Hemostasis is the process by which bleeding is stopped. It involves four key mechanisms:
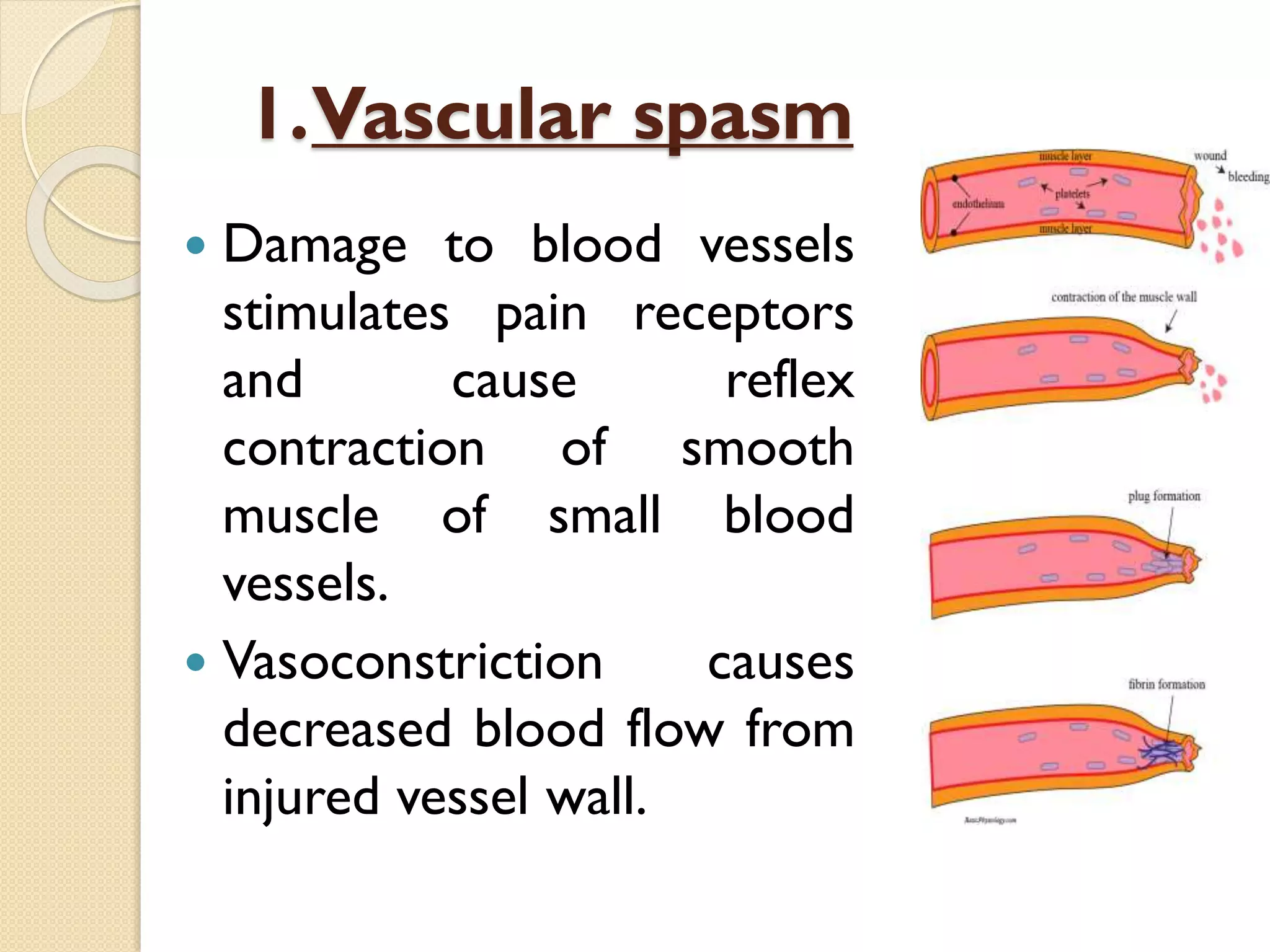
