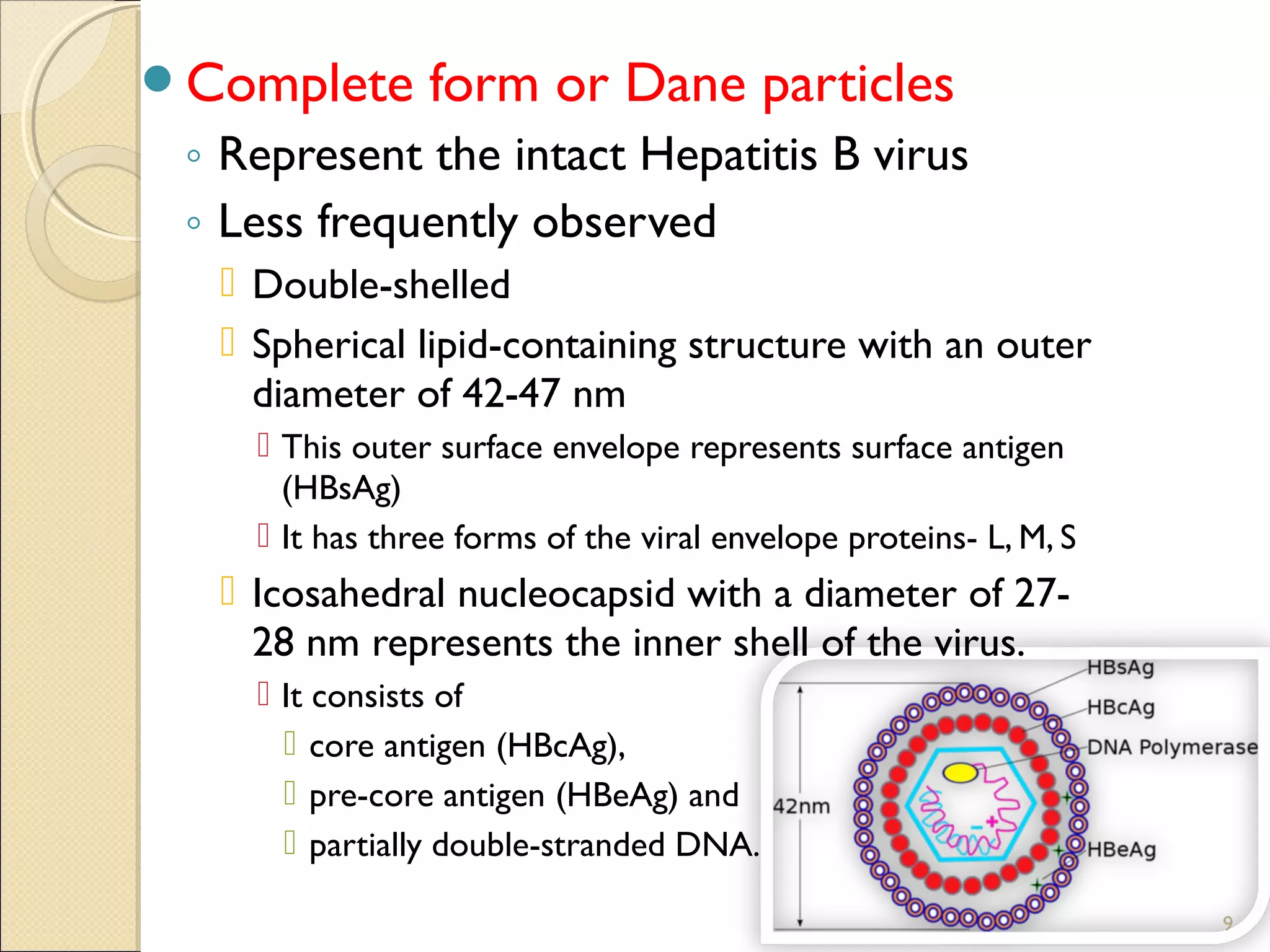
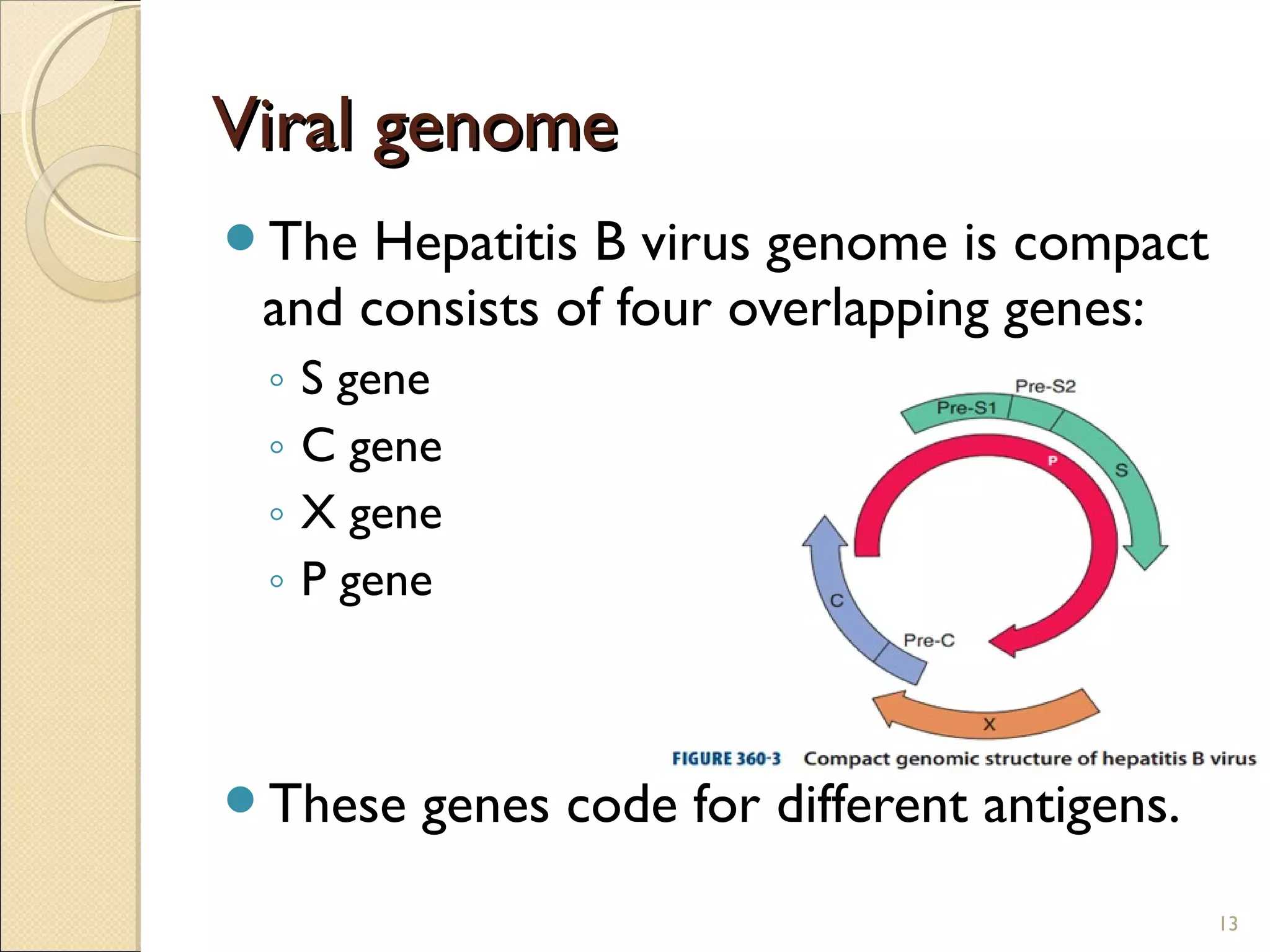
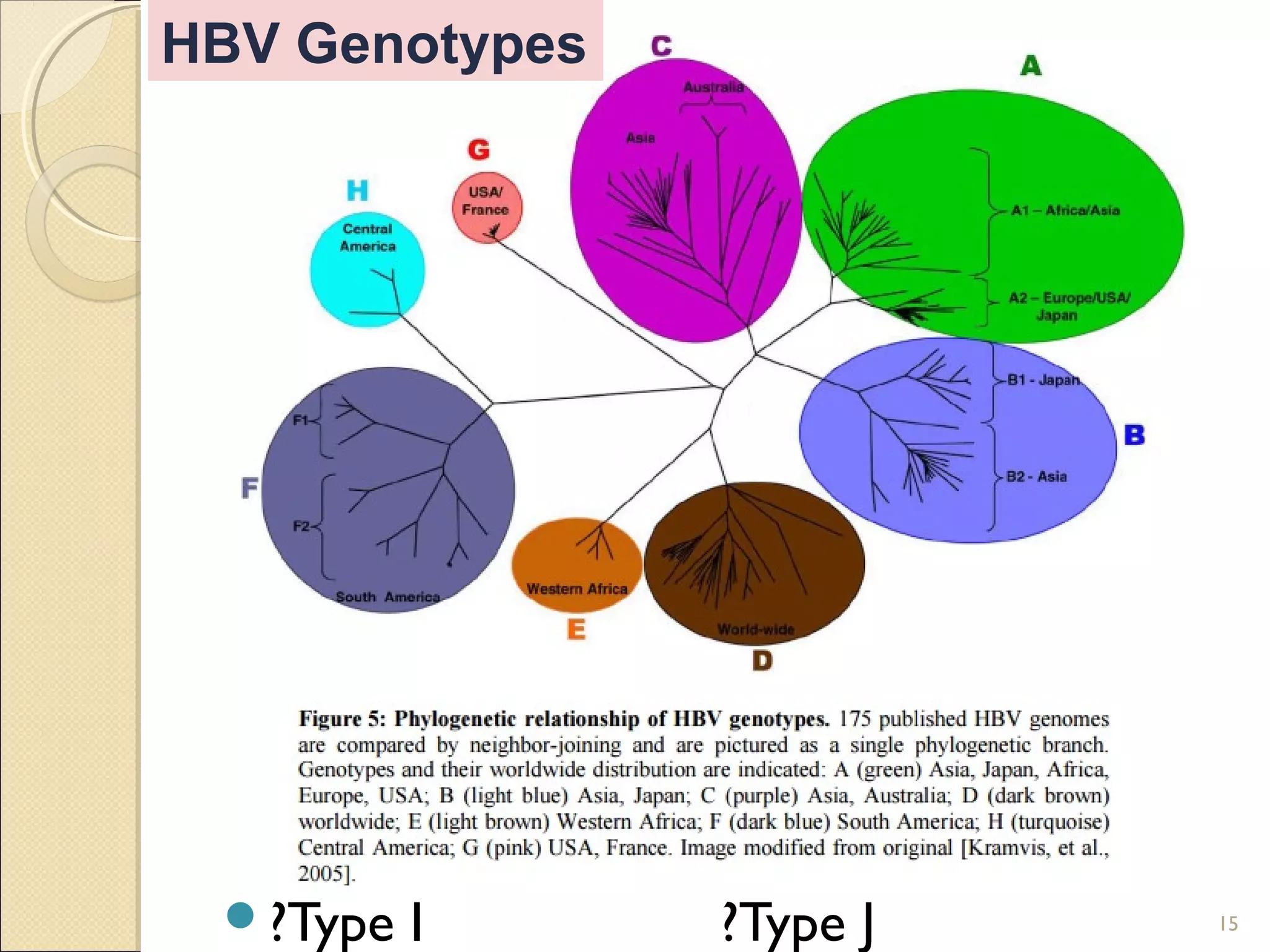
