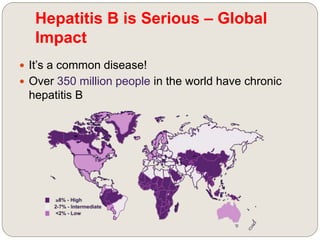
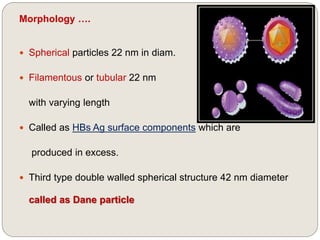
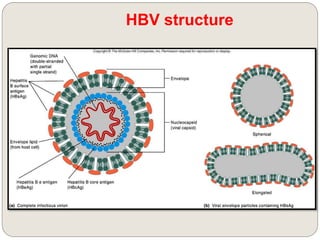
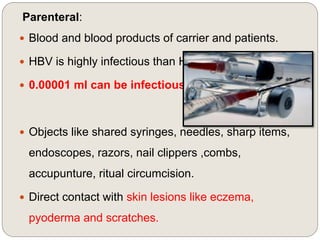
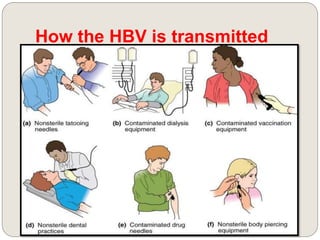
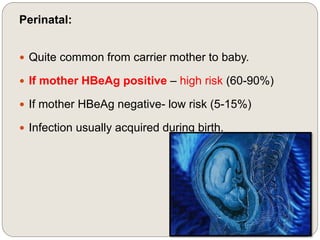
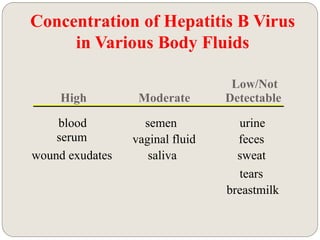
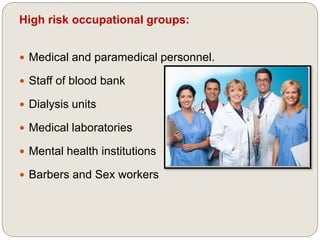
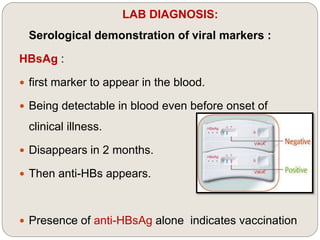
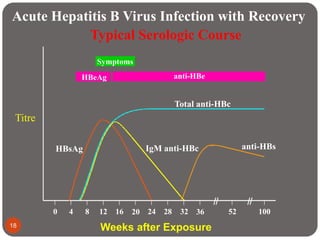
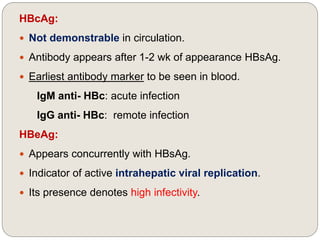
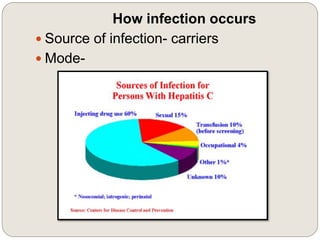
This document summarizes Hepatitis B and C. It describes that Hepatitis B is caused by the HBV virus and can range from mild to chronic liver disease or cancer. Over 350 million people worldwide have chronic Hepatitis B. The virus is classified in the family Hepadnaviridae and genus Orthohepadnavirus. It is transmitted through blood, sexual contact, and from mother to child. Hepatitis C is caused by the HCV virus and transmitted through blood. There is no vaccine for Hepatitis C, but screening blood and safe injection practices can help prevent transmission.