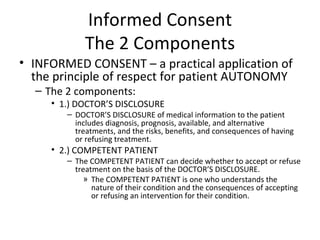
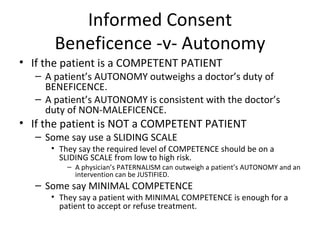
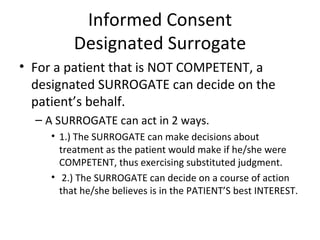
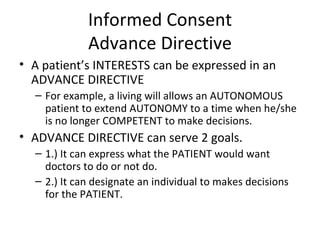
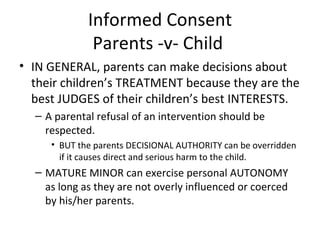
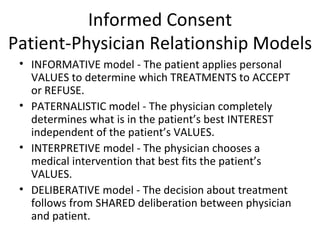
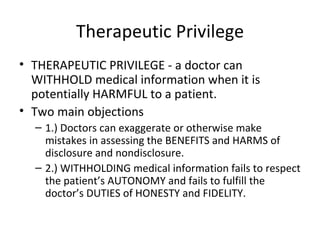
The document discusses key concepts in biomedical ethics related to the patient-doctor relationship, including informed consent, competence, autonomy, beneficence, and confidentiality. Informed consent requires doctors to disclose information to competent patients and for patients to decide on treatment. Surrogates can make decisions for incompetent patients. Advance directives allow autonomous patients to express future treatment preferences. While parents generally decide on children's treatment, mature minors can exercise autonomy. Models of the patient-doctor relationship include informative, paternalistic, interpretive, and deliberative. Therapeutic privilege and confidentiality also factor into ethical considerations.