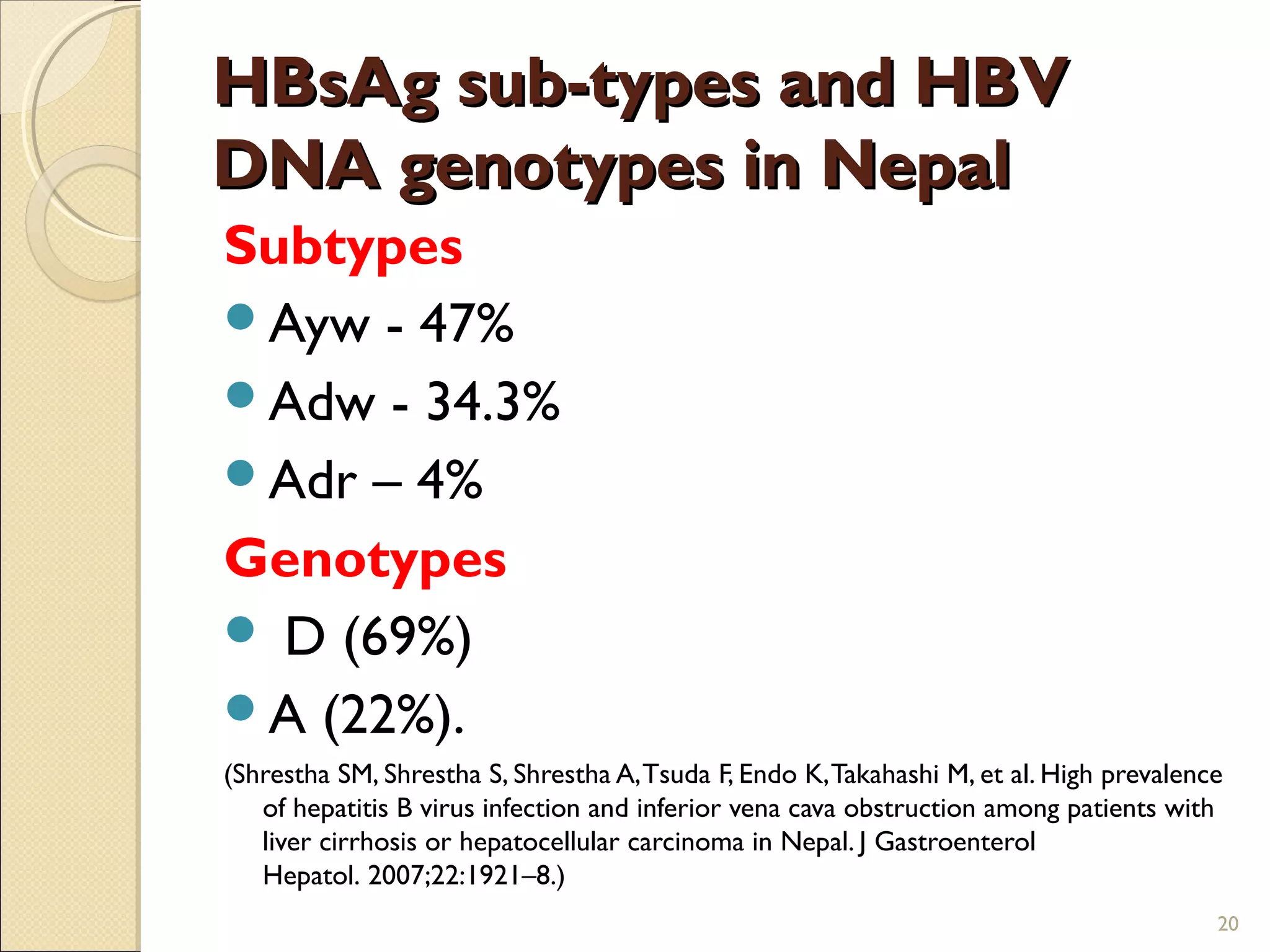
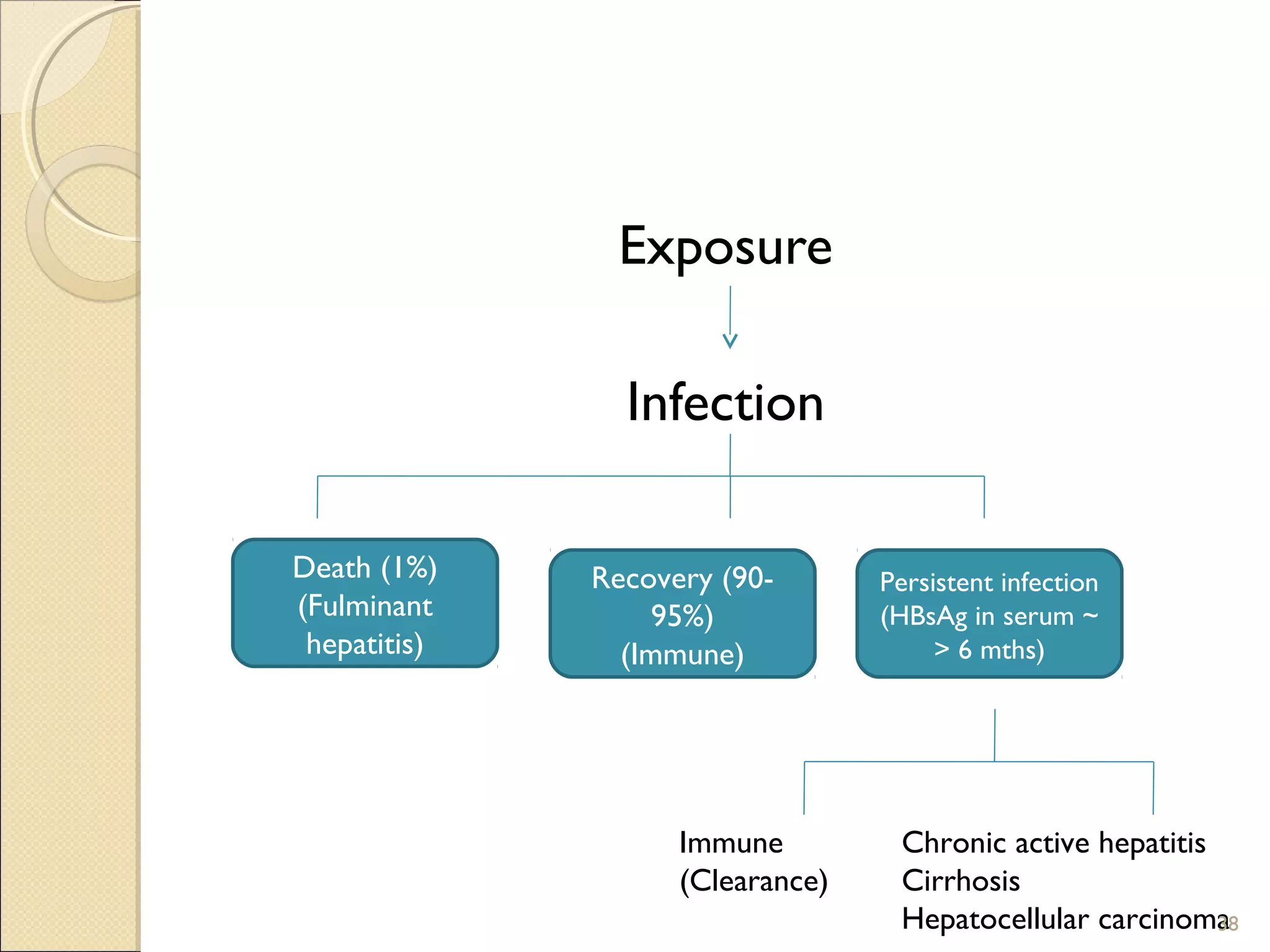
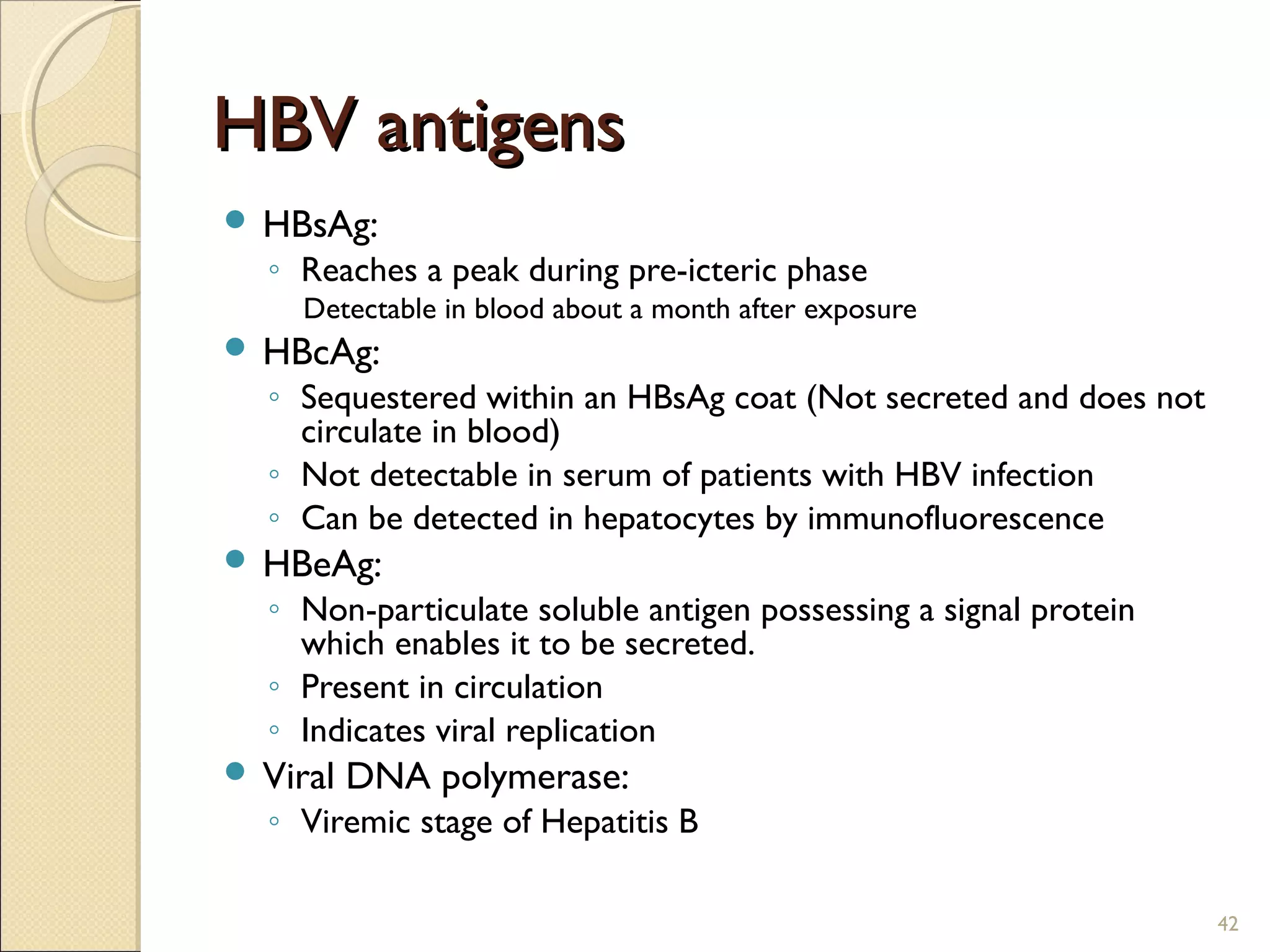