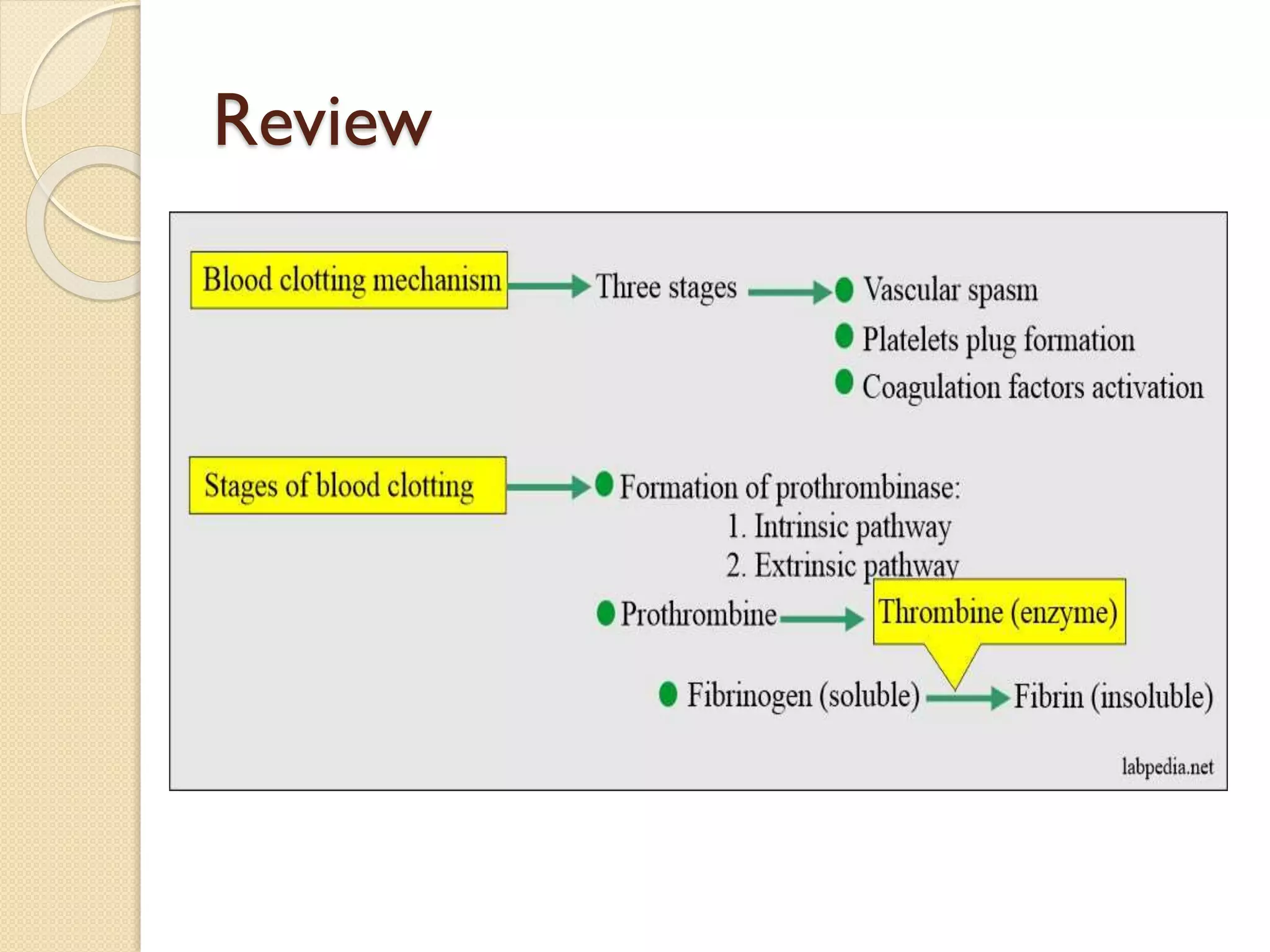
1) Vasoconstriction of blood vessels to reduce blood flow from the injury site.
