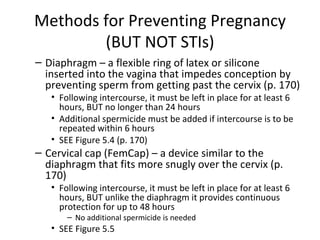
The document discusses various methods of contraception including barrier methods like condoms and diaphragms, hormonal methods like birth control pills and implants, fertility awareness techniques, intrauterine devices (IUDs), and surgical sterilization methods. It provides details on effectiveness, proper use, side effects, and limitations for preventing pregnancy and STIs for each method.