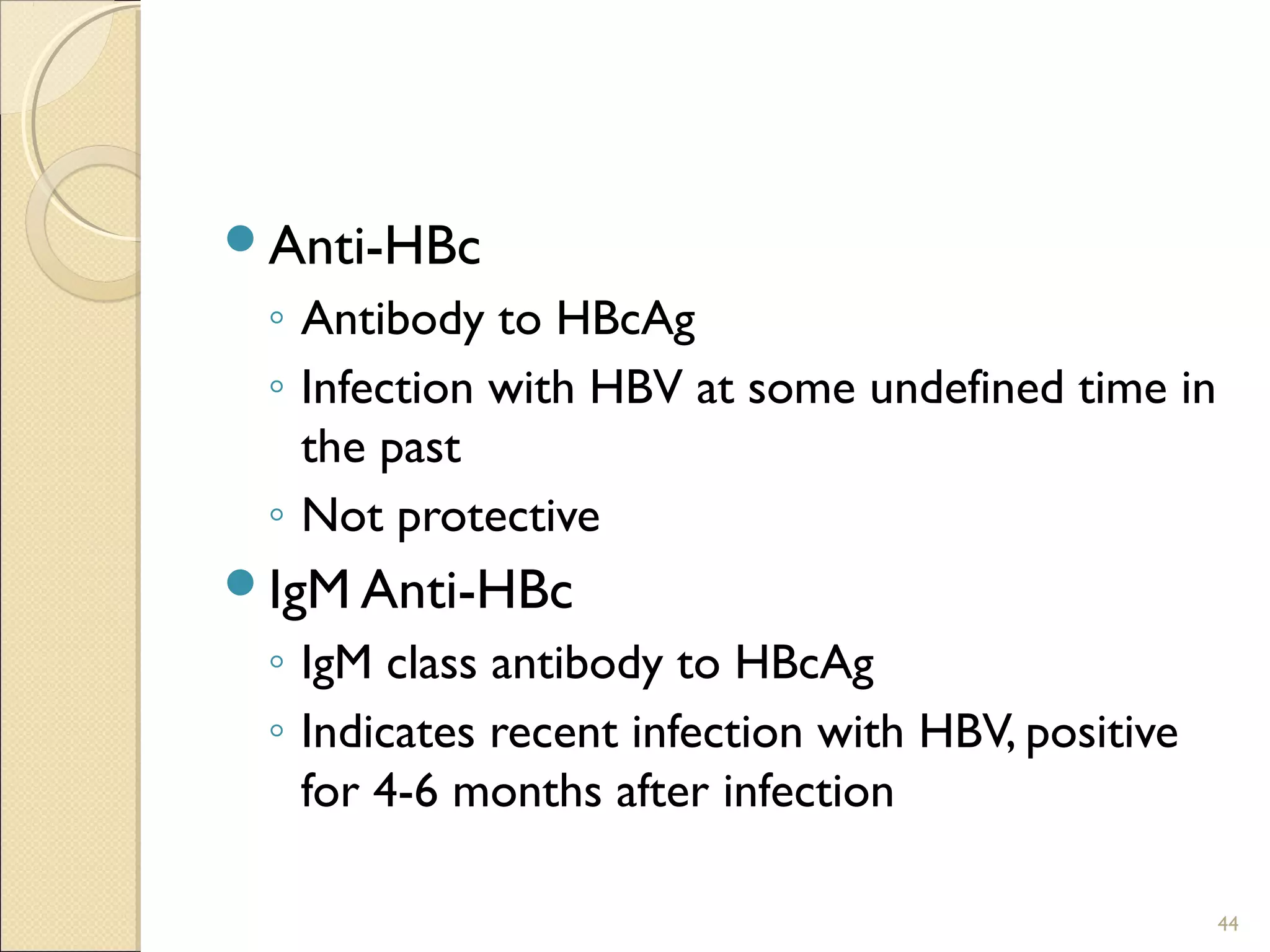
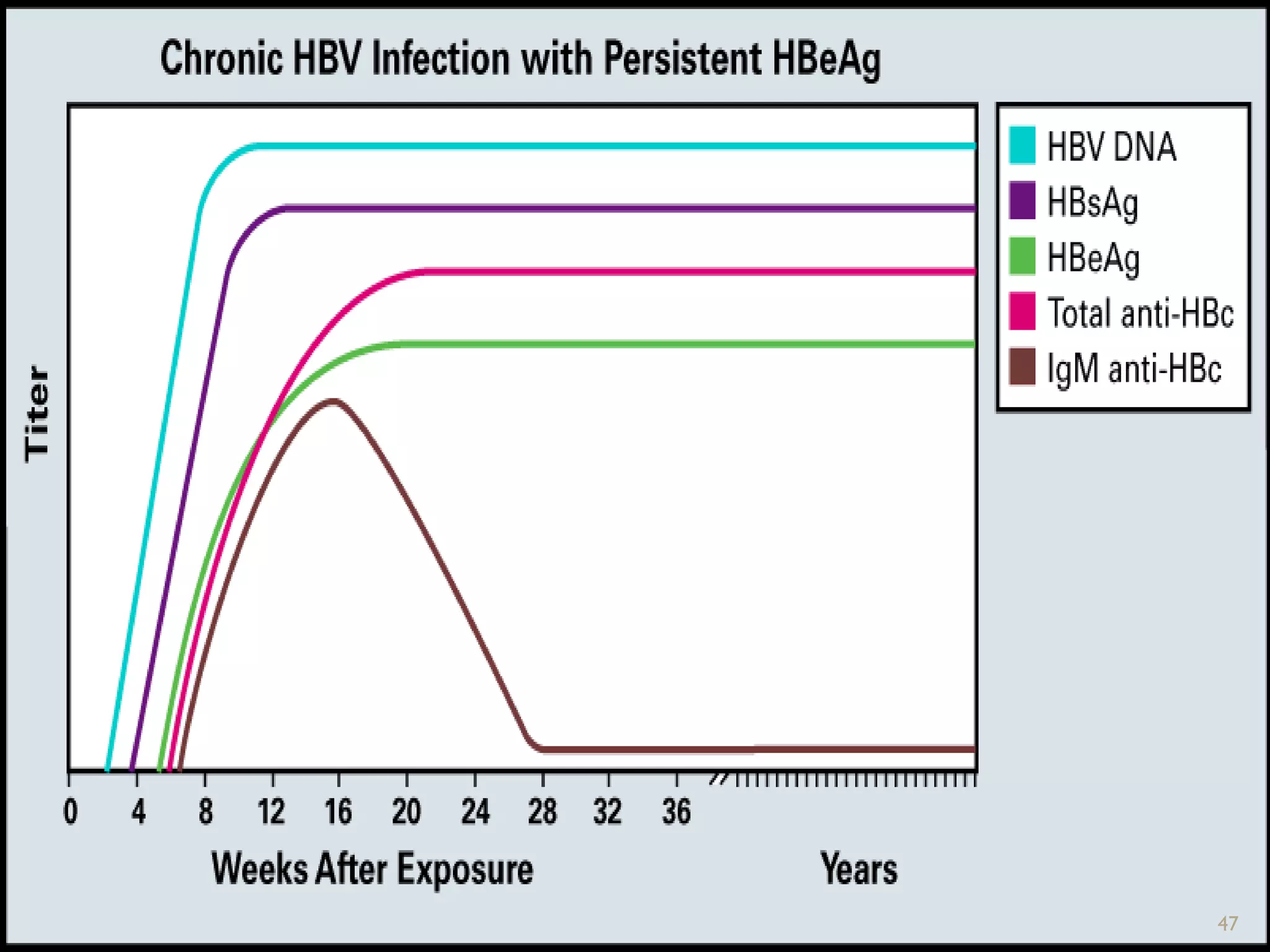
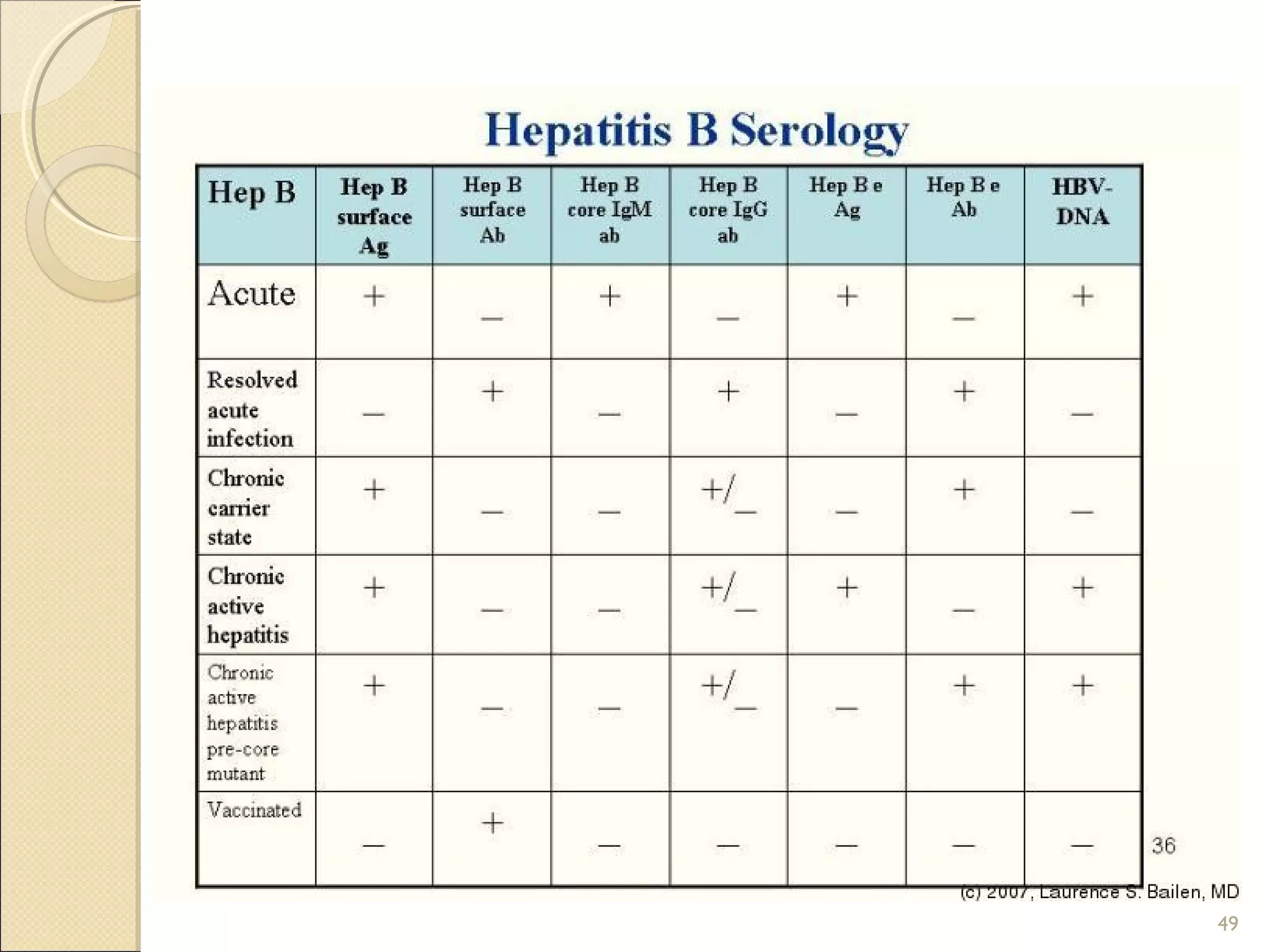
