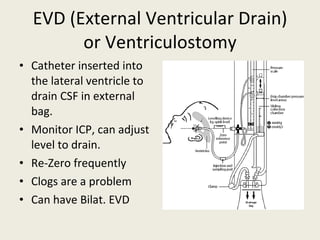
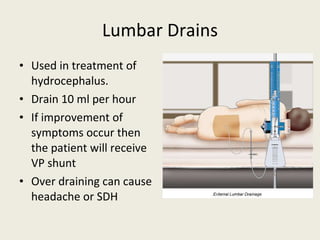
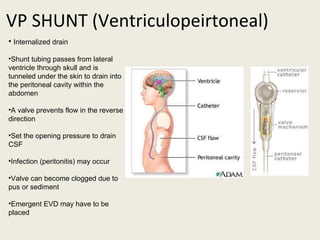
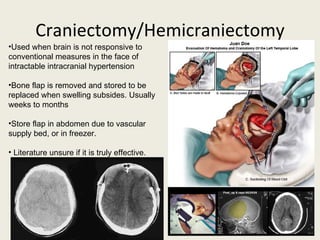
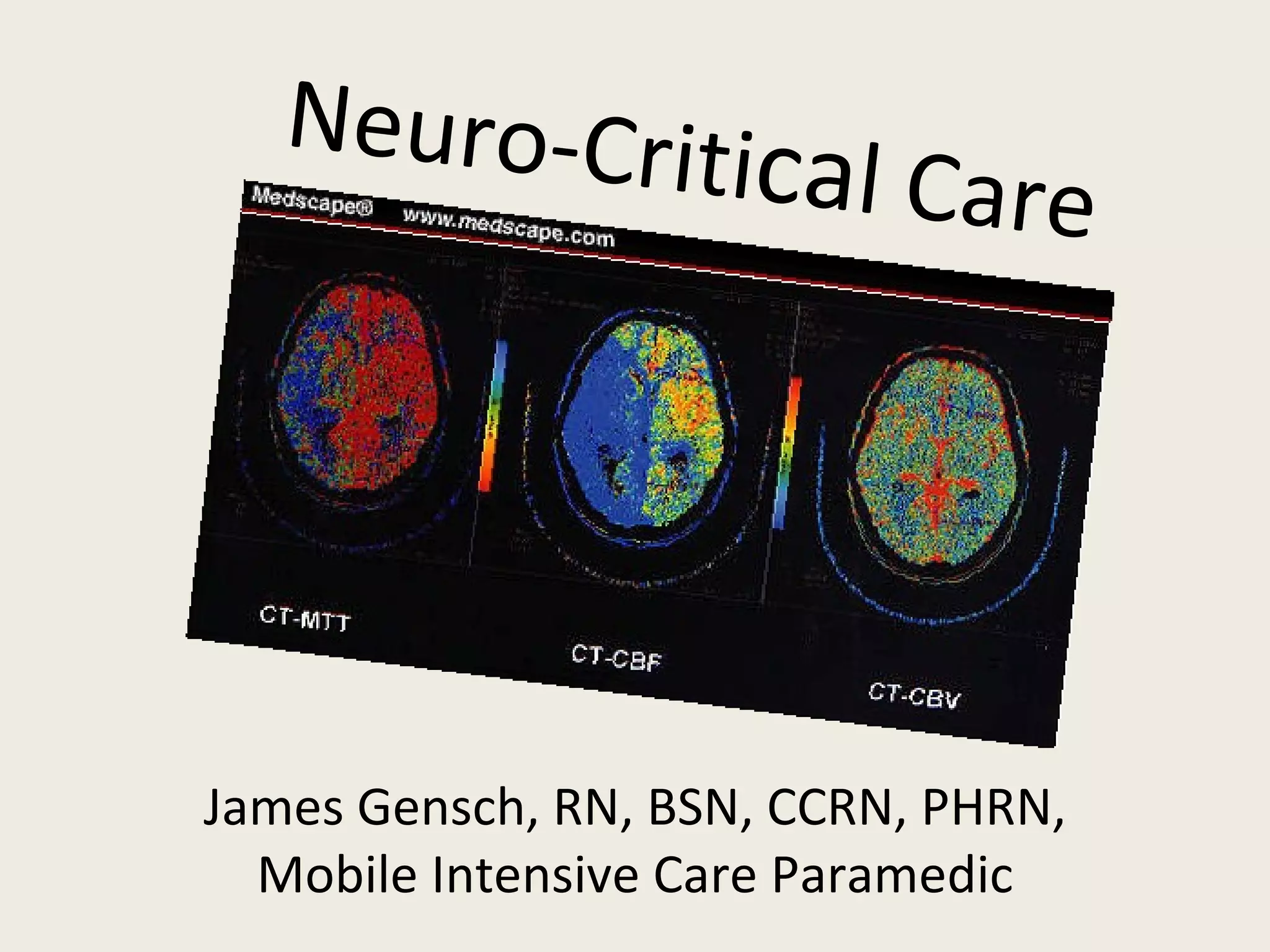
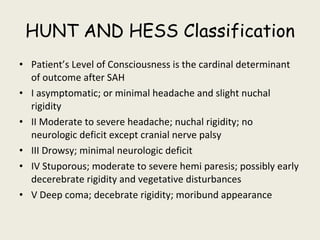
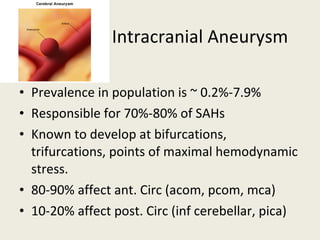
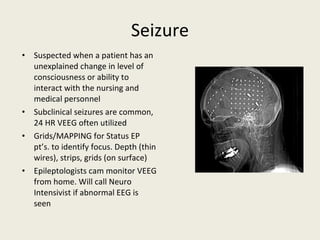
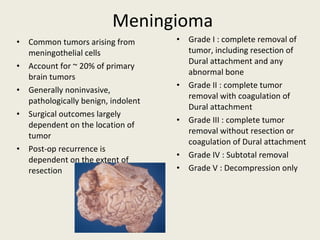
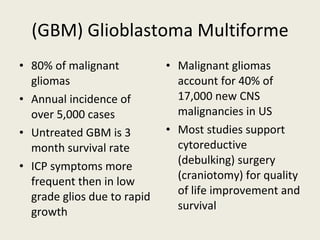
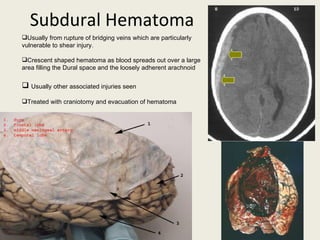
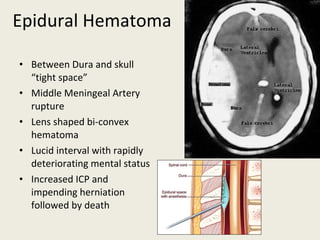
This document provides an overview of neurocritical care topics including: common neurologic emergencies like subarachnoid hemorrhage, aneurysms, seizures and tumors; classifications like Hunt and Hess for SAH; monitoring tools like ventriculostomy for ICP; treatments for increased ICP like hyperosmolar therapy; endovascular procedures like coiling; and surgical treatments including craniotomy, clipping and ventricular shunts.
![ICP Cerebral Perfusion Pressure (CPP=mean arterial pressure [MAP]-ICP) 55mmHg or greater is USUALLY adequate Higher ICP from injury will require higher CPP to maintain cerebral blood flow (CBF) Ventriculostomy is the gold standard for monitoring ICP Zeroed at the level of Circle of Willis](https://image.slidesharecdn.com/neurocriticalcare-12984917855086-phpapp02/85/Neuro-Critical-Care-15-320.jpg)