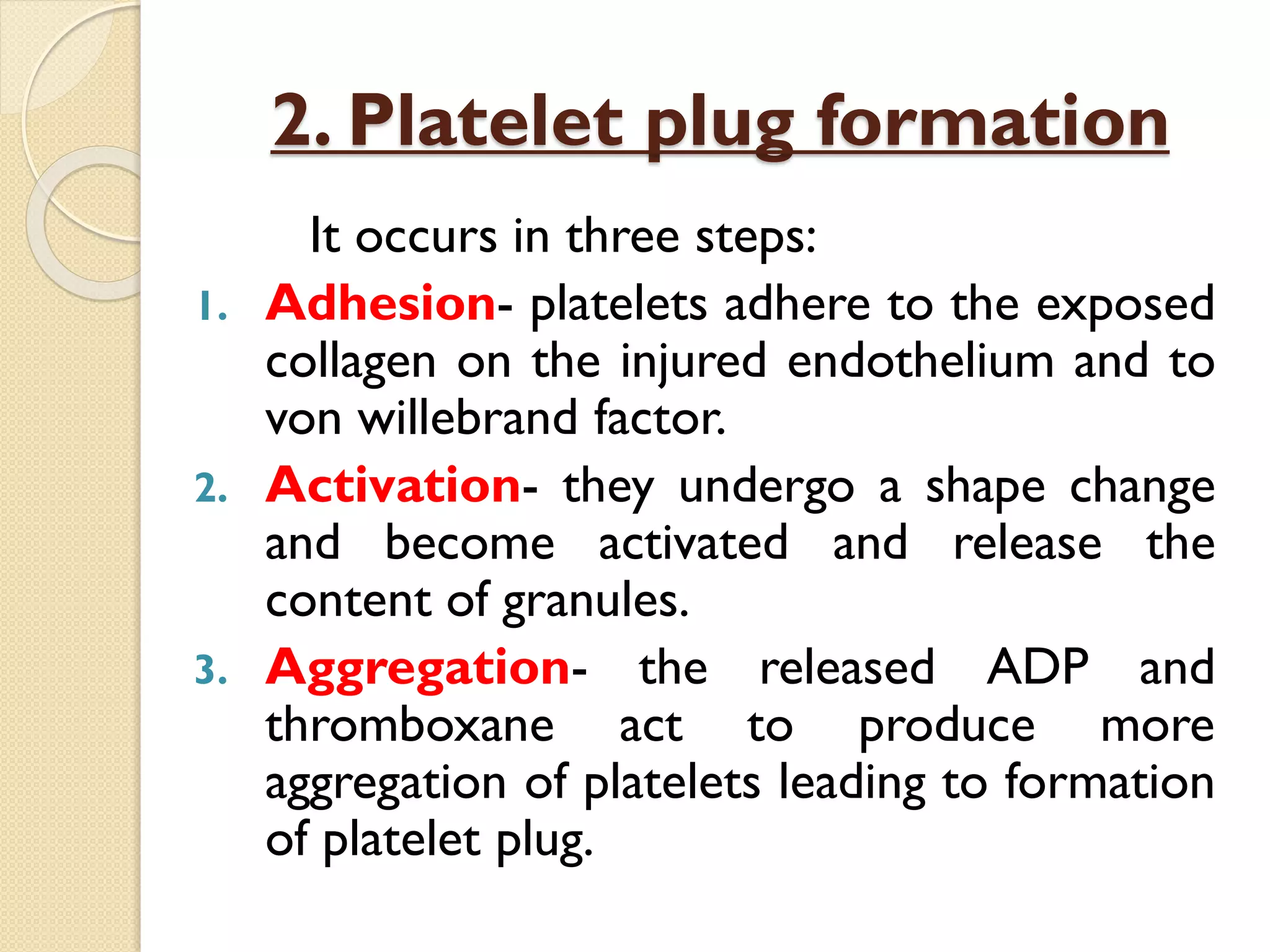
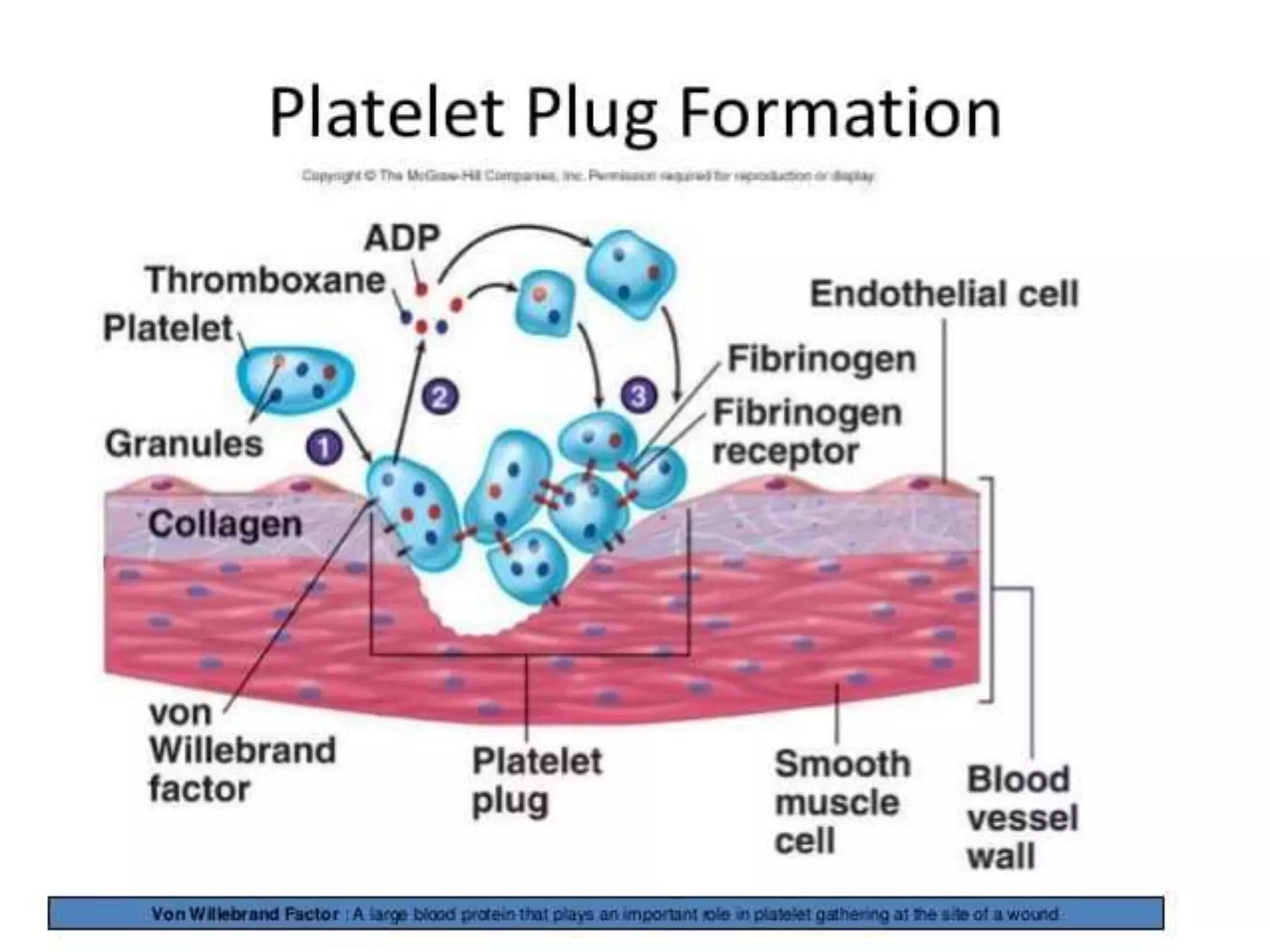
2) Formation of a platelet plug through adhesion, activation, and aggregation of platelets at the injury.