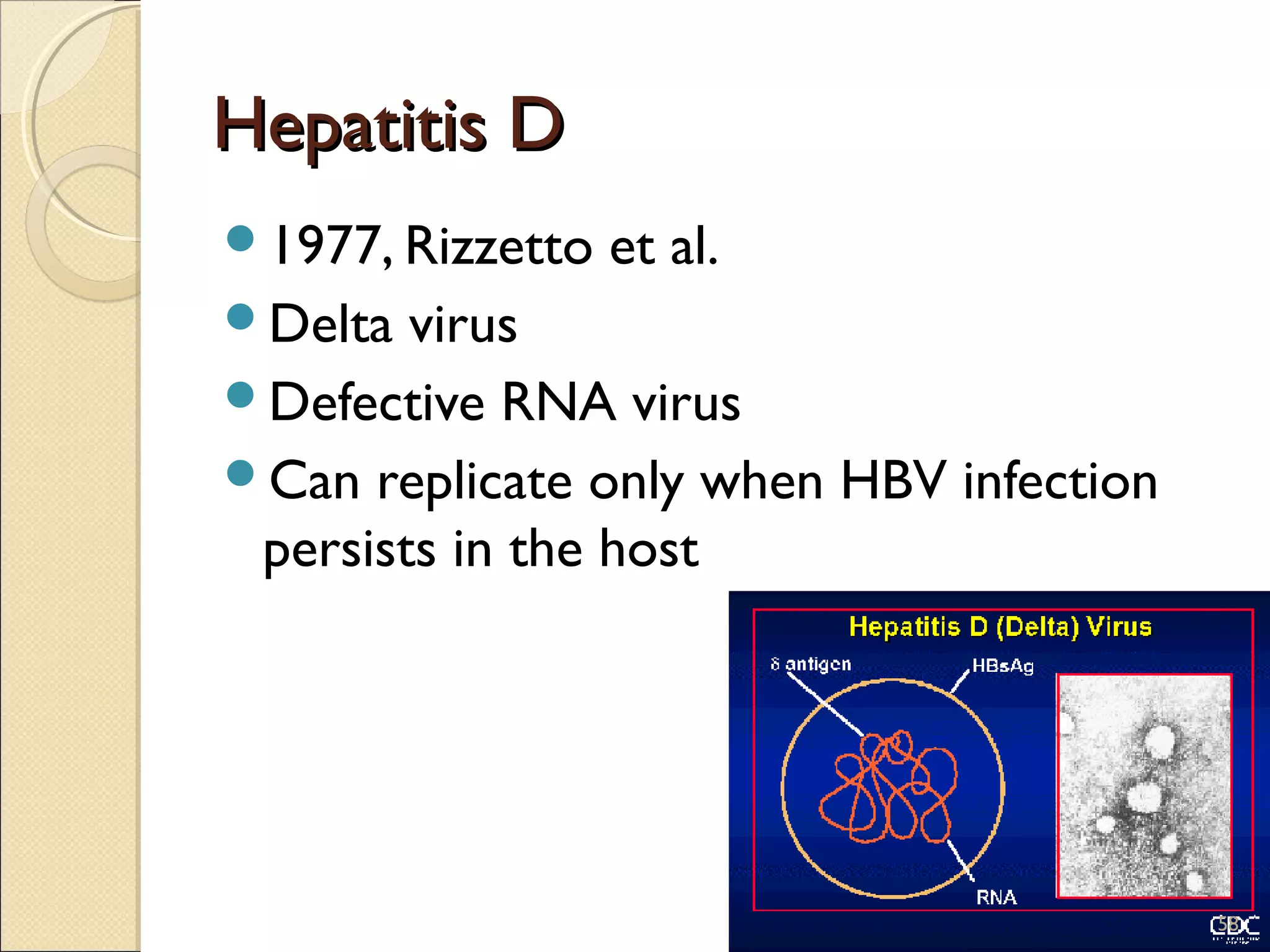
The document provides a comprehensive overview of the hepatitis B virus (HBV), detailing its morphology, viral genome, genotypes, modes of transmission, clinical features, and immunization strategies. It highlights the distinctions between different HBV genotypes and their implications for disease progression and treatment responses, as well as the relevance of various HBV antigens in diagnosis. The document also discusses the epidemiological aspects of HBV, including prevalence, risk factors, and the importance of preventive measures such as vaccination.