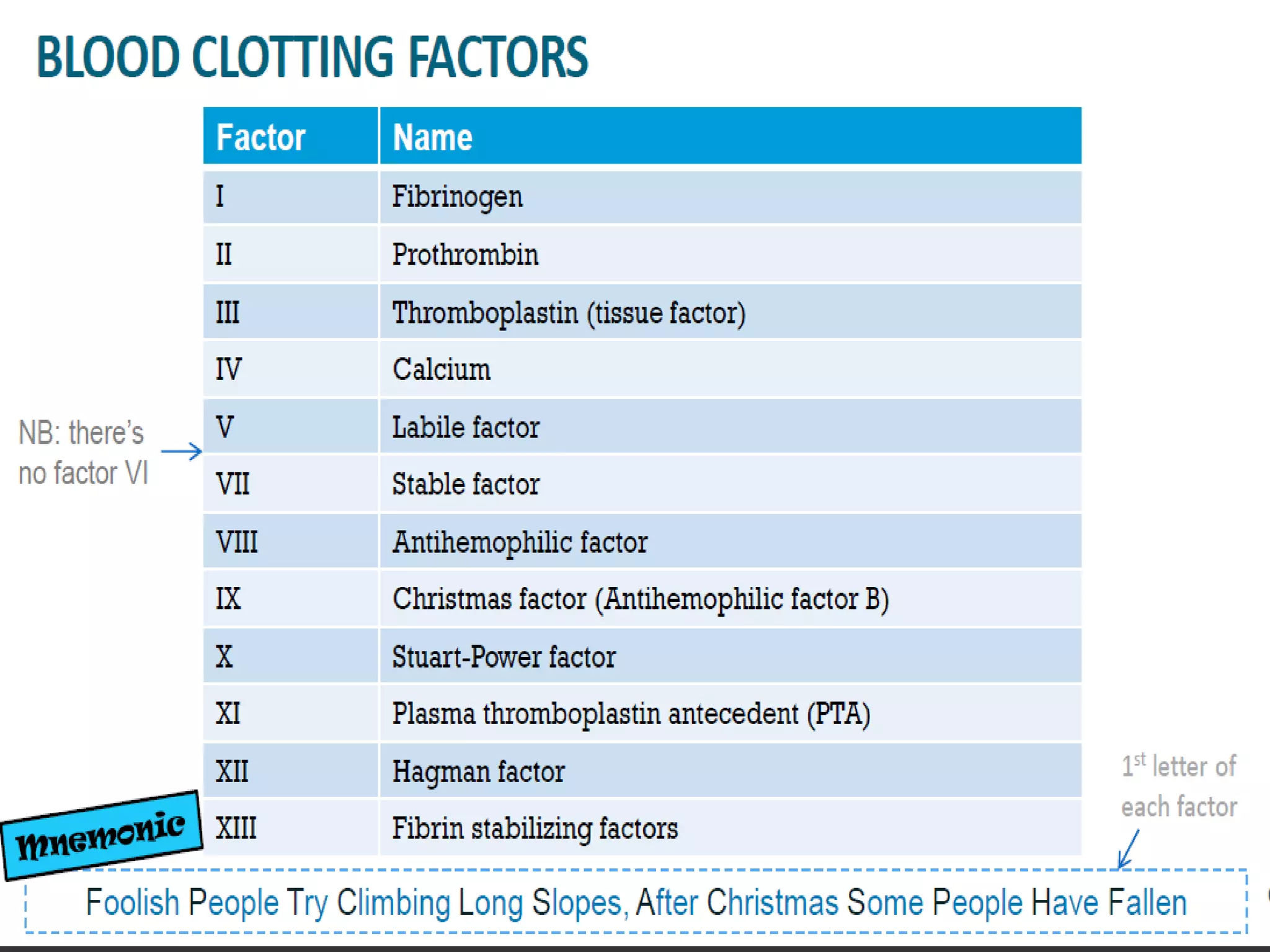
3) Coagulation of blood to form a fibrin clot from fibrinogen.
4) Later lysis of the clot through fibrinolysis to restore blood flow.